Hypertensive Crisis-Related Hospitalizations and Subsequent Major Adverse Cardiac Events in Young Adults with Cannabis Use Disorder: A Nationwide Analysis
Abstract
:1. Introduction
2. Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yu, B.; Chen, X.; Chen, X.; Yan, H. Marijuana legalization and historical trends in marijuana use among US residents aged 12–25: Results from the 1979–2016 National Survey on drug use and health. BMC Public Health 2020, 20, 156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kicman, A.; Toczek, M. The Effects of Cannabidiol, a Non-Intoxicating Compound of Cannabis, on the Cardiovascular System in Health and Disease. Int. J. Mol. Sci. 2020, 21, 6740. [Google Scholar] [CrossRef] [PubMed]
- Fong, H.K.; Lodhi, M.U.; Kothapudi, V.N.; Singh, S.; Desai, R. Alarming trends in the frequency of malignant hypertension among admissions with a known cannabis use disorder. IJC Heart Vasc. 2021, 33, 100729. [Google Scholar] [CrossRef]
- Courts, J.; Maskill, V.; Gray, A.; Glue, P. Signs and symptoms associated with synthetic cannabinoid toxicity: Systematic review. Australas. Psychiatry 2016, 24, 598–601. [Google Scholar] [CrossRef] [PubMed]
- Castaneto, M.S.; Gorelick, D.A.; Desrosiers, N.A.; Hartman, R.L.; Pirard, S.; Huestis, M.A. Synthetic cannabinoids: Epidemiology, pharmacodynamics, and clinical implications. Drug Alcohol Depend. 2014, 144, 12–41. [Google Scholar] [CrossRef] [Green Version]
- Echeverria-Villalobos, M.; Todeschini, A.B.; Stoicea, N.; Fiorda-Diaz, J.; Weaver, T.; Bergese, S.D. Perioperative care of cannabis users: A comprehensive review of pharmacological and anesthetic considerations. J. Clin. Anesth. 2019, 57, 41–49. [Google Scholar] [CrossRef]
- Haleem, A.; Hwang, Y.J.; Elton-Marshall, T.; Rehm, J.; Imtiaz, S. The longitudinal relationship between cannabis use and hypertension. Drug Alcohol Rev. 2021, 40, 914–919. [Google Scholar] [CrossRef] [PubMed]
- Healthcare Cost and Utilization Project (HCUP). Database Overview of the National (Nationwide) Inpatient Sample. Available online: https://www.hcup-us.ahrq.gov/nisoverview.jsp (accessed on 17 January 2022).
- Carrà, G.; Bartoli, F.; Riboldi, I.; Trotta, G.; Crocamo, C. Poverty matters: Cannabis use among people with serious mental illness: Findings from the United States survey on drug use and health, 2015. Int. J. Soc. Psychiatry 2018, 64, 656–659. [Google Scholar] [CrossRef] [PubMed]
- Vidot, D.C.; Powers, M.; Gonzalez, R.; Jayaweera, D.T.; Roy, S.; Dong, C.; Messiah, S.E. Blood Pressure and Marijuana Use: Results from a Decade of NHANES Data. Am. J. Health Behav. 2019, 43, 887–897. [Google Scholar] [CrossRef] [PubMed]
- Yankey, B.N.; Strasser, S.; Okosun, I.S. A cross-sectional analysis of the association between marijuana and cigarette smoking with metabolic syndrome among adults in the United States. Diabetes Metab. Syndr. Clin. Res. Rev. 2016, 10, S89–S95. [Google Scholar] [CrossRef] [PubMed]
- Beaconsfield, P.; Ginsburg, J.; Rainsbury, R. Marihuana Smoking. N. Engl. J. Med. 1972, 287, 209–212. [Google Scholar] [CrossRef] [PubMed]
- Cooper, Z.D.; Haney, M. Actions of delta-9-tetrahydrocannabinol in cannabis: Relation to use, abuse, dependence. Int. Rev. Psychiatry 2009, 21, 104–112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spindle, T.R.; Cone, E.J.; Schlienz, N.; Mitchell, J.M.; Bigelow, G.E.; Flegel, R.; Hayes, E.; Vandrey, R. Acute Effects of Smoked and Vaporized Cannabis in Healthy Adults Who Infrequently Use Cannabis. JAMA Netw. Open 2018, 1, e184841. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abuhasira, R.; Haviv, Y.S.; Leiba, M.; Leiba, A.; Ryvo, L.; Novack, V. Cannabis is associated with blood pressure reduction in older adults—A 24-hours ambulatory blood pressure monitoring study. Eur. J. Intern. Med. 2021, 86, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, S.M.; Patel, R.P.; Cheh, P.; Hsia, J.; Rolle, I.V. Tobacco and Marijuana Initiation among African American and White Young Adults. Nicotine Tob. Res. 2015, 18, S57–S64. [Google Scholar] [CrossRef] [Green Version]
- Dierker, L.; Braymiller, J.; Rose, J.; Goodwin, R.; Selya, A. Nicotine dependence predicts cannabis use disorder symptoms among adolescents and young adults. Drug Alcohol Depend. 2018, 187, 212–220. [Google Scholar] [CrossRef] [PubMed]
- Hayaki, J.; Anderson, B.J.; Stein, M.D. Dual cannabis and alcohol use disorders in young adults: Problems magnified. Subst. Abus. 2016, 37, 579–583. [Google Scholar] [CrossRef] [Green Version]
- Skipina, T.M.; Patel, N.; Upadhya, B.; Soliman, E.Z. Relation of Cannabis Use to Elevated Atherosclerotic Cardiovascular Disease Risk Score. Am. J. Cardiol. 2021, 165, 46–50. [Google Scholar] [CrossRef]
- Lev-Ran, S.; Roerecke, M.; Le Foll, B.; George, T.P.; Mckenzie, K.; Rehm, J. The association between cannabis use and depression: A systematic review and meta-analysis of longitudinal studies. Psychol. Med. 2013, 44, 797–810. [Google Scholar] [CrossRef]
- Bambico, F.R.; Katz, N.; Debonnel, G.; Gobbi, G. Cannabinoids elicit antidepressant-like behavior and activate serotonergic neurons through the medial prefrontal cortex. J. Neurosci. 2007, 27, 11700–11711. [Google Scholar] [CrossRef] [Green Version]
- Di Forti, M.; Quattrone, D.; Freeman, T.P.; Tripoli, G.; Gayer-Anderson, C.; Quigley, H.; Rodriguez, V.; Jongsma, H.E.; Ferraro, L.; La Cascia, C.; et al. The contribution of cannabis use to variation in the incidence of psychotic disorder across Europe (EU-GEI): A multicentre case-control study. Lancet Psychiatry 2019, 6, 427–436. [Google Scholar] [CrossRef] [Green Version]
- Desai, R.; Thakkar, S.; Patel, H.P.; Bryan, E.; Tan, X.; Damarlapally, N.; Haque, F.A.; Farheen, N.; DeWitt, N.; Savani, S.; et al. Higher odds and rising trends in arrhythmia among young cannabis users with comorbid depression. Eur. J. Intern. Med. 2020, 80, 24–28. [Google Scholar] [CrossRef]
- Tan, W.C.; Lo, C.; Jong, A.; Xing, L.; FitzGerald, M.J.; Vollmer, W.M.; Buist, S.A.; Sin, D.D.; for the Vancouver Burden of Obstructive Lung Disease (BOLD) Research Group. Marijuana and chronic obstructive lung disease: A population-based study. Can. Med. Assoc. J. 2009, 180, 814–820. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gunasekaran, K.; Voruganti, D.C.; Singh Rahi, M.; Elango, K.; Ramalingam, S.; Geeti, A.; Kwon, J. Trends in Prevalence and Outcomes of Cannabis Use Among Chronic Obstructive Pulmonary Disease Hospitalizations: A Nationwide Population-Based Study 2005–2014. Cannabis Cannabinoid Res. 2021, 6, 340–348. [Google Scholar] [CrossRef] [PubMed]
- Adejumo, A.C.; Ajayi, T.O.; Adegbala, O.M.; Adejumo, K.L.; Alliu, S.; Akinjero, A.M.; Onyeakusi, N.E.; Ojelabi, O.; Bukong, T.N. Cannabis use is associated with reduced prevalence of progressive stages of alcoholic liver disease. Liver Int. 2018, 38, 1475–1486. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; You, C.-Y.; Kim, J.; Jo, Y.H.; Ro, Y.S.; Kang, S.-H.; Lee, H. Long-term cardiovascular risk of hypertensive events in emergency department: A population-based 10-year follow-up study. PLoS ONE 2018, 13, e0191738. [Google Scholar] [CrossRef]
- Richards, J.R.; Blohm, E.; Toles, K.A.; Jarman, A.F.; Ely, D.F.; Elder, J.W. The association of cannabis use and cardiac dysrhythmias: A systematic review. Clin. Toxicol. 2020, 58, 861–869. [Google Scholar] [CrossRef] [PubMed]
- Desai, R.; Fong, H.K.; Shah, K.; Kaur, V.P.; Savani, S.; Gangani, K.; Damarlapally, N.; Goyal, H. Rising Trends in Hospitalizations for Cardiovascular Events among Young Cannabis Users (18–39 Years) without Other Substance Abuse. Medicina 2019, 55, 438. [Google Scholar] [CrossRef] [Green Version]
- Richards, J.R.; Bing, M.L.; Moulin, A.K.; Elder, J.W.; Rominski, R.T.; Summers, P.J.; Laurin, E.G. Cannabis use and acute coronary syndrome. Clin. Toxicol. 2019, 57, 831–841. [Google Scholar] [CrossRef] [PubMed]
- Montecucco, F.; Di Marzo, V. At the heart of the matter: The endocannabinoid system in cardiovascular function and dysfunction. Trends Pharmacol. Sci. 2012, 33, 331–340. [Google Scholar] [CrossRef]
- Desai, R.; Singh, S.; Patel, K.; Goyal, H.; Shah, M.; Mansuri, Z.; Patel, S.; Mahuwala, Z.K.; Goldstein, L.B.; I Qureshi, A. Stroke in young cannabis users (18–49 years): National trends in hospitalizations and outcomes. Int. J. Stroke 2019, 15, 535–539. [Google Scholar] [CrossRef] [PubMed]
- Parekh, T.; Pemmasani, S.; Desai, R. Marijuana Use Among Young Adults (18–44 Years of Age) and Risk of Stroke. Stroke 2020, 51, 308–310. [Google Scholar] [CrossRef] [PubMed]
- Wolff, V.; Lauer, V.; Rouyer, O.; Sellal, F.; Meyer, N.; Raul, J.S.; Sabourdy, C.; Boujan, F.; Jahn, C.; Beaujeux, R.; et al. Cannabis Use, Ischemic Stroke, and Multifocal Intracranial Vasoconstriction. Stroke 2011, 42, 1778–1780. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leblanc, A.; Tirel-Badets, A.; Paleiron, N.; Castellant, P.; Cornily, J.-C.; Andre, M.; Grassin, F.; Feuvrier, Y.; Blanchard, C.; Zagnoli, F.; et al. Cannabis et infarctus du myocarde du sujet jeune: Association fortuite? À propos d’une observation. In Annales de Cardiologie et d’Angéiologie; Elsevier Masson: Paris, France, 2011; Volume 60, pp. 154–158. [Google Scholar] [CrossRef]
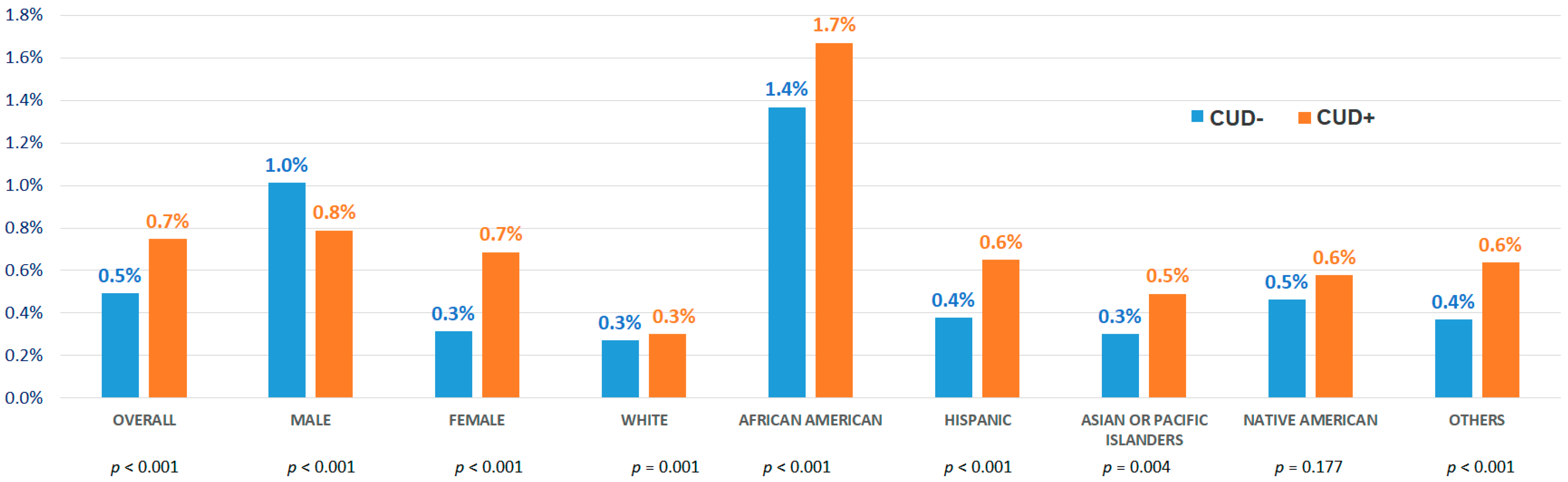
| CUD- | CUD+ | Total Young Admissions | ||
|---|---|---|---|---|
| (n = 18,824,587) | (n = 623,715) | (n= 19,448,302) | ||
| Age (years) at admission | Median [IQR] | 31 (26–37) | 29 (24–36) | 31 (25–37) |
| Sex | Male | 25.50% | 61.20% | 26.60% |
| Female | 74.50% | 38.80% | 73.40% | |
| Race | White | 54.30% | 53.10% | 54.30% |
| African American | 18.80% | 29.00% | 19.10% | |
| Hispanic | 17.80% | 12.10% | 17.60% | |
| Asian or Pacific Islander | 4.10% | 1.20% | 4.00% | |
| Native American | 0.80% | 1.20% | 0.80% | |
| Others | 4.10% | 3.40% | 4.10% | |
| Primary expected payer | Medicare | 6.20% | 9.00% | 6.30% |
| Medicaid | 39.20% | 49.90% | 39.50% | |
| Private including HMO | 43.40% | 22.40% | 42.70% | |
| Self-pay/No charge/Others | 11.20% | 18.70% | 11.40% | |
| Median household income national quartile for patient ZIP Code | 0–25th | 31.80% | 40.80% | 32.10% |
| 26–50th | 25.40% | 25.40% | 25.40% | |
| 51–75th | 23.50% | 20.20% | 23.40% | |
| 76–100th | 19.20% | 13.70% | 19.10% | |
| Non-elective admission | 68.10% | 88.00% | 68.70% | |
| Location/teaching status of hospital | Rural | 8.20% | 8.20% | 8.20% |
| Urban non-teaching | 23.10% | 23.40% | 23.10% | |
| Urban teaching | 68.70% | 68.40% | 68.70% | |
| Region of hospital | Northeast | 17.40% | 21.60% | 17.50% |
| Midwest | 21.30% | 24.70% | 21.40% | |
| South | 39.60% | 35.50% | 39.50% | |
| West | 21.70% | 18.20% | 21.60% | |
| Comorbidities | ||||
| Hypertension | 19.40% | 17.20% | 19.40% | |
| Diabetes mellitus | 6.50% | 5.40% | 6.50% | |
| Hyperlipidemia | 4.70% | 4.40% | 4.70% | |
| Obesity | 12.20% | 7.80% | 12.10% | |
| Peripheral vascular disease | 0.60% | 0.50% | 0.60% | |
| Tobacco use disorder | 23.10% | 58.80% | 24.20% | |
| Drug abuse | 5.50% | 86.20% | 8.10% | |
| Alcohol abuse | 3.90% | 19.10% | 4.40% | |
| Acquired immune deficiency syndrome | 0.20% | 0.60% | 0.30% | |
| Rheumatoid arthritis/collagen vascular heart disease | 1.20% | 0.70% | 1.20% | |
| Coagulopathy | 3.20% | 2.40% | 3.20% | |
| Congestive heart failure | 1.20% | 1.10% | 1.20% | |
| Chronic pulmonary disease | 8.60% | 12.80% | 8.70% | |
| Pulmonary circulation disease | 0.40% | 0.30% | 0.40% | |
| Chronic kidney disease | 2.70% | 2.00% | 2.60% | |
| Liver disease | 2.40% | 3.00% | 2.40% | |
| Other neurological disorders | 4.10% | 6.50% | 4.20% | |
| Depression | 7.90% | 13.60% | 8.00% | |
| Psychoses | 3.50% | 10.00% | 3.70% | |
| Overall Young Population | Young Adults with Known Benign Hypertension | |||||
|---|---|---|---|---|---|---|
| OR | 95%CI | p | OR | 95%CI | p | |
| Unadjusted | 1.52 | 1.41–1.64 | <0.001 | 1.25 | 1.09–1.44 | 0.002 |
| Model A: Adjusted with sociodemographic and hospital characteristics | 0.97 | 0.89–1.04 | 0.394 | 1.12 | 0.97–1.30 | 0.123 |
| Model B: Model A + comorbidities including alcohol abuse and tobacco use disorder | 1.22 | 1.13–1.32 | <0.001 | 1.17 | 1.01–1.36 | 0.034 |
| Model C: Model B + cocaine abuse and other stimulant abuse including amphetamine | 1.15 | 1.06–1.24 | 0.001 | 1.12 | 0.96–1.30 | 0.154 |
| CUD- (n = 4440) | CUD+ (n = 4440) | Total HTN Crisis in Young (n = 8880) | p | ||
|---|---|---|---|---|---|
| Age (years) at admission | Median [IQR] | 37 (31–41) | 36 (31–40) | 36 (31–40) | 0.004 |
| Sex | Male | 62.80% | 64.20% | 63.50% | 0.186 |
| Female | 37.20% | 35.80% | 36.50% | ||
| Race | White | 18.90% | 20.80% | 19.90% | 0.029 |
| African American | 65.10% | 64.40% | 64.80% | ||
| Hispanic | 11.80% | 10.20% | 11.00% | ||
| Asian or Pacific Islander | 0.70% | 0.80% | 0.70% | ||
| Native American | 1.10% | 0.90% | 1.00% | ||
| Others | 2.40% | 2.80% | 2.60% | ||
| Primary expected payer | Medicare | 15.10% | 15.50% | 15.30% | 0.403 |
| Medicaid | 48.20% | 46.70% | 47.50% | ||
| Private including HMO | 13.00% | 13.00% | 13.00% | ||
| Self-pay | 18.50% | 19.90% | 19.20% | ||
| No charges | 1.70% | 1.70% | 1.70% | ||
| Others | 3.60% | 3.20% | 3.40% | ||
| Median household income national quartile for patient ZIP Code | 0–25th | 63.00% | 60.50% | 61.70% | 0.061 |
| 26–50th | 20.40% | 21.70% | 21.10% | ||
| 51–75th | 12.50% | 12.80% | 12.70% | ||
| 76–100th | 4.20% | 5.00% | 4.60% | ||
| Elective versus non-elective admission | Non-elective | 97.70% | 97.60% | 97.70% | 0.724 |
| Elective | 2.30% | 2.40% | 2.30% | ||
| Bed size of hospital | Small | 18.80% | 20.40% | 19.60% | 0.145 |
| Medium | 30.00% | 28.80% | 29.40% | ||
| Large | 51.20% | 50.80% | 51.00% | ||
| Location/teaching status of hospital | Rural | 6.90% | 5.50% | 6.20% | 0.017 |
| Urban non-teaching | 16.80% | 17.90% | 17.30% | ||
| Urban teaching | 76.40% | 76.60% | 76.50% | ||
| Region of hospital | Northeast | 14.60% | 13.00% | 13.80% | 0.058 |
| Midwest | 20.30% | 21.60% | 20.90% | ||
| South | 49.40% | 49.00% | 49.20% | ||
| West | 15.70% | 16.40% | 16.00% | ||
| Comorbidity | |||||
| Diabetes mellitus | 31.30% | 24.00% | 27.60% | <0.001 | |
| Hyperlipidemia | 19.40% | 18.50% | 18.90% | 0.278 | |
| Obesity | 28.00% | 24.10% | 26.10% | <0.001 | |
| Peripheral vascular disease | 2.30% | 2.10% | 2.20% | 0.717 | |
| Tobacco use disorder | 40.80% | 65.40% | 53.10% | <0.001 | |
| Drug abuse | 8.40% | 87.70% | 48.10% | <0.001 | |
| Alcohol abuse | 5.60% | 12.80% | 9.20% | <0.001 | |
| Acquired immune deficiency syndrome | 1.20% | 0.60% | 0.90% | 0.001 | |
| Rheumatoid arthritis/collagen vascular disease | 2.90% | 2.70% | 2.80% | 0.521 | |
| Coagulopathy | 5.70% | 3.40% | 4.60% | <0.001 | |
| Congestive heart failure | 17.30% | 16.20% | 16.80% | 0.156 | |
| Valvular disease | 1.90% | 3.80% | 2.90% | <0.001 | |
| Chronic pulmonary disease | 12.50% | 14.20% | 13.30% | 0.019 | |
| Pulmonary circulation disease | 0.20% | 0.80% | 0.50% | <0.001 | |
| Renal failure | 45.30% | 34.30% | 39.80% | <0.001 | |
| Liver disease | 2.50% | 4.30% | 3.40% | <0.001 | |
| Other neurological disorders | 7.30% | 7.80% | 7.50% | 0.422 | |
| Depression | 8.30% | 11.00% | 9.70% | <0.001 | |
| Psychoses | 4.40% | 7.80% | 6.10% | <0.001 | |
| Prior Myocardial infarction | 3.30% | 4.30% | 3.80% | 0.012 | |
| Prior Stroke/Transient ischemic attack | 4.40% | 4.40% | 4.40% | 1 | |
| CUD- (n = 4440) | CUD+ (n = 4440) | Total HTN CRISIS IN YOUNG (n = 8880) | p | Adjusted Odds ratio | 95% CI | Adjusted p | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Composite major adverse cardiac/cerebrovascular events, MACCE | 475 | 10.7% | 490 | 11.0% | 965 | 10.9% | 0.609 | 1.16 | 0.91 | 1.47 | 0.231 | |
| All-cause mortality | 25 | 0.6% | 35 | 0.8% | 60 | 0.7% | 0.192 | 5.74 | 2.55 | 12.91 | <0.001 | |
| Acute myocardial infarction | 215 | 4.8% | 270 | 6.1% | 485 | 5.5% | 0.01 | 1.26 | 0.91 | 1.73 | 0.166 | |
| Arrhythmia | 430 | 9.7% | 500 | 11.3% | 930 | 10.5% | 0.015 | 1.73 | 1.38 | 2.17 | <0.001 | |
| Stroke | 240 | 5.4% | 215 | 4.8% | 455 | 5.1% | 0.229 | 1.46 | 1.02 | 2.10 | 0.040 | |
| Cardiac arrest including ventricular fibrillation/flutter | 25 | 0.6% | 20 | 0.5% | 45 | 0.5% | 0.455 | 2.75 | 0.99 | 7.66 | 0.053 | |
| Disposition of patient | Routine | 3575 | 80.5% | 3485 | 78.7% | 7060 | 79.6% | <0.001 | ||||
| Transfer to short term hospital | 110 | 2.5% | 70 | 1.6% | 180 | 2.0% | ||||||
| Other transfer including SNF, ICF, etc. | 150 | 3.4% | 135 | 3.0% | 285 | 3.2% | ||||||
| Home health care | 185 | 4.2% | 195 | 4.4% | 380 | 4.3% | ||||||
| Length of stay (days), median [IQR] | 3 (2–5) | 3 (2–5) | 3 (2–5) | 0.223 | ||||||||
| Cost adjusted for inflation in 2017 (USD), median [IQR] | 7074 (4429–11519) | 6948 (4768–12,063) | 6999 (4647–11,746) | 0.187 | ||||||||
| aOR | 95% CI | p | ||
|---|---|---|---|---|
| Lower | Upper | |||
| Age (years) at admission | 1.04 | 1.02 | 1.06 | <0.001 |
| Male vs. Female | 1.19 | 0.95 | 1.5 | 0.136 |
| Race | 0.001 | |||
| African American vs. white | 0.67 | 0.52 | 0.86 | 0.002 |
| Hispanic vs. white | 0.8 | 0.54 | 1.18 | 0.254 |
| Others vs. white | 1.85 | 1.08 | 3.18 | 0.025 |
| Primary expected payer | <0.001 | |||
| Medicaid vs. Medicare | 1.56 | 1.11 | 2.18 | 0.011 |
| Private including HMO vs. Medicare | 1.61 | 1.07 | 2.43 | 0.023 |
| Median household income national quartile for patient ZIP Code | <0.001 | |||
| 26–50th vs. 0–25th | 0.61 | 0.47 | 0.81 | <0.001 |
| 51–75th vs. 0–25th | 1.41 | 1.06 | 1.87 | 0.019 |
| 76–100th vs. 0–25th | 0.16 | 0.06 | 0.41 | <0.001 |
| Region of hospital | <0.001 | |||
| Midwest vs. Northeast | 2.06 | 1.37 | 3.09 | 0.001 |
| South vs. Northeast | 1.95 | 1.32 | 2.89 | 0.001 |
| West vs. Northeast | 1.06 | 0.66 | 1.71 | 0.801 |
| Comorbidities | ||||
| Acquired immune deficiency syndrome | 5.42 | 2.24 | 13.1 | <0.001 |
| Peripheral vascular disease | 3.03 | 1.79 | 5.11 | <0.001 |
| Coagulopathy | 2.07 | 1.33 | 3.22 | 0.001 |
| Prior myocardial infarction | 1.57 | 0.96 | 2.56 | 0.07 |
| Prior TIA/Stroke | 1.57 | 1.02 | 2.4 | 0.039 |
| Hypothyroidism | 1.5 | 0.79 | 2.85 | 0.213 |
| Other neurological disorders | 1.5 | 1.03 | 2.18 | 0.035 |
| Pulmonary circulation disease | 1.39 | 0.5 | 3.88 | 0.53 |
| Obesity | 1.25 | 1 | 1.58 | 0.053 |
| Tobacco use disorder | 1.23 | 0.98 | 1.54 | 0.076 |
| Hyperlipidemia | 1.2 | 0.93 | 1.55 | 0.168 |
| Valvular heart disease | 1.05 | 0.62 | 1.8 | 0.852 |
| Alcohol abuse | 1.01 | 0.75 | 1.37 | 0.941 |
| Chronic kidney disease | 0.94 | 0.74 | 1.2 | 0.61 |
| Diabetes mellitus | 0.89 | 0.7 | 1.15 | 0.374 |
| Depression | 0.72 | 0.49 | 1.05 | 0.086 |
| Congestive heart failure | 0.67 | 0.49 | 0.92 | 0.014 |
| Chronic pulmonary disease | 0.44 | 0.31 | 0.62 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Desai, R.; Jain, A.; Sultan, W.; Gandhi, Z.; Raju, A.R.; Varughese, V.J.; Jnaneswaran, G.; Agarwal, C.; Rizvi, B.; Mansuri, Z.; et al. Hypertensive Crisis-Related Hospitalizations and Subsequent Major Adverse Cardiac Events in Young Adults with Cannabis Use Disorder: A Nationwide Analysis. Medicina 2022, 58, 1465. https://doi.org/10.3390/medicina58101465
Desai R, Jain A, Sultan W, Gandhi Z, Raju AR, Varughese VJ, Jnaneswaran G, Agarwal C, Rizvi B, Mansuri Z, et al. Hypertensive Crisis-Related Hospitalizations and Subsequent Major Adverse Cardiac Events in Young Adults with Cannabis Use Disorder: A Nationwide Analysis. Medicina. 2022; 58(10):1465. https://doi.org/10.3390/medicina58101465
Chicago/Turabian StyleDesai, Rupak, Akhil Jain, Waleed Sultan, Zainab Gandhi, Athul Raj Raju, Vivek Joseph Varughese, Geethu Jnaneswaran, Charu Agarwal, Bisharah Rizvi, Zeeshan Mansuri, and et al. 2022. "Hypertensive Crisis-Related Hospitalizations and Subsequent Major Adverse Cardiac Events in Young Adults with Cannabis Use Disorder: A Nationwide Analysis" Medicina 58, no. 10: 1465. https://doi.org/10.3390/medicina58101465






