Clusters of Comorbidities in the Short-Term Prognosis of Acute Heart Failure among Elderly Patients: A Retrospective Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Approval and Data Availability Statement
2.2. Definition of Comorbidities
2.3. Inclusion and Exclusion Criteria
2.4. Statistical Analysis
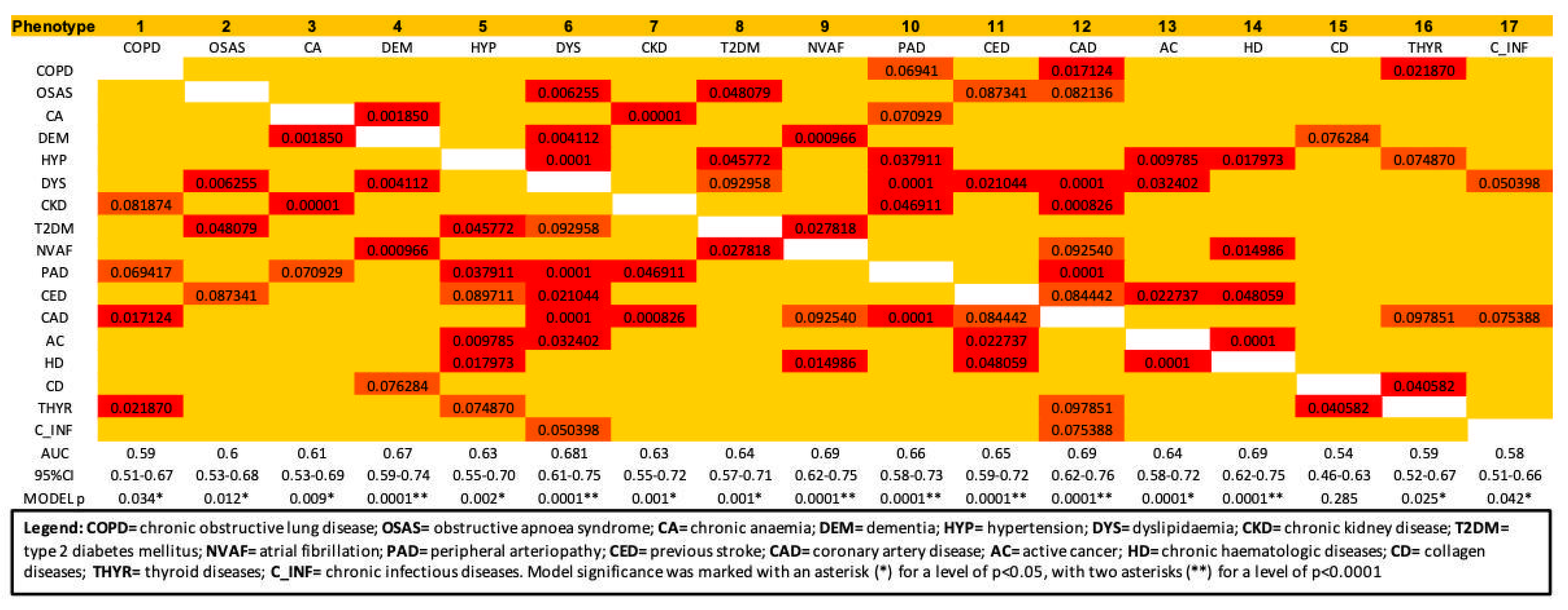
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ziaeian, B.; Fonarow, B.Z.G.C. Epidemiology and aetiology of heart failure. Nat. Rev. Cardiol. 2016, 13, 368–378. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chamberlain, A.M.; St. Sauver, J.L.; Gerber, Y.; Manemann, S.M.; Boyd, C.M.; Dunlay, S.M.; Rocca, W.A.; Rutten, L.J.F.; Jiang, R.; Weston, S.A.; et al. Multimorbidity in Heart Failure: A Community Perspective. Am. J. Med. 2015, 128, 38–45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahluwalia, S.C.; Gross, C.P.; Chaudhry, S.I.; Ning, Y.M.; Leo-Summers, L.; Van Ness, P.H.; Fried, T.R. Impact of Comorbidity on Mortality Among Older Persons with Advanced Heart Failure. J. Gen. Intern. Med. 2012, 27, 513–519. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rahimi, K.; Bennett, D.; Conrad, N.; Williams, T.M.; Basu, J.; Dwight, J.; Woodward, M.; Patel, A.; Mcmurray, J.; MacMahon, S. Risk Prediction in Patients with Heart Failure: A systematic review and analysis. JACC Heart Fail. 2014, 2, 440–446. [Google Scholar] [CrossRef]
- Hawkins, N.M.; Petrie, M.C.; Jhund, P.S.; Chalmers, G.W.; Dunn, F.G.; Mcmurray, J.J. Heart failure and chronic obstructive pulmonary disease: Diagnostic pitfalls and epidemiology. Eur. J. Heart Fail. 2009, 11, 130–139. [Google Scholar] [CrossRef] [Green Version]
- Macchia, A.; Moncalvo, J.J.R.; Kleinert, M.; Comignani, P.D.; Gimeno, G.; Arakaki, D.; Laffaye, N.; Fuselli, J.J.; Massolin, H.P.; Gambarte, J.; et al. Unrecognised ventricular dysfunction in COPD. Eur. Respir. J. 2012, 39, 51–58. [Google Scholar] [CrossRef] [Green Version]
- López-Sánchez, M.; Muñoz-Esquerre, M.; Huertas, D.; González-Costello, J.; Ribas, J.; Manresa, F.; Dorca, J.; Santos, S. High Prevalence of Left Ventricle Diastolic Dysfunction in Severe COPD Associated with A Low Exercise Capacity: A Cross-Sectional Study. PLoS ONE 2013, 8, e68034. [Google Scholar] [CrossRef] [Green Version]
- Sabit, R.; Bolton, C.E.; Fraser, A.G.; Edwards, J.M.; Edwards, P.H.; Ionescu, A.A.; Cockcroft, J.R.; Shale, D.J. Sub-clinical left and right ventricular dysfunction in patients with COPD. Respir. Med. 2010, 104, 1171–1178. [Google Scholar] [CrossRef] [Green Version]
- Hawkins, N.M.; Khosla, A.; Virani, S.A.; McMurray, J.J.V.; FitzGerald, J.M. B-type natriuretic peptides in chronic obstructive pulmonary disease: A systematic review. BMC Pulm. Med. 2017, 17, 11. [Google Scholar] [CrossRef] [Green Version]
- House, A.A. Management of Heart Failure in Advancing CKD: Core Curriculum 2018. Am. J. Kidney Dis. 2018, 72, 284–295. [Google Scholar] [CrossRef]
- Heywood, J.T.; Fonarow, G.C.; Costanzo, M.R.; Mathur, V.S.; Wigneswaran, J.R.; Wynne, J. High Prevalence of Renal Dysfunction and Its Impact on Outcome in 118,465 Patients Hospitalized with Acute Decompensated Heart Failure: A Report from the ADHERE Database. J. Card. Fail. 2007, 13, 422–430. [Google Scholar] [CrossRef] [PubMed]
- Cherian, T.S.; Shrader, P.; Fonarow, G.C.; Allen, L.A.; Piccini, J.P.; Peterson, E.D.; Thomas, L.; Kowey, P.R.; Gersh, B.J.; Mahaffey, K.W. Effect of Atrial Fibrillation on Mortality, Stroke Risk, and Quality-of-Life Scores in Patients with Heart Failure (from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation [ORBIT-AF]). Am. J. Cardiol. 2017, 119, 1763–1769. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kotecha, D.; Chudasama, R.; Lane, D.A.; Kirchhof, P.; Lip, G.Y. Atrial fibrillation and heart failure due to reduced versus preserved ejection fraction: A systematic review and meta-analysis of death and adverse outcomes. Int. J. Cardiol. 2016, 203, 660–666. [Google Scholar] [CrossRef] [PubMed]
- De Amicis, M.M.; Chivite, D.; Corbella, X.; Cappellini, M.D.; Formiga, F. Anemia is a mortality prognostic factor in patients initially hospitalized for acute heart failure. Intern. Emerg. Med. 2017, 12, 749–756. [Google Scholar] [CrossRef] [PubMed]
- Von Haehling, S.; Schefold, J.C.; Hodoscek, L.M.; Doehner, W.; Mannaa, M.; Anker, S.D.; Lainscak, M. Anaemia is an independent predictor of death in patients hospitalized for acute heart failure. Clin. Res. Cardiol. 2010, 99, 107–113. [Google Scholar] [CrossRef]
- Mentz, R.J.; Felker, G. Noncardiac Comorbidities and Acute Heart Failure Patients. Heart Fail. Clin. 2013, 9, 359–367. [Google Scholar] [CrossRef] [Green Version]
- Castelli, R.; Schiavon, R.; Deliliers, G.L. The impact of anaemia, transfusion dependency, comorbidities and polypharmacy in elderly patients with low-risk myelodysplastic syndromes. Med. Oncol. 2018, 35, 33. [Google Scholar] [CrossRef]
- Mohammed, S.F.; Borlaug, B.A.; Roger, V.L.; Mirzoyev, S.A.; Rodeheffer, R.J.; Chirinos, J.A.; Redfield, M.M. Comorbidity and Ventricular and Vascular Structure and Function in Heart Failure with Preserved Ejection Fraction. Circ. Hear. Fail. 2012, 5, 710–719. [Google Scholar] [CrossRef] [Green Version]
- El-Battrawy, I.; Behnes, M.; Ansari, U.; Hillenbrand, D.; Haghi, D.; Hoffmann, U.; Papavassiliu, T.; Elmas, E.; Fastner, C.; Becher, T.; et al. Comparison and outcome analysis of patients with apical and non-apical takotsubo cardiomyopathy. QJM Int. J. Med. 2016, 109, 797–802. [Google Scholar] [CrossRef] [Green Version]
- El-Battrawy, I.; Lang, S.; Ansari, U.; Behnes, M.; Hillenbrand, D.; Schramm, K.; Fastner, C.; Zhou, X.; Bill, V.; Hoffmann, U.; et al. Impact of concomitant atrial fibrillation on the prognosis of Takotsubo cardiomyopathy. Europace 2017, 19, 1288–1292. [Google Scholar] [CrossRef]
- Sattler, K.; El-Battrawy, I.; Lang, S.; Zhou, X.; Schramm, K.; Tülümen, E.; Kronbach, F.; Röger, S.; Behnes, M.; Kuschyk, J.; et al. Prevalence of cancer in Takotsubo cardiomyopathy: Short and long-term outcome. Int. J. Cardiol. 2017, 238, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Formiga, F.; Moreno-Gonzalez, R.; Chivite, D.; Franco, J.; Montero, A.; Corbella, X. High comorbidity, measured by the Charlson Comorbidity Index, associates with higher 1-year mortality risks in elderly patients experiencing a first acute heart failure hospitalization. Aging 2017, 30, 927–933. [Google Scholar] [CrossRef] [PubMed]
- Oudejans, I.; Mosterd, A.; Zuithoff, N.P.; Hoes, A.W. Comorbidity Drives Mortality in Newly Diagnosed Heart Failure: A Study among Geriatric Outpatients. J. Card. Fail. 2012, 18, 47–52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Testa, G.; Cacciatore, F.; Galizia, G.; DELLA Morte, D.; Mazzella, F.; Russo, S.; Ferrara, N.; Rengo, F.; Abete, P. Charlson Comorbidity Index does not predict long-term mortality in elderly subjects with chronic heart failure. Age Ageing 2009, 38, 734–740. [Google Scholar] [CrossRef] [Green Version]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; González-Juanatey, J.R.; Harjola, V.-P.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2016, 37, 2129–2200. [Google Scholar] [CrossRef] [Green Version]
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease KDIGO 2012 Clinical Practice Guideline for the Evaluation. Kidney Int. Suppl. 2013, 3, 136–150. [Google Scholar]
- Michalik, C.; Matusik, P.; Nowak, J.; Chmielowska, K.; Tomaszewski, K.A.; Parnicka, A.; Dubiel, M.; Gąsowski, J.; Grodzicki, T. Heart failure, comorbidities, and polypharmacy among elderly nursing home residents. Pol. Arch. Intern. Med. 2013, 123, 170–175. [Google Scholar] [CrossRef] [Green Version]
- Nobili, A.; Marengoni, A.; Tettamanti, M.; Salerno, F.; Pasina, L.; Franchi, C.; Iorio, A.; Marcucci, M.; Corrao, S.; Licata, G.; et al. Association between clusters of diseases and polypharmacy in hospitalized elderly patients: Results from the REPOSI study. Eur. J. Intern. Med. 2011, 22, 597–602. [Google Scholar] [CrossRef] [Green Version]
- Greenberg, B.H.; Abraham, W.T.; Albert, N.M.; Chiswell, K.; Clare, R.; Stough, W.G.; Gheorghiade, M.; O’Connor, C.M.; Sun, J.L.; Yancy, C.W.; et al. Influence of diabetes on characteristics and outcomes in patients hospitalized with heart failure: A report from the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF). Am. Heart J. 2007, 154, 277.e1–277.e8. [Google Scholar] [CrossRef]
- Rosolova, H.; Čech, J.; Simon, J.; Spinar, J.; Jandova, R.; Sen, J.W.; Holubec, L.; Topolčan, O. Short to long term mortality of patients hospitalised with heart failure in the Czech Republic—A report from the EuroHeart Failure Survey. Eur. J. Heart Fail. 2005, 7, 780–783. [Google Scholar] [CrossRef] [PubMed]
- Braunstein, J.B.; Anderson, G.F.; Gerstenblith, G.; Weller, W.; Niefeld, M.; Herbert, R.; Wu, A.W. Noncardiac comorbidity increases preventable hospitalizations and mortality among medicare beneficiaries with chronic heart failure. J. Am. Coll. Cardiol. 2003, 42, 1226–1233. [Google Scholar] [CrossRef] [Green Version]
- O’Connor, C.M.; Miller, A.B.; Blair, J.E.; Konstam, M.A.; Wedge, P.; Bahit, M.C.; Carson, P.; Haass, M.; Hauptman, P.J.; Metra, M.; et al. Causes of death and rehospitalization in patients hospitalized with worsening heart failure and reduced left ventricular ejection fraction: Results from efficacy of vasopressin antagonism in heart failure outcome study with tolvaptan (EVEREST) program. Am. Heart J. 2010, 159, 841–849.e1. [Google Scholar] [CrossRef] [PubMed]
- Auerbach, A.D.; Hamel, M.B.; Califf, R.M.; Davis, R.B.; Wenger, N.S.; Desbiens, N.; Goldman, L.; Vidaillet, H.; Connors, A.F.; Lynn, J.; et al. Patient characteristics associated with care by a cardiologist among adults hospitalized with severe congestive heart failure. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. J. Am. Coll. Cardiol. 2000, 36, 2119–2125. [Google Scholar] [CrossRef] [Green Version]
- Falsetti, L.; Rucco, M.; Proietti, M.; Viticchi, G.; Zaccone, V.; Scarponi, M.; Giovenali, L.; Moroncini, G.; Nitti, C.; Salvi, A. Risk prediction of clinical adverse outcomes with machine learning in a cohort of critically ill patients with atrial fibrillation. Sci. Rep. 2021, 11, 18925. [Google Scholar] [CrossRef] [PubMed]
- Falsetti, L.; Viticchi, G.; Zaccone, V.; Guerrieri, E.; Moroncini, G.; Luzzi, S.; Silvestrini, M. Shared Molecular Mechanisms among Alzheimer’s Disease, Neurovascular Unit Dysfunction and Vascular Risk Factors: A Narrative Review. Biomedicines 2022, 10, 439. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.S.; Chien, C.V.; Bidwell, J.T.; Gelow, J.M.; Denfeld, Q.E.; Creber, R.M.; Buck, H.G.; O’Mudd, J. Comorbidity profiles and inpatient outcomes during hospitalization for heart failure: An analysis of the U.S. Nationwide inpatient sample. BMC Cardiovasc. Disord. 2014, 14, 73. [Google Scholar] [CrossRef] [Green Version]
- Gulea, C.; Zakeri, R.; Quint, J.K. Model-based comorbidity clusters in patients with heart failure: Association with clinical outcomes and healthcare utilization. BMC Med. 2021, 19, 9. [Google Scholar] [CrossRef]
- Quan, H.; Li, B.; Couris, C.M.; Fushimi, K.; Graham, P.; Hider, P.; Januel, J.-M.; Sundararajan, V. Updating and Validating the Charlson Comorbidity Index and Score for Risk Adjustment in Hospital Discharge Abstracts Using Data from 6 Countries. Am. J. Epidemiol. 2011, 173, 676–682. [Google Scholar] [CrossRef] [Green Version]
- Falsetti, L.; Viticchi, G.; Tarquinio, N.; Silvestrini, M.; Capeci, W.; Catozzo, V.; Fioranelli, A.; Buratti, L.; Pellegrini, F. Charlson comorbidity index as a predictor of in-hospital death in acute ischemic stroke among very old patients: A single-cohort perspective study. Neurol. Sci. 2016, 37, 1443–1448. [Google Scholar] [CrossRef]
- Núñez, J.E.; Núñez, E.; Fácila, L.; Bertomeu, V.; Llàcer, À.; Bodí, V.; Sanchis, J.; Sanjuán, R.; Blasco, M.L.; Consuegra, L.; et al. Prognostic Value of Charlson Comorbidity Index at 30 Days and 1 Year After Acute Myocardial Infarction. Rev. Esp. Cardiol. 2004, 57, 842–849. [Google Scholar] [CrossRef]
- Radovanovic, D.; Seifert, B.; Urban, P.; Eberli, F.R.; Rickli, H.; Bertel, O.; Puhan, M.A.; Erne, P.; on behalf of the AMIS Plus Investigators Validity of Charlson Comorbidity Index in patients hospitalised with acute coronary syndrome. Insights from the nationwide AMIS Plus registry 2002–2012. Heart 2014, 100, 288–294. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Falsetti, L.; Zaccone, V.; Guerrieri, E.; Perrotta, G.; Diblasi, I.; Giuliani, L.; Palma, L.E.G.; Viticchi, G.; Fioranelli, A.; Moroncini, G.; et al. Implementation of EHMRG Risk Model in an Italian Population of Elderly Patients with Acute Heart Failure. J. Clin. Med. 2022, 11, 2982. [Google Scholar] [CrossRef] [PubMed]
- Falsetti, L.; Zaccone, V.; Viticchi, G.; Fioranelli, A.; Diblasi, I.; Guerrieri, E.; Ferrini, C.; Scarponi, M.; Giuliani, L.; Scalpelli, C.; et al. Improving the EHMRG Prognostic Evaluation of Acute Heart Failure with TAPSE/PASp: A Sequential Approach. Diagnostics 2022, 12, 478. [Google Scholar] [CrossRef]

| In-hospital death (n, %) | 55 (11.90%) |
| Days of admission (median, [IQR]) | 10 [6] |
Type of AHF
|
|
| Male sex (n, %) | 260 (56.60%) |
| Age (mean, ±SD), years | 83.98 (±8.02) |
| Charlson comorbidity index (median, [IQR]) | 6 [2] |
| Drugs taken at admission (median, [IQR]) | 7 [5] |
| General characteristics | |
| BNP at admission (mean, ±SD), ng/mL | 977.15 (±212.6) |
| BNP at discharge (mean, ±SD), ng/mL | 737.82 (±115.8) |
| Ejection Fraction (mean, ±SD), % | 46 (±13.1) |
| Comorbidities | |
| Number of comorbidities (mean, ±SD) | 4.44 (±1.89) |
| COPD (n, %) | 82 (17.90%) |
| OSAS (n, %) | 8 (1.70%) |
| Chronic Anemia (n, %) | 154 (33.60%) |
| Dementia (n, %) | 71 (15.50%) |
| Hypertension (n, %) | 332 (72.30%) |
| Dyslipidemia (n, %) | 186 (40.50%) |
| Chronic Kidney Disease (n, %) | 212 (46.20%) |
| Diabetes (n, %) | 140 (30.40%) |
| Atrial Fibrillation (n, %) | 249 (54.10%) |
| Peripheral Artery Disease (n, %) | 90 (19.60%) |
| Previous Stroke or TIA (n, %) | 72 (15.70%) |
| Previous Acute Myocardial Infarction (n, %) | 110 (24.00%) |
| Active Cancer (n, %) | 97 (21.10%) |
| Hematologic Pathologies (n, %) | 50 (10.90%) |
| Connective Tissue Diseases (n, %) | 38 (8.30%) |
| Thyroid Diseases (n, %) | 78 (17.00%) |
| Chronic Infectious Diseases (n, %) | 17 (3.70%) |
| Uncorrected Model | p | Corrected Model | p | |||
|---|---|---|---|---|---|---|
| AUC | 95% CI | AUC | 95% CI | |||
| Phenotype 4 | 0.67 | 0.59–0.74 | 0.0001 | 0.80 | 0.73–0.87 | 0.0001 |
| Phenotype 6 | 0.68 | 0.61–0.75 | 0.0001 | 0.83 | 0.77–0.88 | 0.0001 |
| Phenotype 9 | 0.69 | 0.62–0.75 | 0.0001 | 0.82 | 0.76–0.88 | 0.0001 |
| Phenotype 10 | 0.66 | 0.58–0.73 | 0.0001 | 0.81 | 0.75–0.87 | 0.0001 |
| Phenotype 11 | 0.65 | 0.59–0.72 | 0.0001 | 0.83 | 0.77–0.88 | 0.0001 |
| Phenotype 12 | 0.69 | 0.62–0.76 | 0.0001 | 0.81 | 0.75–0.88 | 0.0001 |
| Phenotype 14 | 0.69 | 0.58–0.72 | 0.0001 | 0.81 | 0.75–0.86 | 0.0001 |
| CCI | 0.69 | 0.58–0.75 | 0.0001 | 0.73 | 0.64–0.82 | 0.0001 |
| AUC (95% CI) | DeltaAUC | p (vs. CCI) | |
|---|---|---|---|
| Phenotype 4 | 0.80 (0.73–0.87) | 7.09% | 0.114 |
| Phenotype 6 | 0.83 (0.77–0.88) | 9.87% | 0.030 (*) |
| Phenotype 9 | 0.82 (0.76–0.88) | 9.28% | 0.036 (*) |
| Phenotype 10 | 0.81 (0.75–0.87) | 8.32% | 0.089 |
| Phenotype 11 | 0.83 (0.77–0.88) | 9.72% | 0.027 (*) |
| Phenotype 12 | 0.81 (0.75–0.88) | 8.38% | 0.048 (*) |
| Phenotype 14 | 0.81 (0.75–0.86) | 7.83% | 0.063 |
| HR | 95% CI | p | |
|---|---|---|---|
| CCI Q1 | (ref.) | - | - |
| CCI Q2 | 5.042 | 1.133–22.442 | 0.034 |
| CCI Q3 | 5.336 | 1.087–26.196 | 0.039 |
| CCI Q4 | 8.509 | 1.932–37.465 | 0.005 |
| Sex | 1.307 | 0.691–2.471 | 0.411 |
| Number of drugs at admission | 0.910 | 0.825–1.004 | 0.061 |
| BNP at admission | 1.005 | 1.001–1.010 | 0.000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Falsetti, L.; Viticchi, G.; Zaccone, V.; Guerrieri, E.; Diblasi, I.; Giuliani, L.; Giovenali, L.; Gialluca Palma, L.E.; Marconi, L.; Mariottini, M.; et al. Clusters of Comorbidities in the Short-Term Prognosis of Acute Heart Failure among Elderly Patients: A Retrospective Cohort Study. Medicina 2022, 58, 1394. https://doi.org/10.3390/medicina58101394
Falsetti L, Viticchi G, Zaccone V, Guerrieri E, Diblasi I, Giuliani L, Giovenali L, Gialluca Palma LE, Marconi L, Mariottini M, et al. Clusters of Comorbidities in the Short-Term Prognosis of Acute Heart Failure among Elderly Patients: A Retrospective Cohort Study. Medicina. 2022; 58(10):1394. https://doi.org/10.3390/medicina58101394
Chicago/Turabian StyleFalsetti, Lorenzo, Giovanna Viticchi, Vincenzo Zaccone, Emanuele Guerrieri, Ilaria Diblasi, Luca Giuliani, Laura Giovenali, Linda Elena Gialluca Palma, Lucia Marconi, Margherita Mariottini, and et al. 2022. "Clusters of Comorbidities in the Short-Term Prognosis of Acute Heart Failure among Elderly Patients: A Retrospective Cohort Study" Medicina 58, no. 10: 1394. https://doi.org/10.3390/medicina58101394
APA StyleFalsetti, L., Viticchi, G., Zaccone, V., Guerrieri, E., Diblasi, I., Giuliani, L., Giovenali, L., Gialluca Palma, L. E., Marconi, L., Mariottini, M., Fioranelli, A., Moroncini, G., Pansoni, A., Burattini, M., & Tarquinio, N. (2022). Clusters of Comorbidities in the Short-Term Prognosis of Acute Heart Failure among Elderly Patients: A Retrospective Cohort Study. Medicina, 58(10), 1394. https://doi.org/10.3390/medicina58101394







