Successful Interventional Management of Life-Threatening Bleeding after Oocyte Retrieval: A Case Report and Review of the Literature
Abstract
:1. Introduction
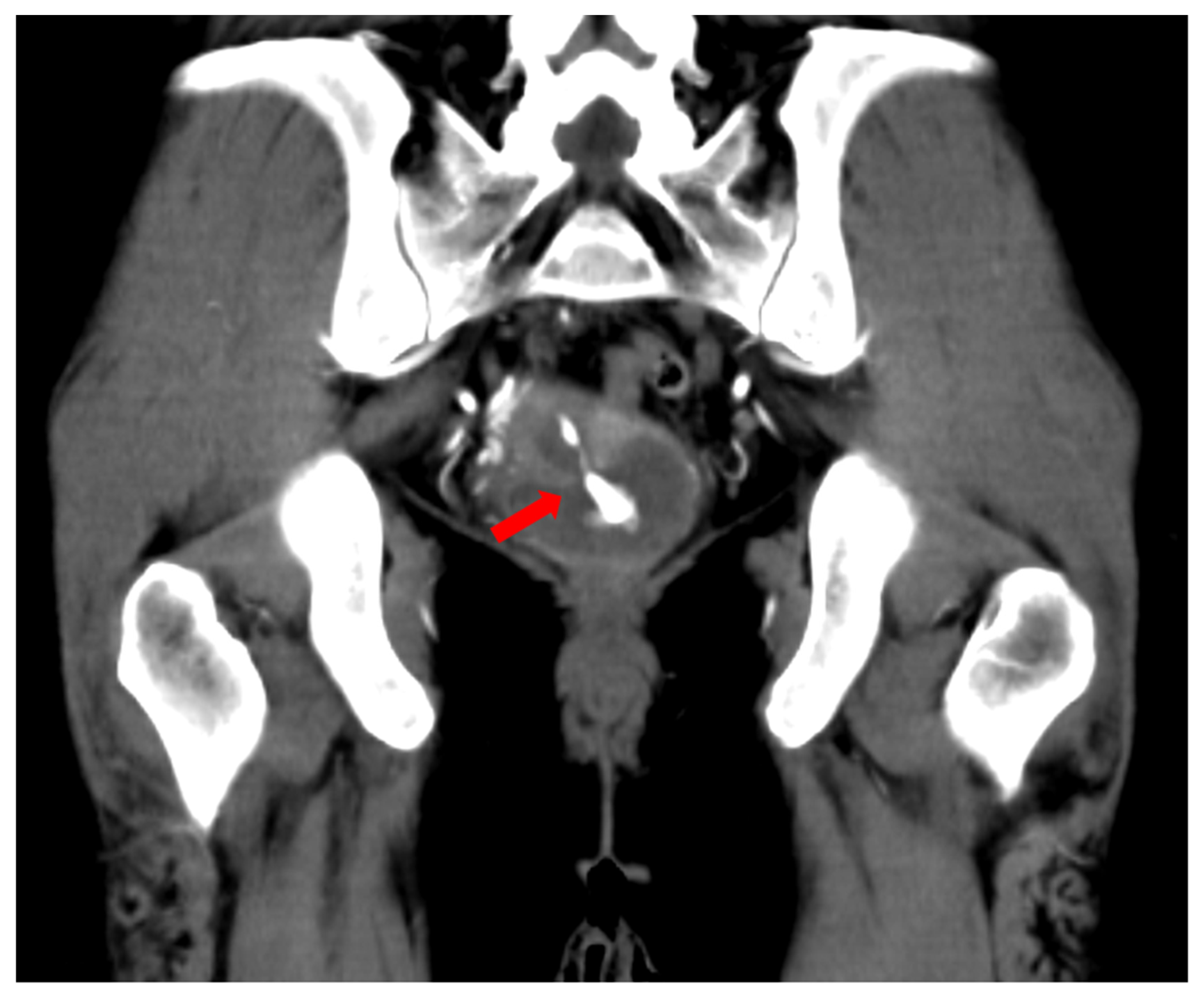
2. Case Presentation
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Bennett, S.J.; Waterstone, J.J.; Cheng, W.C.; Parsons, J. Complications of transvaginal ultrasound-directed follicle aspiration: A review of 2670 consecutive procedures. J Assist. Reprod. Genet. 1993, 10, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Bozdag, G.; Basaran, A.; Cil, B.; Esinler, I.; Yarali, H. An oocyte pick-up procedure complicated with pseudoaneurysm of the internal iliac artery. Fertil. Steril. 2008, 90, 2004.e11–2004.e13. [Google Scholar] [CrossRef] [PubMed]
- Takeda, A.; Koike, W.; Hayashi, S. Delayed hemorrhage as a result of ruptured uterine artery pseudoaneurysm after transmyometrial oocyte retrieval: Management by transcatheter arterial embolization using N-butyl-2-cyanoacrylate. J. Obs. Gynaecol. Res. 2017, 43, 1655–1659. [Google Scholar] [CrossRef] [PubMed]
- Kart, C.; Guven, S.; Aran, T.; Dinc, H. Life-threatening intraabdominal bleeding after oocyte retrieval successfully managed with angiographic embolization. Fertil. Steril. 2011, 96, e99–e102. [Google Scholar] [CrossRef] [PubMed]
- Pappin, C.; Plant, G. A pelvic pseudoaneurysm (a rare complication of oocyte retrieval for IVF) treated by arterial embolization. Hum. Fertil. (Camb) 2006, 9, 153–155. [Google Scholar] [CrossRef] [PubMed]
- Mulkers, A.; Podevyn, K.; Dehaene, I. Recurrent uterine artery pseudo-aneurysm requiring repeat embolization during pregnancy—A case report. Case Rep. Womens Health 2020, 29, e00280. [Google Scholar] [CrossRef] [PubMed]
- Wisanto, A.; Bollen, N.; Camus, M.; De Grauwe, E.; Devroey, P.; Van Steirteghem, A.C. Effect of transuterine puncture during transvaginal oocyte retrieval on the results of human in-vitro fertilization. Hum. Reprod. 1989, 4, 790–793. [Google Scholar] [CrossRef] [PubMed]


| Case | Authors | Age of the Patient (Years) | Past Medical History | Symptoms | The Day Pseudoaneurysm Was Observed | Diagnosis of Pseudoaneurysm | The Injured Artery | The Embolic Material |
|---|---|---|---|---|---|---|---|---|
| 1 | Bozdag et al. [2] | 22 | Nothing | Nothing | 29 weeks of gestation (33 weeks after OR) | US, MRI | Left inferior pudendal artery | NBCA |
| 2 | Takeda et al. [3] | 34 | Four miscarriages | Vaginal bleeding | 7 days after OR | US | Right uterine artery | NBCA |
| 3 | Kart et al. [4] | 40 | Mild factor VIII deficiency | Pain, pale, hypotension | Same day of OR | US | Right and left uterine arteries | PVA |
| 4 | Pappin and Plant [5] | 37 | Not reported | Vaginal bleeding | 12 weeks of gestation (6 years after OR) | US, MRI | Left internal iliac artery | Coils, thrombin |
| 5a * | Mulkers et al. [6] | 35 | Laparoscopy | Pain | 19 weeks and 2 days of gestation | US, MRI | Left uterine artery | Microsphere, gelfoam, coils |
| 5b * | 35 | Laparoscopy | Pain, vaginal bleeding | 30 weeks of gestation | US, MRI | Left uterine artery | Glue | |
| 6 | The present case | 40 | Nothing | Pain, hypotension, vaginal bleeding | Same day of OR | CT | Right pudendal artery | Gelfoam |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tokue, H.; Tokue, A.; Tsushima, Y. Successful Interventional Management of Life-Threatening Bleeding after Oocyte Retrieval: A Case Report and Review of the Literature. Medicina 2022, 58, 1534. https://doi.org/10.3390/medicina58111534
Tokue H, Tokue A, Tsushima Y. Successful Interventional Management of Life-Threatening Bleeding after Oocyte Retrieval: A Case Report and Review of the Literature. Medicina. 2022; 58(11):1534. https://doi.org/10.3390/medicina58111534
Chicago/Turabian StyleTokue, Hiroyuki, Azusa Tokue, and Yoshito Tsushima. 2022. "Successful Interventional Management of Life-Threatening Bleeding after Oocyte Retrieval: A Case Report and Review of the Literature" Medicina 58, no. 11: 1534. https://doi.org/10.3390/medicina58111534
APA StyleTokue, H., Tokue, A., & Tsushima, Y. (2022). Successful Interventional Management of Life-Threatening Bleeding after Oocyte Retrieval: A Case Report and Review of the Literature. Medicina, 58(11), 1534. https://doi.org/10.3390/medicina58111534







