Transitional Care Programs for Patients with High Nursing Activity Scores Reduce Unplanned Readmissions to Intensive Care Units
Abstract
:1. Introduction
2. Materials and Methods
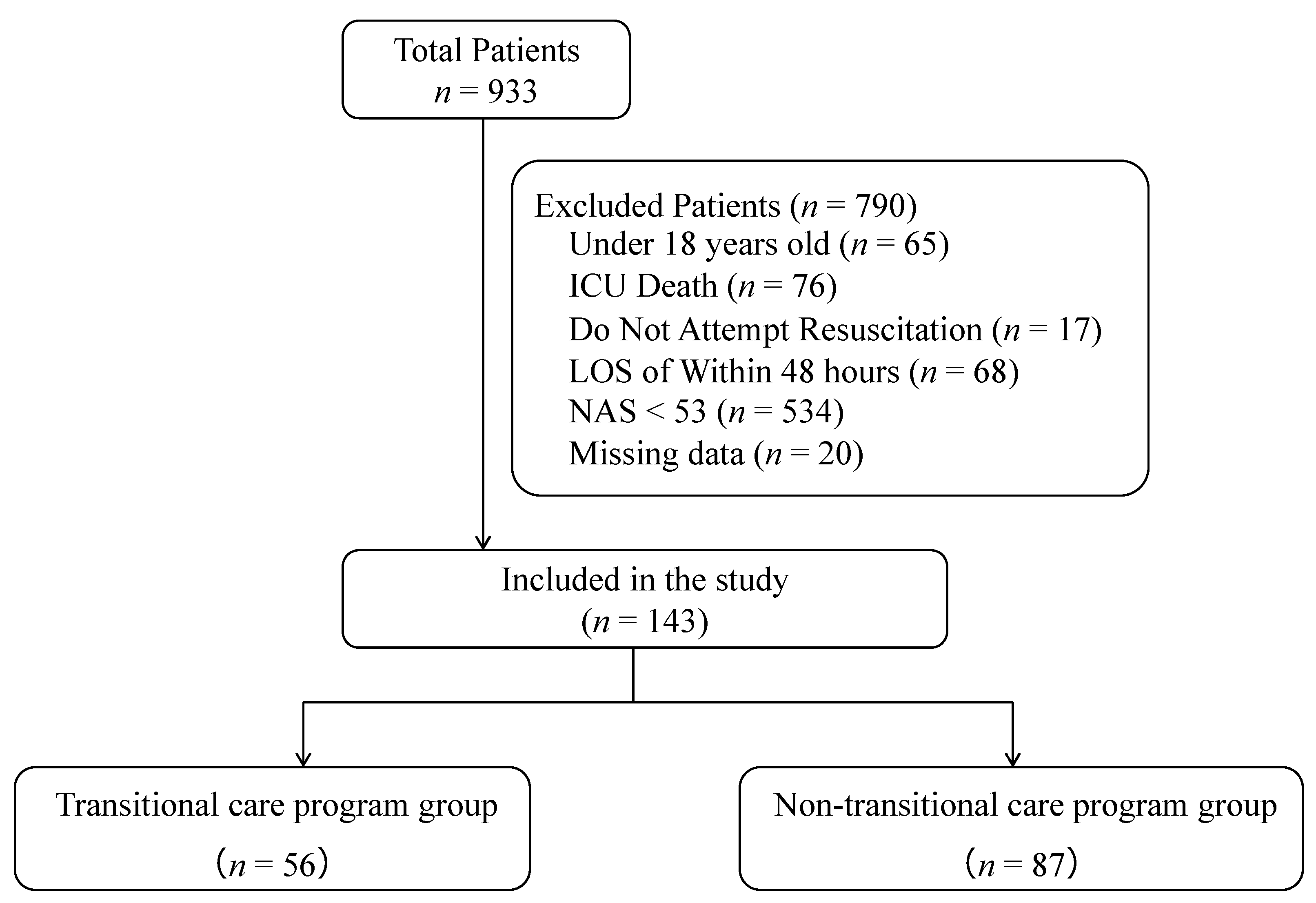
2.1. Design, Setting, and Inclusion Criteria
2.2. Exclusion Criteria
2.3. Outcome Measures
2.4. Data Collection
2.5. Criteria for ICU Discharge
- (1)
- A stable condition, which does not require treatment or monitoring that should be performed in the ICU.
- (2)
- Consensus with the attending physician at a multidisciplinary conference, confirming that the patient is ready for ICU discharge.
2.6. Description of TCP
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rosenberg, A.L.; Hofer, T.P.; Hayward, R.A.; Strachan, C.; Watts, C.M. Who bounces back? Physiologic and other predictors of intensive care unit readmission. Crit. Care Med. 2001, 29, 511–518. [Google Scholar] [CrossRef]
- Rojas, J.C.; Carey, K.A.; Edelson, D.P.; Venable, L.R.; Howell, M.D.; Churpek, M.M. Predicting Intensive Care Unit Readmission with Machine Learning Using Electronic Health Record Data. Ann. Am. Thorac. Soc. 2018, 15, 846–853. [Google Scholar] [CrossRef]
- Ponzoni, C.R.; Corrêa, T.D.; Filho, R.R.; Serpa Neto, A.; Assunção, M.S.C.; Pardini, A.; Schettino, G.P.P. Readmission to the Intensive Care Unit: Incidence, Risk Factors, Resource Use, and Outcomes. A Retrospective Cohort Study. Ann. Am. Thorac. Soc. 2017, 14, 1312–1319. [Google Scholar] [CrossRef]
- Woldhek, A.L.; Rijkenberg, S.; Bosman, R.J.; van der Voort, P.H.J. Readmission of ICU patients: A quality indicator? J. Crit. Care 2017, 38, 328–334. [Google Scholar] [CrossRef]
- Brown, S.E.S.; Ratcliffe, S.J.; Kahn, J.M.; Halpern, S.D. The epidemiology of intensive care unit readmissions in the United States. Am. J. Respir. Crit. Care Med. 2012, 185, 955–964. [Google Scholar] [CrossRef] [Green Version]
- Kaben, A.; Corrêa, F.; Reinhart, K.; Settmacher, U.; Gummert, J.; Kalff, R.; Sakr, Y. Readmission to a surgical intensive care unit: Incidence, outcome and risk factors. Crit. Care 2008, 12, R123. [Google Scholar] [CrossRef] [Green Version]
- Wong, E.G.; Parker, A.M.; Leung, D.G.; Brigham, E.P.; Arbaje, A.I. Association of severity of illness and intensive care unit readmission: A systematic review. Heart Lung 2016, 45, 3–9.e2. [Google Scholar] [CrossRef] [Green Version]
- Morgan, M.; Vernon, T.; Bradburn, E.H.; Miller, J.A.; Jammula, S.; Rogers, F.B. A Comprehensive Review of the Outcome for Patients Readmitted to the ICU Following Trauma and Strategies to Decrease Readmission Rates. J. Intensive Care Med. 2020, 35, 936–942. [Google Scholar] [CrossRef]
- Haruna, J.; Masuda, Y.; Tatsumi, H.; Sonoda, T. Nursing Activities Score at Discharge from the Intensive Care Unit Is Associated with Unplanned Readmission to the Intensive Care Unit. J. Clin. Med. Res. 2022, 11, 5203. [Google Scholar] [CrossRef]
- Azevedo, A.V.; Tonietto, T.A.; Boniatti, M.M. Nursing workload on the day of discharge from the intensive care unit is associated with readmission. Intensive Crit. Care Nurs. 2021, 69, 103162. [Google Scholar] [CrossRef]
- Elliott, M.; Worrall-Carter, L.; Page, K. Intensive care readmission: A contemporary review of the literature. Intensive Crit. Care Nurs. 2014, 30, 121–137. [Google Scholar] [CrossRef]
- Kareliusson, F.; De Geer, L.; Tibblin, A.O. Risk prediction of ICU readmission in a mixed surgical and medical population. J. Intensive Care Med. 2015, 3, 30. [Google Scholar] [CrossRef] [Green Version]
- Österlind, J.; Gerhardsson, J.; Myrberg, T. Critical care transition programs on readmission or death: A systematic review and meta-analysis. Acta Anaesthesiol. Scand. 2020, 64, 870–883. [Google Scholar] [CrossRef]
- Niven, D.J.; Bastos, J.F.; Stelfox, H.T. Critical care transition programs and the risk of readmission or death after discharge from an ICU: A systematic review and meta-analysis. Crit. Care Med. 2014, 42, 179–187. [Google Scholar] [CrossRef]
- So, H.M.; Yan, W.W.; Chair, S.Y. A nurse-led critical care outreach program to reduce readmission to the intensive care unit: A quasi-experimental study with a historical control group. Aust. Crit. Care 2019, 32, 494–501. [Google Scholar] [CrossRef]
- van Sluisveld, N.; Hesselink, G.; van der Hoeven, J.G.; Westert, G.; Wollersheim, H.; Zegers, M. Improving clinical handover between intensive care unit and general ward professionals at intensive care unit discharge. Intensive Care Med. 2015, 41, 589–604. [Google Scholar] [CrossRef] [Green Version]
- Ball, C.; Kirkby, M.; Williams, S. Effect of the critical care outreach team on patient survival to discharge from hospital and readmission to critical care: Non-randomised population based study. BMJ 2003, 327, 1014. [Google Scholar] [CrossRef] [Green Version]
- McGaughey, J.; Alderdice, F.; Fowler, R.; Kapila, A.; Mayhew, A.; Moutray, M. Outreach and Early Warning Systems (EWS) for the prevention of intensive care admission and death of critically ill adult patients on general hospital wards. Cochrane Database Syst. Rev. 2007, 3, CD005529. [Google Scholar] [CrossRef]
- Williams, T.A.; Leslie, G.; Finn, J.; Brearley, L.; Asthifa, M.; Hay, B.; Laurie, K.; Leen, T.; O’Brien, K.; Stuart, M.; et al. Clinical effectiveness of a critical care nursing outreach service in facilitating discharge from the intensive care unit. Am. J. Crit. Care 2010, 19, e63–e72. [Google Scholar] [CrossRef]
- Neto, R.; Carvalho, M.; Paixão, A.I.; Fernandes, P.; Castelões, P. The Impact of an Intensivist-Led Critical Care Transition Program. Cureus 2022, 14, e21313. [Google Scholar] [CrossRef]
- Leary, T.; Ridley, S. Impact of an outreach team on re-admissions to a critical care unit. Anaesthesia 2003, 58, 328–332. [Google Scholar] [CrossRef] [PubMed]
- Butcher, B.W.; Vittinghoff, E.; Maselli, J.; Auerbach, A.D. Impact of proactive rounding by a rapid response team on patient outcomes at an academic medical center. J. Hosp. Med. 2013, 8, 7–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miranda, D.R.; Nap, R.; de Rijk, A.; Schaufeli, W.; Iapichino, G.; TISS Working Group. Therapeutic Intervention Scoring System. Nursing activities score. Crit. Care Med. 2003, 31, 374–382. [Google Scholar] [CrossRef]
- Lachance, J.; Douville, F.; Dallaire, C.; Padilha, K.G.; Gallani, M.C. The use of the Nursing Activities Score in clinical settings: An integrative review. Rev. Esc. Enferm. USP 2015, 49, 147–156. [Google Scholar] [CrossRef] [Green Version]
- da Silva, M.C.M.; de Sousa, R.M.C.; Padilha, K.G. Factors associated with death and readmission into the Intensive Care Unit. Rev. Lat. Am. Enfermagem. 2011, 19, 911–919. [Google Scholar] [CrossRef] [Green Version]
- Hoogendoorn, M.E.; Margadant, C.C.; Brinkman, S.; Haringman, J.J.; Spijkstra, J.J.; de Keizer, N.F. Workload scoring systems in the Intensive Care and their ability to quantify the need for nursing time: A systematic literature review. Int. J. Nurs. Stud. 2020, 101, 103408. [Google Scholar] [CrossRef]
- Shankar-Hari, M.; Saha, R.; Wilson, J.; Prescott, H.C.; Harrison, D.; Rowan, K.; Rubenfeld, G.D.; Adhikari, N.K.J. Rate and risk factors for rehospitalisation in sepsis survivors: Systematic review and meta-analysis. Intensive Care Med. 2020, 46, 619–636. [Google Scholar] [CrossRef]
- Kastrup, M.; Powollik, R.; Balzer, F.; Röber, S.; Ahlborn, R.; von Dossow-Hanfstingl, V.; Wernecke, K.D.; Spies, C.D. Predictive ability of the stability and workload index for transfer score to predict unplanned readmissions after ICU discharge. Crit. Care Med. 2013, 41, 1608–1615. [Google Scholar] [CrossRef] [Green Version]
- Nates, J.L.; Nunnally, M.; Kleinpell, R.; Blosser, S.; Goldner, J.; Birriel, B.; Fowler, C.S.; Byrum, D.; Miles, W.S.; Bailey, H.; et al. ICU Admission, Discharge, and Triage Guidelines: A Framework to Enhance Clinical Operations, Development of Institutional Policies, and Further Research. Crit. Care Med. 2016, 44, 1553–1602. [Google Scholar] [CrossRef] [Green Version]
- Kramer, A.A.; Higgins, T.L.; Zimmerman, J.E. The association between ICU readmission rate and patient outcomes. Crit. Care Med. 2013, 41, 24–33. [Google Scholar] [CrossRef]
- Rosenberg, A.L.; Watts, C. Patients readmitted to ICUs*: A systematic review of risk factors and outcomes. Chest 2000, 118, 492–502. [Google Scholar] [CrossRef]
- Campbell, A.J.; Cook, J.A.; Adey, G.; Cuthbertson, B.H. Predicting death and readmission after intensive care discharge. Br. J. Anaesth. 2008, 100, 656–662. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caffin, C.L.; Linton, S.; Pellegrini, J. Introduction of a liaison nurse role in a tertiary paediatric ICU. Intensive Crit. Care Nurs. 2007, 23, 226–233. [Google Scholar] [CrossRef] [PubMed]
- Utzolino, S.; Kaffarnik, M.; Keck, T.; Berlet, M.; Hopt, U.T. Unplanned discharges from a surgical intensive care unit: Readmissions and mortality. J. Crit. Care 2010, 25, 375–381. [Google Scholar] [CrossRef]
- McQuillan, P.; Pilkington, S.; Allan, A.; Taylor, B.; Short, A.; Morgan, G.; Nielsen, M.; Barrett, D.; Smith, G.; Collins, C.H. Confidential inquiry into quality of care before admission to intensive care. BMJ 1998, 316, 1853–1858. [Google Scholar] [CrossRef] [Green Version]
- McGloin, H.; Adam, S.K.; Singer, M. Unexpected deaths and referrals to intensive care of patients on general wards. Are some cases potentially avoidable? J. R. Coll. Phys. Lond. 1999, 33, 255–259. Available online: https://www.ncbi.nlm.nih.gov/pubmed/10402575 (accessed on 30 August 2022).
- Kovner, C.; Gergen, P.J. Nurse staffing levels and adverse events following surgery in U.S. hospitals. Image J. Nurs. Sch. 1998, 30, 315–321. Available online: https://www.ncbi.nlm.nih.gov/pubmed/9866290 (accessed on 30 August 2022). [CrossRef]
- Lee, A.; Cheung, Y.S.L.; Joynt, G.M.; Leung, C.C.H.; Wong, W.-T.; Gomersall, C.D. Are high nurse workload/staffing ratios associated with decreased survival in critically ill patients? A cohort study. Ann. Intensive Care 2017, 7, 46. [Google Scholar] [CrossRef]
- Needleman, J.; Buerhaus, P.; Mattke, S.; Stewart, M.; Zelevinsky, K. Nurse-staffing levels and the quality of care in hospitals. N. Engl. J. Med. 2002, 346, 1715–1722. [Google Scholar] [CrossRef]
- Carayon, P.; Gurses, A.P. Nursing Workload and Patient Safety—A Human Factors Engineering Perspective. Agency for Healthcare Research and Quality (US); 2008. Available online: https://www.ncbi.nlm.nih.gov/books/NBK2657/ (accessed on 30 August 2022).
- Baggs, J.G.; Schmitt, M.H.; Mushlin, A.I.; Mitchell, P.H.; Eldredge, D.H.; Oakes, D.; Hutson, A.D. Association between nurse-physician collaboration and patient outcomes in three intensive care units. Crit. Care Med. 1999, 27, 1991–1998. [Google Scholar] [CrossRef]
- Llenore, E.; Ogle, K.R. Nurse-patient communication in the intensive care unit: A review of the literature. Aust. Crit. Care 1999, 12, 142–145. [Google Scholar] [CrossRef]
| TCP Group (n = 56) | Non-TCP Group (n = 87) | p Value | ||
|---|---|---|---|---|
| Age (years), mean ± SD | 67.3 ± 13.1 | 66.8 ± 12.9 | 0.88 | |
| Male, n (%) | 32 (57.1) | 55 (63.2) | 0.49 | |
| Charlson Comorbidities Index, mean ± SD | 1.6 ± 1.6 | 1.7 ± 1.4 | 0.63 | |
| APACHE II, mean ± SD | 16.5 ± 8.8 | 20.0 ± 5.9 | <0.01 | |
| SOFA at ICU admission, mean ± SD | 6.1 ± 3.8 | 6.2 ± 3.1 | 0.58 | |
| Reason for ICU admission | ||||
| Sepsis, n (%) | 18 (32.1) | 28 (32.2) | 1.00 | |
| Cardiovascular surgery, n (%) | 10 (17.9) | 11 (12.6) | 0.47 | |
| Other surgery, n (%) | 2 (3.6) | 5 (5.7) | 0.75 | |
| Respiratory failure, n (%) | 15 (26.8) | 16 (18.4) | 0.29 | |
| Circulatory failure, n (%) | 7 (12.5) | 5 (5.7) | 0.21 | |
| Cerebrovascular disease, n (%) | 3 (5.4) | 12 (13.8) | 0.16 | |
| Acute kidney injury, n (%) | 2 (3.6) | 4 (4.6) | 1.00 | |
| Acute pancreatitis, n (%) | 0 (0) | 3 (3.4) | 0.28 | |
| Liver failure, n (%) | 0 (0) | 3 (3.4) | 0.28 | |
| ICU readmission | 4 (7.1) | 23 (26.4) | <0.01 | |
| Reason for ICU readmission | ||||
| Respiratory failure, n (%) | 3 (75.0) | 14 (60.9) | 1.00 | |
| Circulatory failure, n (%) | 1 (25.0) | 7 (30.4) | 1.00 | |
| Cerebrovascular disease, n (%) | 0 (0) | 1 (4.3) | 1.00 | |
| Acute kidney injury, n (%) | 0 (0) | 2 (8.7) | 1.00 | |
| ICU length of stay (days), mean ± SD | 5.8 ± 6.5 | 7.5 ± 5.0 | 0.36 | |
| Mechanical ventilation, n (%) | 49 (87.5) | 70 (80.5) | 0.36 | |
| Ventilator days, mean ± SD | 5.8 ± 6.5 | 4.4 ± 4.0 | 0.69 | |
| CRRT, n. (%) | 16 (28.6) | 27 (31.0) | 0.85 | |
| Mortality for 28 days, n (%) | 3 (5.4) | 5 (5.7) | 1.00 | |
| Mortality for 90 days, n (%) | 11 (19.6) | 15 (17.2) | 0.83 | |
| NAS at ICU discharge, mean ± SD | 64.9 ± 11.1 | 66.7 ± 9.8 | 0.15 | |
| Frequency of TCP, mean ± SD | 1.4 ± 1.0 | - | ||
| Consultation details for TCP | ||||
| Respiratory support, n | 35 | - | ||
| Mobilization, n | 18 | - | ||
| Delirium care, n | 17 | - | ||
| Others, n | 26 | - | ||
| Odds Ratio (95%CI) | p Value | ||
|---|---|---|---|
| Primary Outcome | |||
| TCP | 5.15 (1.46–18.2) | 0.01 | |
| Secondary Outcomes | |||
| Delirium at ICU discharge | 0.89 (0.33–2.42) | 0.83 | |
| After-hours ICU discharge | 0.37 (0.09–1.50) | 0.16 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haruna, J.; Masuda, Y.; Tatsumi, H. Transitional Care Programs for Patients with High Nursing Activity Scores Reduce Unplanned Readmissions to Intensive Care Units. Medicina 2022, 58, 1532. https://doi.org/10.3390/medicina58111532
Haruna J, Masuda Y, Tatsumi H. Transitional Care Programs for Patients with High Nursing Activity Scores Reduce Unplanned Readmissions to Intensive Care Units. Medicina. 2022; 58(11):1532. https://doi.org/10.3390/medicina58111532
Chicago/Turabian StyleHaruna, Junpei, Yoshiki Masuda, and Hiroomi Tatsumi. 2022. "Transitional Care Programs for Patients with High Nursing Activity Scores Reduce Unplanned Readmissions to Intensive Care Units" Medicina 58, no. 11: 1532. https://doi.org/10.3390/medicina58111532
APA StyleHaruna, J., Masuda, Y., & Tatsumi, H. (2022). Transitional Care Programs for Patients with High Nursing Activity Scores Reduce Unplanned Readmissions to Intensive Care Units. Medicina, 58(11), 1532. https://doi.org/10.3390/medicina58111532






