Impact of Capsulotomy on Hip Biomechanics during Arthroscopy
Abstract
:1. Introduction
2. Materials and Methods
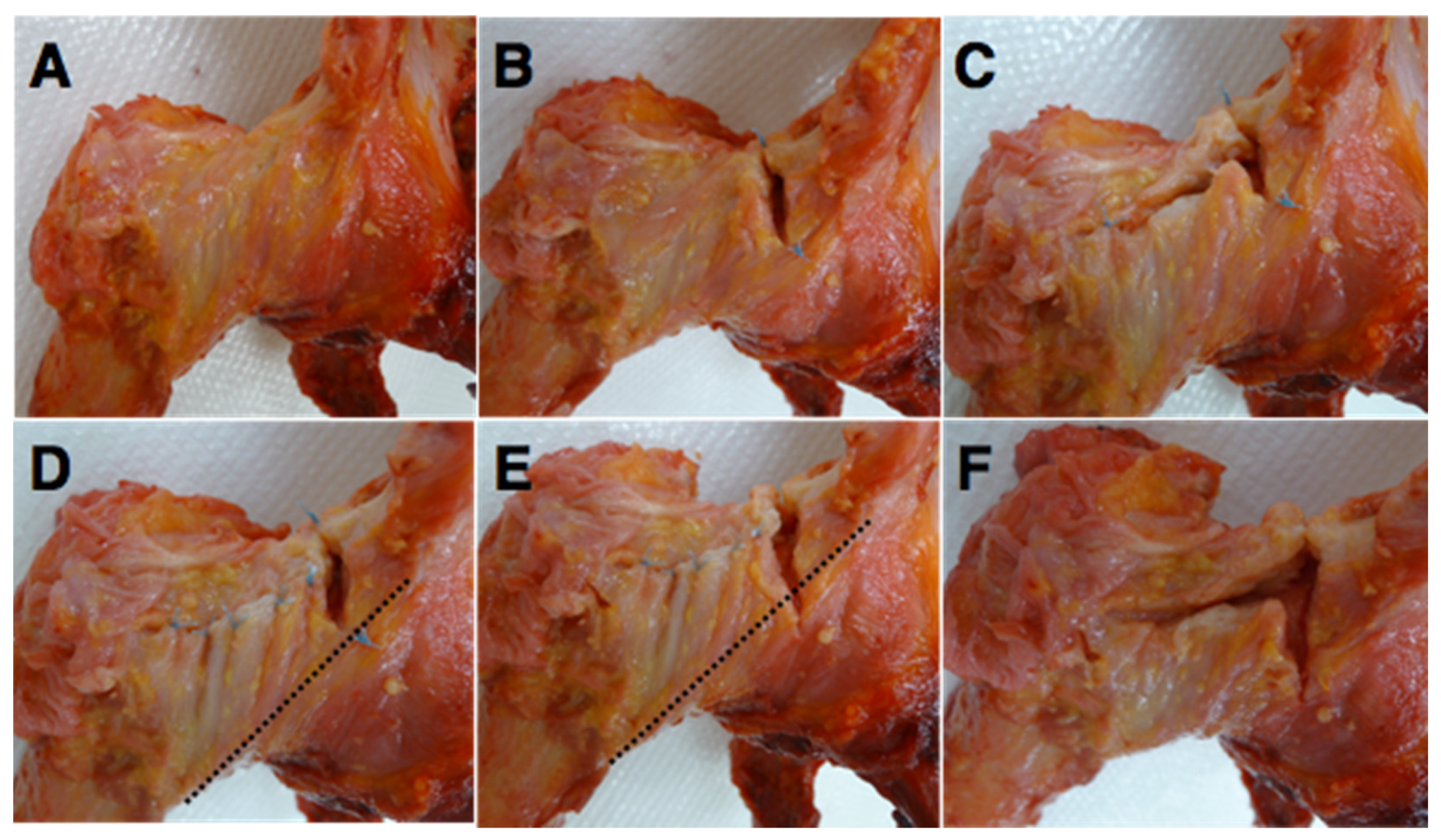
2.1. Specimen Preparation and Test Setup
2.2. Test Process
2.3. Statistical Analysis
3. Results
3.1. Effect of Conventional Capsulotomy
3.2. Effect of IFL Disruption
3.3. Effect of IFL and ZO Disruption
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Montgomery, S.R.; Ngo, S.S.; Hobson, T.; Nguyen, S.; Alluri, R.; Wang, J.C.; Hame, S.L. Trends and demographics in hip arthroscopy in the United States. Arthrosc. J. Arthrosc. Relat. Surg. 2013, 29, 661–665. [Google Scholar] [CrossRef] [PubMed]
- Botser, I.B.; Smith, T.W., Jr.; Nasser, R.; Domb, B.G. Open surgical dislocation versus arthroscopy for femoroacetabular impingement: A comparison of clinical outcomes. Arthrosc. J. Arthrosc. Relat. Surg. 2011, 27, 270–278. [Google Scholar] [CrossRef] [PubMed]
- Glick, J.M. Complications of hip arthroscopy by the lateral approach. In Current Management of Complications in Orthopaedics: Arthroscopic Surgery; Williams & Wilkins: Baltimore, MD, USA, 1990; pp. 193–201. [Google Scholar]
- Domb, B.G.; Philippon, M.J.; Giordano, B.D. Arthroscopic capsulotomy, capsular repair, and capsular plication of the hip: Relation to atraumatic instability. Arthrosc. J. Arthrosc. Relat. Surg. 2013, 29, 162–173. [Google Scholar] [CrossRef] [PubMed]
- Bedi, A.; Galano, G.; Walsh, C.; Kelly, B.T. Capsular management during hip arthroscopy: From femoroacetabular impingement to instability. Arthrosc. J. Arthrosc. Relat. Surg. 2011, 27, 1720–1731. [Google Scholar] [CrossRef]
- Philippon, M.J.; Stubbs, A.J.; Schenker, M.L.; Maxwell, R.B.; Ganz, R.; Leunig, M. Arthroscopic management of femoroacetabular impingement: Osteoplasty technique and literature review. Am. J. Sports Med. 2007, 35, 1571–1580. [Google Scholar] [CrossRef]
- Ito, H.; Song, Y.; Lindsey, D.P.; Safran, M.R.; Giori, N.J. The proximal hip joint capsule and the zona orbicularis contribute to hip joint stability in distraction. J. Orthop. Res. 2009, 27, 989–995. [Google Scholar] [CrossRef]
- Gold, M.; Munjal, A.; Varacallo, M. Anatomy, Bony Pelvis and Lower Limb, Hip Joint; StatPearls: Treasure Island, FL, USA, 2022. [Google Scholar]
- Hewitt, J.D.; Glisson, R.R.; Guilak, F.; Vail, T.P. The mechanical properties of the human hip capsule ligaments. J. Arthroplast. 2002, 17, 82–89. [Google Scholar] [CrossRef]
- Hidaka, E.; Aoki, M.; Izumi, T.; Suzuki, D.; Fujimiya, M. Ligament strain on the iliofemoral, pubofemoral, and ischiofemoral ligaments in cadaver specimens: Biomechanical measurement and anatomical observation. Clin. Anat. 2014, 27, 1068–1075. [Google Scholar] [CrossRef]
- Martin, H.D.; Savage, A.; Braly, B.A.; Palmer, I.J.; Beall, D.P.; Kelly, B. The function of the hip capsular ligaments: A quantitative report. Arthrosc. J. Arthrosc. Relat. Surg. 2008, 24, 188–195. [Google Scholar] [CrossRef]
- Myers, C.A.; Register, B.C.; Lertwanich, P.; Ejnisman, L.; Pennington, W.W.; Giphart, J.E.; LaPrade, R.F.; Philippon, M.J. Role of the acetabular labrum and the iliofemoral ligament in hip stability: An in vitro biplane fluoroscopy study. Am. J. Sports Med. 2011, 39, 85–91. [Google Scholar] [CrossRef]
- Benali, Y.; Katthagen, B.D. Hip subluxation as a complication of arthroscopic debridement. Arthrosc. J. Arthrosc. Relat. Surg. 2009, 25, 405–407. [Google Scholar] [CrossRef] [PubMed]
- Matsuda, D.K. Acute iatrogenic dislocation following hip impingement arthroscopic surgery. Arthrosc. J. Arthrosc. Relat. Surg. 2009, 25, 400–404. [Google Scholar] [CrossRef] [PubMed]
- Ranawat, A.S.; McClincy, M.; Sekiya, J.K. Anterior dislocation of the hip after arthroscopy in a patient with capsular laxity of the hip: A case report. J. Bone Jt. Surg. 2009, 91, 192–197. [Google Scholar] [CrossRef]
- Harris, J.D.; Slikker, W., III; Gupta, A.K.; McCormick, F.M.; Nho, S.J. Routine complete capsular closure during hip arthroscopy. Arthrosc. Tech. 2013, 2, e89–e94. [Google Scholar] [CrossRef] [PubMed]
- Heller, M.; Bergmann, G.; Kassi, J.-P.; Claes, L.; Haas, N.; Duda, G. Determination of muscle loading at the hip joint for use in pre-clinical testing. J. Biomech. 2005, 38, 1155–1163. [Google Scholar] [CrossRef]
- Wu, G.; Siegler, S.; Allard, P.; Kirtley, C.; Leardini, A.; Rosenbaum, D.; Whittle, M.; D’Lima, D.D.; Cristofolini, L.; Witte, H.; et al. ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion—Part I: Ankle, hip, and spine. J. Biomech. 2002, 35, 543–548. [Google Scholar] [CrossRef]
- Blankevoort, L.; Huiskes, R.; De Lange, A. Helical axes of passive knee joint motions. J. Biomech. 1990, 23, 1219–1229. [Google Scholar] [CrossRef] [Green Version]
- Leardini, A.; Cappozzo, A.; Catani, F.; Toksvig-Larsen, S.; Petitto, A.; Sforza, V.; Cassanelli, G.; Giannini, S. Validation of a functional method for the estimation of hip joint centre location. J. Biomech. 1999, 32, 99–103. [Google Scholar] [CrossRef]
- Smith, M.V.; Panchal, H.B.; Ruberte Thiele, R.A.; Sekiya, J.K. Effect of acetabular labrum tears on hip stability and labral strain in a joint compression model. Am. J. Sports Med. 2011, 39, 103–110. [Google Scholar] [CrossRef]
- Stewart, K.J.; Edmonds-Wilson, R.H.; Brand, R.A.; Brown, T.D. Spatial distribution of hip capsule structural and material properties. J. Biomech. 2002, 35, 1491–1498. [Google Scholar] [CrossRef]
- Chow, R.M.; Engasser, W.M.; Krych, A.J.; Levy, B.A. Arthroscopic capsular repair in the treatment of femoroacetabular impingement. Arthrosc. Tech. 2014, 3, e27–e30. [Google Scholar] [CrossRef] [PubMed]
- Philippon, M.J.; Michalski, M.P.; Campbell, K.J.; Rasmussen, M.T.; Goldsmith, M.T.; Devitt, B.M.; Wijdicks, C.A.; LaPrade, R.F. A quantitative analysis of hip capsular thickness. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 2548–2553. [Google Scholar] [CrossRef] [PubMed]
- Kelly, B.T.; Weiland, D.E.; Schenker, M.L.; Philippon, M.J. Arthroscopic labral repair in the hip: Surgical technique and review of the literature. Arthrosc. J. Arthrosc. Relat. Surg. 2005, 21, 1496–1504. [Google Scholar] [CrossRef] [PubMed]
- Bogunovic, L.; Gottlieb, M.; Pashos, G.; Baca, G.; Clohisy, J.C. Why do hip arthroscopy procedures fail? Clin. Orthop. Relat. Res. 2013, 471, 2523–2529. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heyworth, B.E.; Shindle, M.K.; Voos, J.E.; Rudzki, J.R.; Kelly, B.T. Radiologic and intraoperative findings in revision hip arthroscopy. Arthrosc. J. Arthrosc. Relat. Surg. 2007, 23, 1295–1302. [Google Scholar] [CrossRef] [PubMed]
- Shindle, M.K.; Ranawat, A.S.; Kelly, B.T. Diagnosis and management of traumatic and atraumatic hip instability in the athletic patient. Clin. Sports Med. 2006, 25, 309–326. [Google Scholar] [CrossRef] [PubMed]
- Fuss, F.K.; Bacher, A. New aspects of the morphology and function of the human hip joint ligaments. Am. J. Anat. 1991, 192, 1–13. [Google Scholar] [CrossRef]
- Hidaka, E.; Aoki, M.; Muraki, T.; Izumi, T.; Fujii, M.; Miyamoto, S. Evaluation of stretching position by measurement of strain on the ilio-femoral ligaments: An in vitro simulation using trans-lumbar cadaver specimens. Man. Ther. 2009, 14, 427–432. [Google Scholar] [CrossRef]






| 10° Extension | 0° Flexion | 30° Flexion | |
|---|---|---|---|
| Intact capsule | 0.8 ± 0.2 | 0.8 ± 0.2 | 1.0 ± 0.5 |
| Interportal capsulotomy | 1.2 ± 0.4 | 1.0 ± 0.1 | 1.5 ± 0.9 |
| T-capsulotomy | 1.9 ± 0.3 | 2.1 ± 0.5 | 2.3 ± 0.8 |
| Reproduced interportal capsulotomy | 1.2 ± 0.6 | 1.3 ± 0.4 | 1.2 ± 0.5 |
| Extended interportal capsulotomy | 1.6 ± 0.9 | 1.9 ± 0.8 | 2.0 ± 1.1 |
| Extended T-capsulotomy | 2.9 ± 0.9 | 2.6 ± 1.0 | 2.7 ± 0.9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, H.; Lim, W.; Lee, S.; Jo, S.; Jo, S. Impact of Capsulotomy on Hip Biomechanics during Arthroscopy. Medicina 2022, 58, 1418. https://doi.org/10.3390/medicina58101418
Lee H, Lim W, Lee S, Jo S, Jo S. Impact of Capsulotomy on Hip Biomechanics during Arthroscopy. Medicina. 2022; 58(10):1418. https://doi.org/10.3390/medicina58101418
Chicago/Turabian StyleLee, Hyeonjoon, Wonbong Lim, Seunghyun Lee, Sungmin Jo, and Suenghwan Jo. 2022. "Impact of Capsulotomy on Hip Biomechanics during Arthroscopy" Medicina 58, no. 10: 1418. https://doi.org/10.3390/medicina58101418






