Comparison of Surgical Outcomes between Single-Use and Reusable Flexible Ureteroscopes for Renal Stone Management: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Inclusion Criteria
2.2. Search Strategy
2.3. Study Selection and Extraction
2.4. Quality Assessment
2.5. Statistical Analysis
3. Results
3.1. Eligible Studies
3.2. Quality Assessment and Publication Bias
3.3. Heterogeneity Assessment
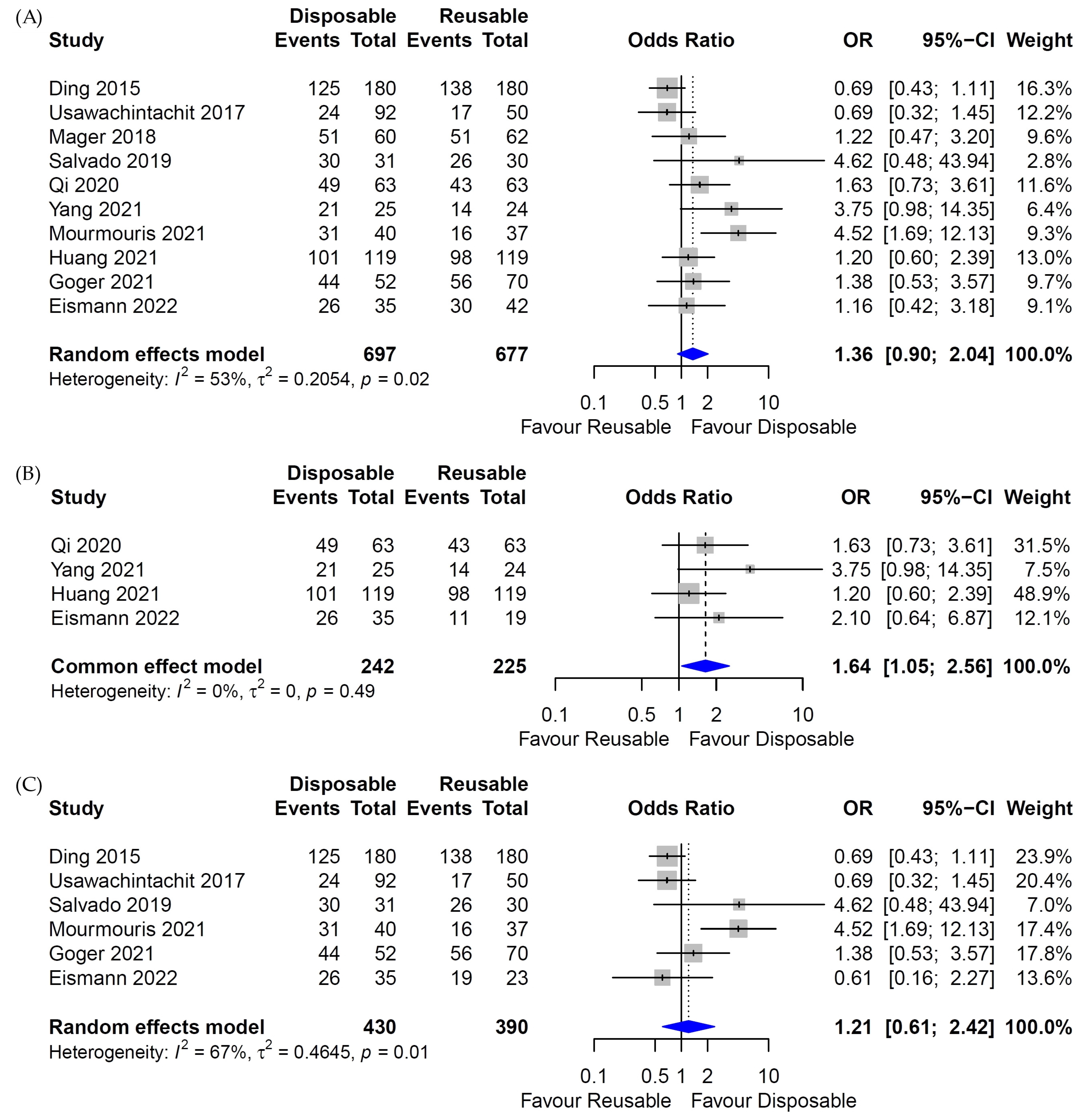
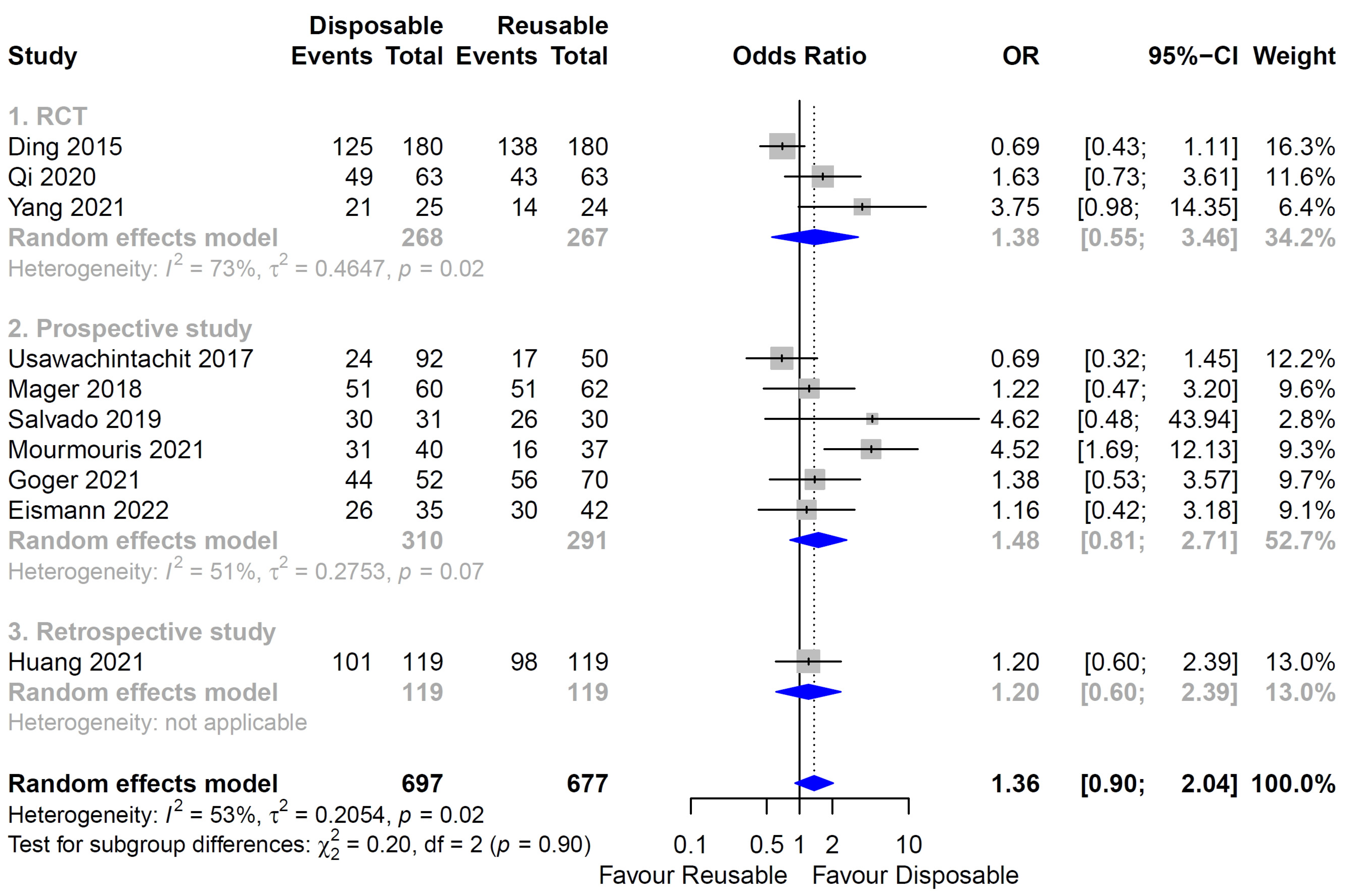
3.4. Stone-Free Rate
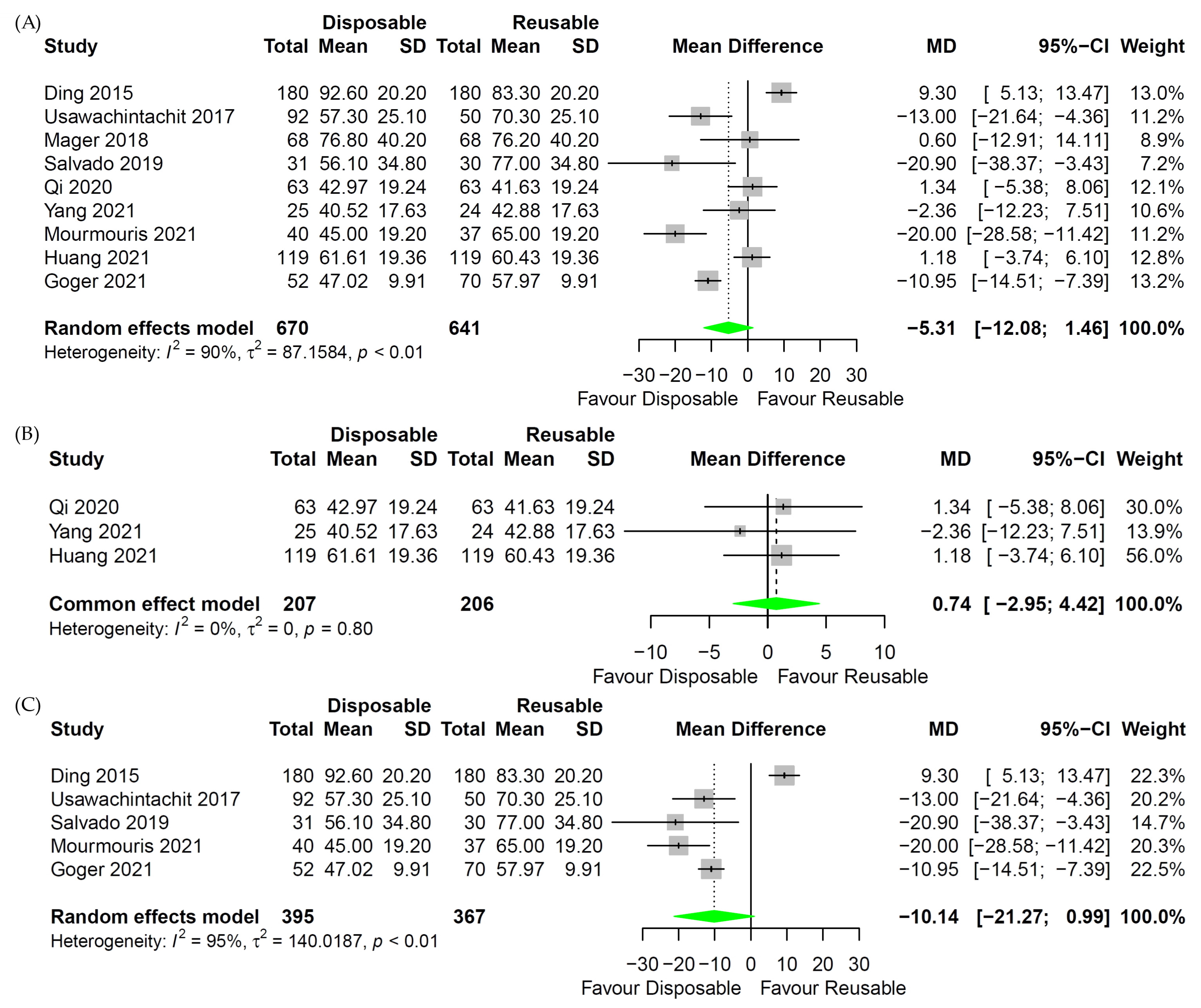
3.5. Operative Time
3.6. Length of Hospital Stay
3.7. Complication Rate
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lang, J.; Narendrula, A.; El-Zawahry, A.; Sindhwani, P.; Ekwenna, O. Global Trends in Incidence and Burden of Urolithiasis from 1990 to 2019: An Analysis of Global Burden of Disease Study Data. Eur. Urol. Open Sci. 2022, 35, 37–46. [Google Scholar] [CrossRef] [PubMed]
- Chewcharat, A.; Curhan, G. Trends in the prevalence of kidney stones in the United States from 2007 to 2016. Urolithiasis 2021, 49, 27–39. [Google Scholar] [CrossRef] [PubMed]
- Raheem, O.A.; Khandwala, Y.S.; Sur, R.L.; Ghani, K.R.; Denstedt, J.D. Burden of Urolithiasis: Trends in Prevalence, Treatments, and Costs. Eur. Urol. Focus 2017, 3, 18–26. [Google Scholar] [CrossRef]
- Liu, Y.; Chen, Y.; Liao, B.; Luo, D.; Wang, K.; Li, H.; Zeng, G. Epidemiology of urolithiasis in Asia. Asian J. Urol. 2018, 5, 205–214. [Google Scholar] [CrossRef]
- Jung, H.D.; Seo, I.Y.; Lee, J.Y. Large database study of urinary stone composition in South Korea: Korean Society of Endourology and Robotics (KSER) research series. Investig. Clin. Urol. 2021, 62, 462–469. [Google Scholar] [CrossRef]
- Türk, C.; Petřík, A.; Sarica, K.; Seitz, C.; Skolarikos, A.; Straub, M.; Knoll, T. EAU Guidelines on Interventional Treatment for Urolithiasis. Eur. Urol. 2016, 69, 475–482. [Google Scholar] [CrossRef]
- Jung, H.D.; Moon, Y.J.; Almujalhem, A.J.; Alqahtani, A.A.; Alkhureeb, M.A.; Lee, J.Y. The First 100 Cases of Endoscopic Combined Intrarenal Surgery in Korea: Matched Cohort Analyses versus Shock-Wave Lithotripsy. Yonsei Med. J. 2022, 63, 440–445. [Google Scholar] [CrossRef]
- Jeong, J.Y.; Kim, J.C.; Kang, D.H.; Lee, J.Y. Digital Videoscopic Retrograde Intrarenal Surgeries for Renal Stones: Time-to-Maximal Stone Length Ratio Analysis. Yonsei Med. J. 2018, 59, 303–309. [Google Scholar] [CrossRef]
- Grasso, M.; Bagley, D. A 7.5/8.2 F actively deflectable, flexible ureteroscope: A new device for both diagnostic and therapeutic upper urinary tract endoscopy. Urology 1994, 43, 435–441. [Google Scholar] [CrossRef]
- Lee, S.H.; Jeon, S.H. Lasers for the treatment of urinary stone disease. Investig. Clin. Urol. 2021, 62, 241–242. [Google Scholar] [CrossRef]
- Cho, S.Y.; Lee, J.Y.; Shin, D.G.; Seo, I.Y.; Yoo, S.; Park, H.K. Evaluation of Performance Parameters of the Disposable Flexible Ureterorenoscope (LITHOVUE) in Patients with Renal Stones: A Prospective, Observational, Single-arm, Multicenter Study. Sci. Rep. 2018, 8, 9795. [Google Scholar] [CrossRef]
- Kam, J.; Yuminaga, Y.; Beattie, K.; Ling, K.Y.; Arianayagam, M.; Canagasingham, B.; Ferguson, R.; Varol, C.; Khadra, M.; Winter, M.; et al. Single use versus reusable digital flexible ureteroscopes: A prospective comparative study. Int. J. Urol. 2019, 26, 999–1005. [Google Scholar] [CrossRef] [PubMed]
- Hennessey, D.B.; Fojecki, G.L.; Papa, N.P.; Lawrentschuk, N.; Bolton, D. Single-use disposable digital flexible ureteroscopes: An ex vivo assessment and cost analysis. BJU Int. 2018, 121 (Suppl. S3), 55–61. [Google Scholar] [CrossRef]
- Ventimiglia, E.; Somani, B.K.; Traxer, O. Flexible ureteroscopy: Reuse? Or is single use the new direction? Curr. Opin. Urol. 2020, 30, 113–119. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [PubMed]
- Ding, J.; Xu, D.; Cao, Q.; Huang, T.; Zhu, Y.; Huang, K.; Chen, Y.; Liang, C.; Qi, J.; Huang, Y. Comparing the Efficacy of a Multimodular Flexible Ureteroscope with Its Conventional Counterpart in the Management of Renal Stones. Urology 2015, 86, 224–229. [Google Scholar] [CrossRef]
- Eismann, L.; Kretschmer, A.; Alghamdi, A.; Eisel, M.; Sroka, R.; Stief, C.G.; Strittmatter, F. Clinical Evaluation of Single-Use, Fiber-Optic, and Digital Ureterorenoscopes in the Treatment of Kidney Stones. Urol. Int. 2022, 106, 476–481. [Google Scholar] [CrossRef]
- Göger, Y.E.; Özkent, M.S.; Kılınç, M.T.; Taşkapu, H.H.; Göger, E.; Aydın, A.; Sönmez, M.G.; Karalezli, G. Efficiency of retrograde intrarenal surgery in lower pole stones: Disposable flexible ureterorenoscope or reusable flexible ureterorenoscope? World J. Urol. 2021, 39, 3643–3650. [Google Scholar] [CrossRef]
- Huang, F.; Zhang, X.; Cui, Y.; Zhu, Z.; Li, Y.; Chen, J.; Zeng, F.; Li, Y.; Chen, Z.; Chen, H. Single-Use vs. Reusable Digital Flexible Ureteroscope to Treat Upper Urinary Calculi: A Propensity-Score Matching Analysis. Front. Surg. 2021, 8, 778157. [Google Scholar] [CrossRef]
- Mager, R.; Kurosch, M.; Höfner, T.; Frees, S.; Haferkamp, A.; Neisius, A. Clinical outcomes and costs of reusable and single-use flexible ureterorenoscopes: A prospective cohort study. Urolithiasis 2018, 46, 587–593. [Google Scholar] [CrossRef]
- Mourmouris, P.; Tzelves, L.; Raptidis, G.; Berdempes, M.; Markopoulos, T.; Dellis, G.; Siafakas, I.; Skolarikos, A. Comparison of a single-use, digital flexible ureteroscope with a reusable, fiberoptic ureteroscope for management of patients with urolithiasis. Arch. Ital. Urol. E Androl. 2021, 93, 326–329. [Google Scholar] [CrossRef] [PubMed]
- Qi, S.; Yang, E.; Bao, J.; Yang, N.; Guo, H.; Wang, G.; Li, N.; Cui, X.; Gao, W.; Ou, T.; et al. Single-Use Versus Reusable Digital Flexible Ureteroscopes for the Treatment of Renal Calculi: A Prospective Multicenter Randomized Controlled Trial. J. Endourol. 2020, 34, 18–24. [Google Scholar] [CrossRef]
- Salvadó, J.A.; Cabello, J.M.; Moreno, S.; Cabello, R.; Olivares, R.; Velasco, A. Endoscopic treatment of lower pole stones: Is a disposable ureteroscope preferable? Results of a prospective case-control study. Cent. Eur. J. Urol. 2019, 72, 280–284. [Google Scholar] [CrossRef]
- Usawachintachit, M.; Isaacson, D.S.; Taguchi, K.; Tzou, D.T.; Hsi, R.S.; Sherer, B.A.; Stoller, M.L.; Chi, T. A Prospective Case-Control Study Comparing LithoVue, a Single-Use, Flexible Disposable Ureteroscope, with Flexible, Reusable Fiber-Optic Ureteroscopes. J. Endourol. 2017, 31, 468–475. [Google Scholar] [CrossRef]
- Yang, E.; Jing, S.; Niu, Y.; Qi, S.; Yadav, P.K.; Yang, L.; Bao, J.; Tian, J.; Wang, J.; Li, N.; et al. Single-Use Digital Flexible Ureteroscopes as a Safe and Effective Choice for the Treatment of Lower Pole Renal Stones: Secondary Analysis of a Randomized-Controlled Trial. J. Endourol. 2021, 35, 1773–1778. [Google Scholar] [CrossRef]
- Marshall, V.F. Fiber optics in urology. J. Urol. 1964, 91, 110–114. [Google Scholar] [CrossRef]
- Takayasu, H.; Aso, Y.; Takagi, T.; Go, T. Clinical application of fiber-optic pyeloureteroscope. Urol. Int. 1971, 26, 97–104. [Google Scholar] [CrossRef]
- Bagley, D.H. Flexible ureteropyeloscopy with modular, “disposable” endoscope. Urology 1987, 29, 296–300. [Google Scholar] [CrossRef]
- Ziemba, J.B.; Matlaga, B.R. Understanding the costs of flexible ureteroscopy. Minerva Urol. Nefrol. 2016, 68, 586–591. [Google Scholar]
- Marchini, G.S.; Torricelli, F.C.; Batagello, C.A.; Monga, M.; Vicentini, F.C.; Danilovic, A.; Srougi, M.; Nahas, W.C.; Mazzucchi, E. A comprehensive literature-based equation to compare cost-effectiveness of a flexible ureteroscopy program with single-use versus reusable devices. Int. Braz. J. Urol. 2019, 45, 658–670. [Google Scholar] [CrossRef]
- Sung, J.C.; Springhart, W.P.; Marguet, C.G.; L’Esperance, J.O.; Tan, Y.H.; Albala, D.M.; Preminger, G.M. Location and etiology of flexible and semirigid ureteroscope damage. Urology 2005, 66, 958–963. [Google Scholar] [CrossRef]
- Afane, J.S.; Olweny, E.O.; Bercowsky, E.; Sundaram, C.P.; Dunn, M.D.; Shalhav, A.L.; McDougall, E.M.; Clayman, R.V. Flexible ureteroscopes: A single center evaluation of the durability and function of the new endoscopes smaller than 9Fr. J. Urol. 2000, 164, 1164–1168. [Google Scholar] [CrossRef]
- Legemate, J.D.; Kamphuis, G.M.; Freund, J.E.; Baard, J.; Zanetti, S.P.; Catellani, M.; Oussoren, H.W.; de la Rosette, J.J. Durability of Flexible Ureteroscopes: A Prospective Evaluation of Longevity, the Factors that Affect it, and Damage Mechanisms. Eur. Urol. Focus 2019, 5, 1105–1111. [Google Scholar] [CrossRef]
- Legemate, J.D.; Kamphuis, G.M.; Freund, J.E.; Baard, J.; Oussoren, H.W.; Spijkerman, I.J.B.; de la Rosette, J. Pre-Use Ureteroscope Contamination after High Level Disinfection: Reprocessing Effectiveness and the Relation with Cumulative Ureteroscope Use. J. Urol. 2019, 201, 1144–1151. [Google Scholar] [CrossRef] [PubMed]
- Bahaee, J.; Plott, J.; Ghani, K.R. Single-use flexible ureteroscopes: How to choose and what is around the corner? Curr. Opin. Urol. 2021, 31, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.Y.; Jung, H.D.; Kwon, S.H.; Lee, E.K.; Lee, J.Y.; Lee, S.H. Does Early Retrograde Intrarenal Surgery Improve the Cost-Effectiveness of Renal Stone Management? Yonsei Med. J. 2020, 61, 515–523. [Google Scholar] [CrossRef]
- Martin, C.J.; McAdams, S.B.; Abdul-Muhsin, H.; Lim, V.M.; Nunez-Nateras, R.; Tyson, M.D.; Humphreys, M.R. The Economic Implications of a Reusable Flexible Digital Ureteroscope: A Cost-Benefit Analysis. J. Urol. 2017, 197, 730–735. [Google Scholar] [CrossRef] [PubMed]
- Al-Balushi, K.; Martin, N.; Loubon, H.; Baboudjian, M.; Michel, F.; Sichez, P.C.; Martin, T.; Di-Crocco, E.; Gaillet, S.; Delaporte, V.; et al. Comparative medico-economic study of reusable vs. single-use flexible ureteroscopes. Int. Urol. Nephrol. 2019, 51, 1735–1741. [Google Scholar] [CrossRef]
- Ozimek, T.; Schneider, M.H.; Hupe, M.C.; Wiessmeyer, J.R.; Cordes, J.; Chlosta, P.L.; Merseburger, A.S.; Kramer, M.W. Retrospective Cost Analysis of a Single-Center Reusable Flexible Ureterorenoscopy Program: A Comparative Cost Simulation of Disposable fURS as an Alternative. J. Endourol. 2017, 31, 1226–1230. [Google Scholar] [CrossRef]
- Ofstead, C.L.; Heymann, O.L.; Quick, M.R.; Johnson, E.A.; Eiland, J.E.; Wetzler, H.P. The effectiveness of sterilization for flexible ureteroscopes: A real-world study. Am. J. Infect. Control 2017, 45, 888–895. [Google Scholar] [CrossRef]
- Dragos, L.B.; Somani, B.K.; Sener, E.T.; Buttice, S.; Proietti, S.; Ploumidis, A.; Iacoboaie, C.T.; Doizi, S.; Traxer, O. Which Flexible Ureteroscopes (Digital vs. Fiber-Optic) Can Easily Reach the Difficult Lower Pole Calices and Have Better End-Tip Deflection: In Vitro Study on K-Box. A petra Evaluation. J. Endourol. 2017, 31, 630–637. [Google Scholar] [CrossRef]
- Hyams, E.S.; Bruhn, A.; Lipkin, M.; Shah, O. Heterogeneity in the reporting of disease characteristics and treatment outcomes in studies evaluating treatments for nephrolithiasis. J. Endourol. 2010, 24, 1411–1414. [Google Scholar] [CrossRef]
- Elbahnasy, A.M.; Shalhav, A.L.; Hoenig, D.M.; Elashry, O.M.; Smith, D.S.; McDougall, E.M.; Clayman, R.V. Lower caliceal stone clearance after shock wave lithotripsy or ureteroscopy: The impact of lower pole radiographic anatomy. J. Urol. 1998, 159, 676–682. [Google Scholar] [CrossRef]
- Acar, C.; Cal, C. Impact of Residual Fragments following Endourological Treatments in Renal Stones. Adv. Urol. 2012, 2012, 813523. [Google Scholar] [CrossRef]
- Ghani, K.R.; Wolf, J.S., Jr. What is the stone-free rate following flexible ureteroscopy for kidney stones? Nat. Rev. Urol. 2015, 12, 281–288. [Google Scholar] [CrossRef]
- Chung, D.Y.; Lee, J.Y. Recommendations for Antibacterial Prophylaxis in Endourological Procedures. Urogenit. Tract. Infect. 2019, 14, 1–8. [Google Scholar] [CrossRef]
- Jung, H.D.; Cho, K.S.; Moon, Y.J.; Chung, D.Y.; Kang, D.H.; Lee, J.Y. Antibiotic prophylaxis for percutaneous nephrolithotomy: An updated systematic review and meta-analysis. PLoS ONE 2022, 17, e0267233. [Google Scholar] [CrossRef] [PubMed]
- Ofstead, C.L.; Hopkins, K.M.; Smart, A.G.; Eiland, J.E.; Wetzler, H.P.; Bechis, S.K. Reprocessing Effectiveness for Flexible Ureteroscopes: A Critical Look at the Evidence. Urology 2022, 164, 25–32. [Google Scholar] [CrossRef]
- Li, Y.; Chen, J.; Zhu, Z.; Zeng, H.; Zeng, F.; Chen, Z.; Yang, Z.; Cui, Y.; Chen, H.; Li, Y. Comparison of single-use and reusable flexible ureteroscope for renal stone management: A pooled analysis of 772 patients. Transl. Androl. Urol. 2021, 10, 483–493. [Google Scholar] [CrossRef] [PubMed]
- Domenech, A.; Alliende, C.; Vivaldi, B.; Pizzi, P. Comparison of pre- and post-surgical images of reusable and single use flexible ureteroscopes: A qualitative analysis. Cent. Eur. J. Urol. 2021, 74, 459–463. [Google Scholar] [CrossRef]
- Talso, M.; Goumas, I.K.; Kamphuis, G.M.; Dragos, L.; Tefik, T.; Traxer, O.; Somani, B.K. Reusable flexible ureterorenoscopes are more cost-effective than single-use scopes: Results of a systematic review from petra Uro-group. Transl. Androl. Urol. 2019, 8, S418–S425. [Google Scholar] [CrossRef]
- Davis, N.F.; McGrath, S.; Quinlan, M.; Jack, G.; Lawrentschuk, N.; Bolton, D.M. Carbon Footprint in Flexible Ureteroscopy: A Comparative Study on the Environmental Impact of Reusable and Single-Use Ureteroscopes. J. Endourol. 2018, 32, 214–217. [Google Scholar] [CrossRef]


| Author Year | Country | Study Design | Inclusion Criteria | Type of Scope | No. Patients | Age (Years) | Follow-Up | Definition of Stone-Free | Complications (No.) | Quality Assessment (SIGN) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| I–II | III–IV | |||||||||||
| Ding et al., 2015 [17] | China | RCT | Renal stones < 3 cm | Disposable fURS | PolyScope | 180 | 50.5 ± 12.8 | 1 day (4 weeks, if not acquire complete stone-free status) | ≤4 mm | Not stated | Not stated | 2+ |
| Reusable fiber-optic fURS | URF P-5 | 180 | 51.1 ± 13.7 | |||||||||
| Usawachintachit et al., 2017 [25] | USA | Prospective | Not stated | Disposable fURS | LithoVue | 92 | 55.8 ± 15.1 | 3 months | No fragments present (Insignificant residual fragment: <2 mm) | Not stated | Not stated | 2+ |
| Reusable fiber-optic fURS | URF-P6 | 50 | 50.5 ± 12.6 | |||||||||
| Mager et al., 2018 [21] | Germany | Prospective | Not stated | Disposable fURS | Lithovue | 68 | 54 ± 17 | Not stated | Not stated | 9 | 3 | 2+ |
| Reusable fiber-optic/digital fURS | Flex-X2S, Flex-XC | 68 | 59 ± 16 | 4 | 1 | |||||||
| Kam et al., 2019 [12] | Australia | Prospective | Patients undergoing retrograde fURS for the management of renal calculi, tumors, and ureteric strictures or ECIRS | Disposable fURS | Lithovue | 55 | 53.5 | Not stated | Not stated | 8 | 0 | 2+ |
| PU3022A | 31 | 54.1 | 9 | 0 | ||||||||
| Reusable digital fURS | URF-V2 | 64 | 53.3 | 12 | 0 | |||||||
| Salvado et al., 2019 [24] | Chile | Prospective | Single stone located in the inferior calyx | Disposable fURS | Uscope3022 | 31 | 50.4 ± 13.8 | 1 month | ≤1 mm | Not stated | Not stated | 1+ |
| Reusable fiber-optic fURS | Cobra | 30 | 49.9 ± 16.5 | |||||||||
| Qi et al., 2020 [23] | China | RCT | Maximum stone diameter 6~20 mm Renal stone or upper ureter stone | Disposable fURS | ZebraScope | 63 | 51.84 ± 13.16 | 1 month | ≤4 mm | Not stated | Not stated | 2+ |
| Reusable digital fURS | URF-V | 63 | 53.25 ± 12.11 | |||||||||
| Yang et al., 2021 [26] | China | RCT | Maximum stone diameter 6~20 mm Lower pole stone | Disposable fURS | ZebraScope | 25 | 52.72 ± 11.79 | 1 month | ≤4 mm | Not stated | Not stated | 2+ |
| Reusable digital fURS | URF-V | 24 | 54.00 ± 12.69 | |||||||||
| Mourmouris et al., 2021 [22] | Greece | Prospective | Radiopaque stone disease | Disposable fURS | Lithovue | 40 | 55.73 ± 13.47 | 1 day | ≤2 mm | Not stated | Not stated | 1+ |
| Reusable fiber-optic fURS | Flex-X2 | 37 | 55 ± 11.2 | |||||||||
| Huang et al., 2021 [20] | China | Retrospective | Upper urinary calculi | Disposable fURS | ZebraScope | 119 | 49.4 ± 12.7 | 1 month | ≤3 mm | 13 | 1 | 1+ |
| Reusable digital fURS | URF-V | 119 | 49.0 ± 12.0 | 9 | 3 | |||||||
| Göger et al., 2021 [19] | Turkey | Prospective | Lower pole stones | Disposable fURS | Uscope3022 | 52 | 52.4 ± 19.4 | 2~4 weeks | ≤3 mm | 9 | 0 | 1+ |
| Reusable fiber-optic fURS | Flex-X2S | 70 | 48.73 ± 14.7 | 6 | 1 | |||||||
| Eismann et al., 2022 [18] | Germany | Prospective | Urolithiasis | Disposable fURS | PU3022A | 35 | Not stated | Not stated | ≤1 mm | Not stated | Not stated | 2+ |
| Reusable digital fURS | Flex-XC | 19 | ||||||||||
| Reusable fiber-optic fURS | Flex-X2S | 23 | ||||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jun, D.Y.; Cho, K.S.; Jeong, J.Y.; Moon, Y.J.; Kang, D.H.; Jung, H.D.; Lee, J.Y. Comparison of Surgical Outcomes between Single-Use and Reusable Flexible Ureteroscopes for Renal Stone Management: A Systematic Review and Meta-Analysis. Medicina 2022, 58, 1388. https://doi.org/10.3390/medicina58101388
Jun DY, Cho KS, Jeong JY, Moon YJ, Kang DH, Jung HD, Lee JY. Comparison of Surgical Outcomes between Single-Use and Reusable Flexible Ureteroscopes for Renal Stone Management: A Systematic Review and Meta-Analysis. Medicina. 2022; 58(10):1388. https://doi.org/10.3390/medicina58101388
Chicago/Turabian StyleJun, Dae Young, Kang Su Cho, Jae Yong Jeong, Young Joon Moon, Dong Hyuk Kang, Hae Do Jung, and Joo Yong Lee. 2022. "Comparison of Surgical Outcomes between Single-Use and Reusable Flexible Ureteroscopes for Renal Stone Management: A Systematic Review and Meta-Analysis" Medicina 58, no. 10: 1388. https://doi.org/10.3390/medicina58101388
APA StyleJun, D. Y., Cho, K. S., Jeong, J. Y., Moon, Y. J., Kang, D. H., Jung, H. D., & Lee, J. Y. (2022). Comparison of Surgical Outcomes between Single-Use and Reusable Flexible Ureteroscopes for Renal Stone Management: A Systematic Review and Meta-Analysis. Medicina, 58(10), 1388. https://doi.org/10.3390/medicina58101388







