Perineal Massage during Pregnancy for the Prevention of Postpartum Urinary Incontinence: Controlled Clinical Trial
Abstract
1. Introduction
2. Materials and Methods
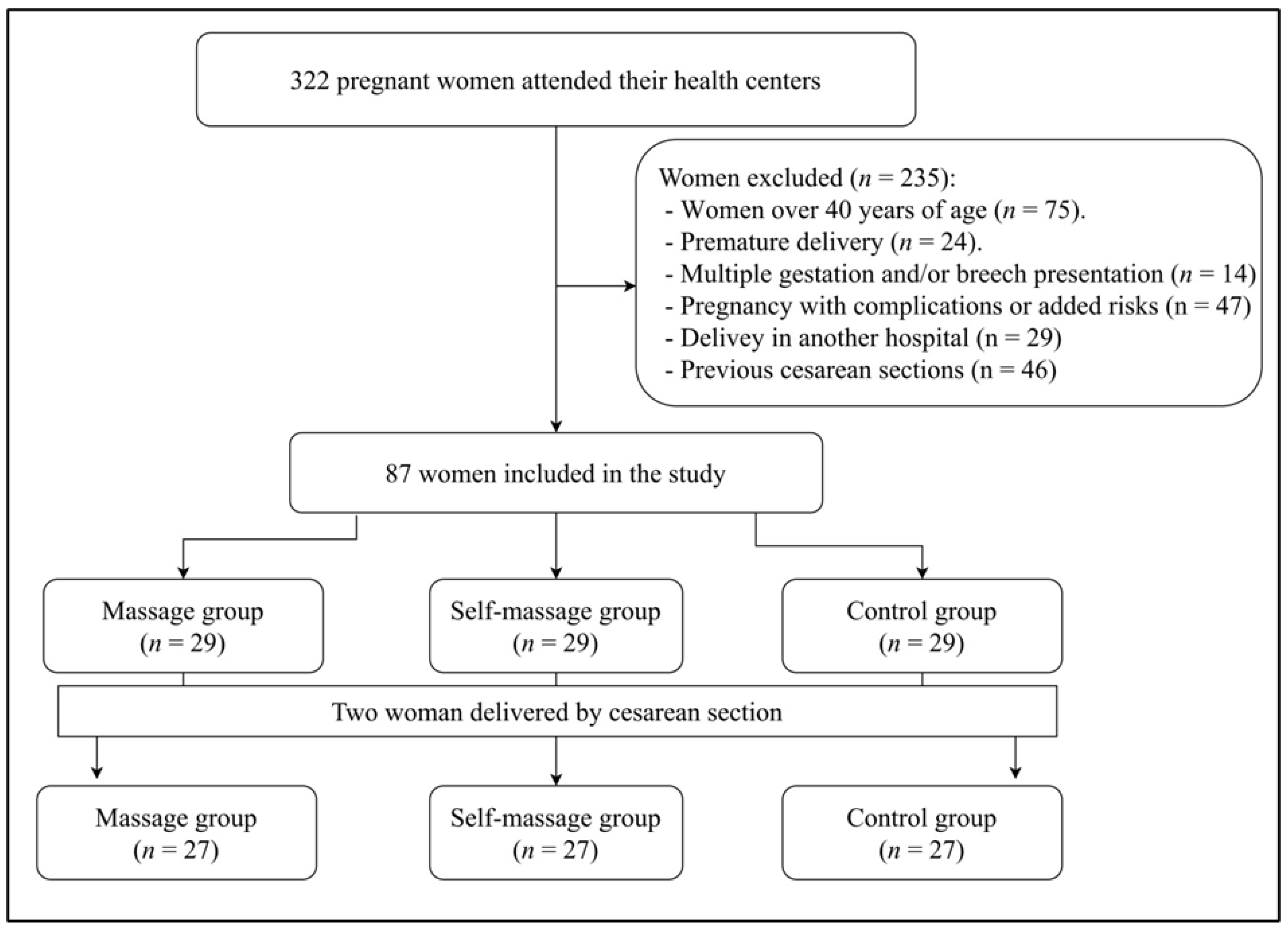
2.1. Design and Sample
2.2. Procedure
2.3. Interventions Applied
- (a)
- Perineal self-massage intervention. As described in a previous publication [16], self-massage group received standing instructions on perineal massage during pregnancy: it should be performed at least twice a week (on alternate days) for 10 min using a water-base lubricant from the 34th gestation week until delivery.
- (b)
- Perineal massage intervention. Perineal massage was applied by a physiotherapist expert in Urogynecol. and obstetrics over 6–10 sessions (from 34th gestation week until delivery) of 30 min each on a weekly basis. The intervention protocol has been used previously [16]. The procedure included direct manual techniques, the use of the EPI-NO® device (Northampton, UK), and another external manual technique [18].
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lukacz, E.S.; Santiago-Lastra, Y.; Albo, M.E.; Brubaker, L. Urinary incontinence in women: A review. JAMA 2017, 318, 1592–1604. [Google Scholar] [CrossRef] [PubMed]
- Frigerio, M.; Barba, M.; Cola, A.; Braga, A.; Celardo, A.; Munno, G.M.; Schettino, M.T.; Vagnetti, P.; de Simone, F.; di Lucia, A.; et al. Quality of life, psychological wellbeing, and sexuality in women with urinary incontinence-Where are we now: A narrative review. Medicina 2022, 58, 525. [Google Scholar] [CrossRef] [PubMed]
- Leirós-Rodríguez, R.; Romo-Pérez, V.; García-Soidán, J. Prevalence of urinary incontinence and its relation with sedentarism in Spain. Act. Urol. Esp. 2017, 41, 624–630. [Google Scholar] [CrossRef] [PubMed]
- Yuaso, D.R.; Santos, J.L.; Castro, R.A.; Duarte, Y.A.O.; Girão, M.J.B.C.; Berghmans, B.; Tamanini, J.T.N. Female double incontinence: Prevalence, incidence, and risk factors from the SABE (health, wellbeing and aging) study. Int. Urogynecol. J. 2018, 29, 265–272. [Google Scholar] [CrossRef] [PubMed]
- Hage-Fransen, M.A.; Wiezer, M.; Otto, A.; Wieffer-Platvoet, M.S.; Slotman, M.H.; Nijhuis, M.W.G.; Pool-Goudzwaard, A.L. Pregnancy-and obstetric-related risk factors for urinary incontinence, fecal incontinence, or pelvic organ prolapse later in life: A systematic review and meta-analysis. Acta Obstet. Gynecol. Scand. 2021, 100, 373–382. [Google Scholar] [CrossRef] [PubMed]
- Graziottin, A.; Murina, F. Vulvar pain during pregnancy and after childbirth. In Vulvar Pain; Graziottin, A., Murina, F., Eds.; Springer: Geneva, Switzerland, 2017; pp. 109–127. [Google Scholar]
- Dieb, A.S.; Shoab, A.Y.; Nabil, H.; Gabr, A.; Abdallah, A.A.; Shaban, M.M.; Attia, A.H. Perineal massage and training reduce perineal trauma in pregnant women older than 35 years: A randomized controlled trial. Int. Urogynecol. J. 2020, 31, 613–619. [Google Scholar] [CrossRef]
- Akhlaghi, F.; Baygi, Z.S.; Miri, M.; Najafi, M.N. Effect of Perineal Massage on the Rate of Episiotomy. J. Fam. Reprod. Health 2019, 13, 160–166. [Google Scholar] [CrossRef]
- Djusad, S.; Purwosunu, Y.; Hidayat, F. Relationship between Perineal Body Length and Degree of Perineal Tears in Primigravidas Undergoing Vaginal Delivery with Episiotomy. Obstet. Gynecol. Int. 2021, 2021, 2621872. [Google Scholar] [CrossRef]
- Laughon, S.K.; Berghella, V.; Reddy, U.M.; Sundaram, R.; Lu, Z.; Hoffman, M.K. Neonatal and Maternal Outcomes With Prolonged Second Stage of Labor. Obstet. Gynecol. 2014, 124, 57–67. [Google Scholar] [CrossRef]
- Hajebrahimi, S.; Corcos, J.; Lemieux, M. International consultation on incontinence questionnaire short form: Comparison of physician versus patient completion and immediate and delayed self-administration. Urology 2004, 63, 1076–1078. [Google Scholar] [CrossRef]
- Avery, K.; Donovan, J.; Peters, T.J.; Shaw, C.; Gotoh, M.; Abrams, P. ICIQ: A brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol. Urodyn. 2004, 23, 322–330. [Google Scholar] [CrossRef] [PubMed]
- Gotoh, M. Scored ICIQ-SF (International Consultation on Incontinence Questionnaire-Short Form) for symptoms and quality of life assessment in patients with urinary incontinence. JNBS 2001, 12, 227–231. [Google Scholar]
- Gotoh, M.; Homma, Y.; Funahashi, Y.; Matsukawa, Y.; Kato, M. Psychometric validation of the Japanese version of the International Consultation on Incontinence Questionnaire-Short Form. Int. J. Urol. 2009, 16, 303–306. [Google Scholar] [CrossRef] [PubMed]
- Espuña, M.; Rebollo, P.; Puig, M. Validación de la versión española del International Consultation on Incontinence Questionnaire-Short Form: Un cuestionario para evaluar la incontinencia urinaria [Validation of the Spanish versión of the International Consultation on Incontinence Questionnaire-Short Form: A questionnaire for assessing the urinary incontinence]. Med. Clin. 2004, 122, 288–292. [Google Scholar]
- Hebbar, S.; Pandey, H.; Chawla, A. Understanding King’s Health Questionnaire (KHQ) in assessment of female urinary incontinence. Int. J. Res. Med. Sci. 2015, 3, 531–538. [Google Scholar] [CrossRef]
- Badia, X.; Castro, D.; Conejero, J.; King’s Group. Validez del cuestionario King’s Health para la evaluación de la calidad de vida en pacientes con incontinencia urinaria [Validity of the King’s Health Questionnaire in the assessment of quality of life in patients with urinary incontinence]. Med. Clin. 2000, 114, 647–652. [Google Scholar] [CrossRef]
- Álvarez-González, M.; Leirós-Rodríguez, R.; Álvarez-Barrio, L.; López-Rodríguez, A.F. Prevalence of Perineal Tear Peripartum after Two Antepartum Perineal Massage Techniques: A Non-Randomised Controlled Trial. J. Clin. Med. 2021, 10, 4934. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioural Sciences; Laurence Erlbaum Associates: Mahwah, NJ, USA, 1988. [Google Scholar]
- Eason, E.; Labrecque, M.; Marcoux, S.; Mondor, M. Effects of carrying a pregnancy and of method of delivery on urinary incontinence: A prospective cohort study. BMC Pregnancy Childbirth 2004, 4, 4. [Google Scholar] [CrossRef]
- Beta, J.; Khan, N.; Fiolna, M.; Khalil, A.; Ramadan, G.; Akolekar, R. Maternal and neonatal complications of fetal macrosomia: Cohort study. Ultrasound Obstet. Gynecol. 2019, 54, 319–325. [Google Scholar] [CrossRef]
- Shinozaki, K.; Suto, M.; Ota, E.; Eto, H.; Horiuchi, S. Postpartum urinary incontinence and birth outcomes as a result of the pushing technique: A systematic review and meta-analysis. Int. Urogynecol. J. 2022, 33, 1435–1449. [Google Scholar] [CrossRef]
- Liang, C.C.; Chao, M.; Chang, S.D.; Chiu, S.Y.H. Impact of prepregnancy body mass index on pregnancy outcomes, incidence of urinary incontinence and quality of life during pregnancy—An observational cohort study. Biomed. J. 2020, 43, 476–483. [Google Scholar] [CrossRef] [PubMed]
- Can, Z.; Şahin, S. The prevalence of urinary incontinence in obese women and its effect on quality of life. Health Care Women Int. 2022, 43, 207–218. [Google Scholar] [CrossRef] [PubMed]
- Siahkal, S.F.; Iravani, M.; Mohaghegh, Z.; Sharifipour, F.; Zahedian, M. Maternal, obstetrical and neonatal risk factors’ impact on female urinary incontinence: A systematic review. Int. Urogynecol. J. 2020, 31, 2205–2224. [Google Scholar] [CrossRef] [PubMed]
- Wesnes, S.L.; Hannestad, Y.; Rortveit, G. Delivery parameters, neonatal parameters and incidence of urinary incontinence six months postpartum: A cohort study. Acta Obstet. Gynecol. Scand. 2017, 96, 1214–1222. [Google Scholar] [CrossRef]
- Abdelhakim, A.M.; Eldesouky, E.; Elmagd, I.A.; Mohammed, A.; Farag, E.A.; Mohammed, A.E.; Hamam, K.M.; Hussein, A.S.; Ali, A.S.; Keshta, N.H.A.; et al. Antenatal perineal massage benefits in reducing perineal trauma and postpartum morbidities: A systematic review and meta-analysis of randomized controlled trials. Int. Urogynecol. J. 2020, 31, 1735–1745. [Google Scholar] [CrossRef]
- Demirel, G.; Golbasi, Z. Effect of perineal massage on the rate of episiotomy and perineal tearing. Int. J. Gynecol. Obstet. 2015, 131, 183–186. [Google Scholar] [CrossRef]
- Zare, O.; Pasha, H.; Faramarzi, M. Effect of perineal massage on the incidence of episiotomy and perineal laceration. Health 2014, 6, 10–14. [Google Scholar] [CrossRef]
- Boelig, R.C.; Manuck, T.; Oliver, E.A.; Di Mascio, D.; Saccone, G.; Bellussi, F.; Berghella, V. Labor and delivery guidance for COVID-19. Am. J. Obstet. Gynecol. MFM 2020, 2, 100110. [Google Scholar] [CrossRef]
- Favilli, A.; Tiburzi, C.; Gargaglia, E.; Cerotto, V.; Bagaphou, T.C.; Checcaglini, A.; Bini, V.; Gori, F.; Torrioli, D.; Gerli, S. Does epidural analgesia influence labor progress in women aged 35 or more? J. Matern.-Fetal Neonatal Med. 2022, 35, 1219–1223. [Google Scholar] [CrossRef]
- World Health Organization. Managing Prolonged and Obstructed Labor; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
| All (n = 81) | Control (n = 27) | Self-Massage (n = 27) | Massage (n = 27) | |
|---|---|---|---|---|
| Age (years) | 32.6 ± 4 | 30.7 ± 4.3 a | 33.2 ± 3.2 | 33.8 ± 3.8 a |
| Height (cm) | 164 ± 6.2 | 163.4 ± 6.3 | 163.8 ± 5.5 | 164.7 ± 6.9 |
| Weight (kg) | 58 ± 8.3 | 58.2 ± 9.3 | 59.1 ± 8.9 | 56.8 ± 6.5 |
| Body Mass Index (kg/m2) | 21.6 ± 2.8 | 21.8 ± 2.8 | 22 ± 2.9 | 21.2 ± 2.9 |
| Weight gain (kg) | 12 ± 4 | 12.6 ± 4.8 | 11.9 ± 3.4 | 11.5 ± 3.8 |
| Deliveries (nº) | 1.3 ± 0.5 | 1.4 ± 0.5 | 1.2 ± 0.4 | 1.4 ± 0.6 |
| Labor week (nº) | 39.3 ± 1.7 | 39 ± 2.3 | 39.4 ± 1.6 | 39.5 ± 1.2 |
| Baby weight (kg) | 3.3 ± 0.4 | 3.3 ± 0.5 | 3.2 ± 0.2 | 3.4 ± 0.3 |
| Duration of labor (hours) | 10.9 ± 8.1 | 9.3 ± 6.6 | 13 ± 9.3 | 10.4 ± 8.2 |
| All (n = 81) | Control (n = 27) | Self-Massage (n = 27) | Massage (n = 27) | |
|---|---|---|---|---|
| Episiotomy * | 35 (43.2%) | 19 (70.4%) | 14 (51.9%) | 2 (7.4%) |
| Perineal tear: | ||||
| No | 57 (70.4%) | 15 (55.6%) | 20 (74.1%) | 22 (81.5%) |
| Mild | 17 (21%) | 8 (29.6%) | 5 (18.5%) | 4 (14.8%) |
| Moderate/severe | 7 (8.6%) | 4 (14.8%) | 2 (7.4%) | 1 (3.7%) |
| Position: | ||||
| Lithotomy | 63 (77.8%) | 25 (92.6%) | 21 (77.8%) | 17 (63%) |
| Sideways | 5 (6.2%) | 1 (3.7%) | 3 (11.1%) | 1 (3.7%) |
| Sit/squat | 11 (13.6%) | 1 (3.7%) | 2 (7.4%) | 8 (29.6%) |
| Standing | 2 (2.5%) | 0 (0%) | 1 (3.7%) | 1 (3.7%) |
| Instrumental: | ||||
| No | 64 (71.9%) | 17 (63%) | 23 (85.2%) | 24 (88.9%) |
| Vacuum | 10 (12.4%) | 6 (22.2%) | 1 (3.7%) | 3 (11.1%) |
| Forceps | 7 (8.6%) | 4 (14.8%) | 3 (11.1%) | 0 (0%) |
| Analgesia: | ||||
| No | 16 (19.8%) | 4 (14.8%) | 5 (18.5%) | 7 (25.9%) |
| Local | 2 (2.5%) | 1 (3.7%) | 1 (3.7%) | 0 (0%) |
| Epidural | 63 (77.8%) | 22 (81.5%) | 21 (77.8%) | 20 (74.1%) |
| Urinary incontinence: | ||||
| No | 56 (69.1%) | 18 (66.7%) | 15 (55.6%) | 23 (85.2%) |
| Yes | 25 (30.9%) | 9 (33.3%) | 12 (44.4%) | 4 (14.8%) |
| Severity of urinary incontinence (perception of amount of urine from leaks): | ||||
| Nothing | 56 (69.1%) | 18 (66.7%) | 15 (55.6%) | 23 (85.2%) |
| Little | 24 (29.6%) | 8 (29.6%) | 12 (44.4%) | 4 (14.8%) |
| Moderate | 1 (1.2%) | 1 (3.7%) | 0 (0%) | 0 (0%) |
| A lot | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Quality of life (mean ± standard deviation): | ||||
| 0–100 points | 39.6 ± 20.1 | 31.4 ± 34.1 | 57.3 ± 13.4 | 50 ± 18.9 |
| Variable | Quality of Life | UI Severity | ||||
|---|---|---|---|---|---|---|
| B | SE | R2 | B | SE | R2 | |
| Number of deliveries | −0.27 | 1 | 0.003 | 0.02 | 0.11 | 0.001 |
| Body Mass Index | 0.02 | 0.18 | 0.001 | 0.04 * | 0.02 | 0.05 |
| Weight gain | 0.04 | 0.16 | 0.003 | 0.01 | 0.01 | 0.002 |
| Labor week | −0.61 ** | 0.2 | 0.286 | −0.01 | 0.03 | 0.99 |
| Perineal tear | −0.97 | 0.99 | 0.04 | 0.08 | 0.121 | 0.005 |
| Duration of labor | 0.01 | 0.06 | 0.002 | 0.01 | 0.007 | 0.002 |
| Baby weight | −0.25 ** | 0.01 | 0.3 | 0.04 ** | 0.001 | 0.005 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Álvarez-González, M.; Leirós-Rodríguez, R.; Álvarez-Barrio, L.; López-Rodríguez, A.F. Perineal Massage during Pregnancy for the Prevention of Postpartum Urinary Incontinence: Controlled Clinical Trial. Medicina 2022, 58, 1485. https://doi.org/10.3390/medicina58101485
Álvarez-González M, Leirós-Rodríguez R, Álvarez-Barrio L, López-Rodríguez AF. Perineal Massage during Pregnancy for the Prevention of Postpartum Urinary Incontinence: Controlled Clinical Trial. Medicina. 2022; 58(10):1485. https://doi.org/10.3390/medicina58101485
Chicago/Turabian StyleÁlvarez-González, María, Raquel Leirós-Rodríguez, Lorena Álvarez-Barrio, and Ana F. López-Rodríguez. 2022. "Perineal Massage during Pregnancy for the Prevention of Postpartum Urinary Incontinence: Controlled Clinical Trial" Medicina 58, no. 10: 1485. https://doi.org/10.3390/medicina58101485
APA StyleÁlvarez-González, M., Leirós-Rodríguez, R., Álvarez-Barrio, L., & López-Rodríguez, A. F. (2022). Perineal Massage during Pregnancy for the Prevention of Postpartum Urinary Incontinence: Controlled Clinical Trial. Medicina, 58(10), 1485. https://doi.org/10.3390/medicina58101485








