Postpartum Depression Prevalence and Associated Factors: An Observational Study in Saudi Arabia
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5; American Psychiatric Association: Washington, DC, USA, 2013; Volume 5. [Google Scholar]
- Cox, J.; Holden, J. Perinatal Mental Health: A Guide to the Edinburgh Postnatal Depression Scale (EPDS); Royal College of Psychiatrists: London, UK, 2003. [Google Scholar]
- Fan, Q.; Long, Q.; De Silva, V.; Gunarathna, N.; Jayathilaka, U.; Dabrera, T.; Lynn, H.; Østbye, T. Prevalence and risk factors for postpartum depression in Sri Lanka: A population-based study. Asian J. Psychiatry 2020, 47, 101855. [Google Scholar] [CrossRef] [PubMed]
- Adamu, A.F.; Adinew, Y.M. Domestic Violence as a Risk Factor for Postpartum Depression Among Ethiopian Women: Facility Based Study. Clin. Pract. Epidemiol. Ment. Health 2018, 14, 109–119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bauer, N.S.; Ofner, S.; Pottenger, A.; Carroll, A.E.; Downs, S.M. Follow-up of mothers with suspected postpartum depression from pediatrics clinics. Front. Pediatr. 2017, 5, 212. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hartmann, J.M.; Mendoza-Sassi, R.A.; Cesar, J.A. Postpartum depression: Prevalence and associated factors. Cad. De Saude Publica 2017, 33, e00094016. [Google Scholar]
- Hoertel, N.; López, S.; Peyre, H.; Wall, M.M.; González-Pinto, A.; Limosin, F.; Blanco, C. Are symptom features of depression during pregnancy, the postpartum period and outside the peripartum period distinct? Results from a nationally representative sample using item response theory (IRT). Depress. Anxiety 2015, 32, 129–140. [Google Scholar] [CrossRef] [Green Version]
- Al Rawahi, A.; Al Kiyumi, M.H.; Al Kimyani, R.; Al-Lawati, I.; Murthi, S.; Davidson, R.; Al Maniri, A.; Al Azri, M. The effect of antepartum depression on the outcomes of pregnancy and development of postpartum depression: A prospective cohort study of Omani women. Sultan Qaboos Univ. Med. J. 2020, 20, e179. [Google Scholar] [CrossRef]
- Sheela, C.N.; Venkatesh, S. Screening for postnatal depression in a tertiary care hospital. J. Obstet. Gynecol. India 2016, 66, 72–76. [Google Scholar] [CrossRef] [Green Version]
- Bhusal, B.R.; Bhandari, N. Identifying the factors associated with depressive symptoms among postpartum mothers in Kathmandu, Nepal. Int. J. Nurs. Sci. 2018, 5, 268–274. [Google Scholar] [CrossRef]
- Finnbogadóttir, H.; Dykes, A.-K. Increasing prevalence and incidence of domestic violence during the pregnancy and one and a half year postpartum, as well as risk factors:-a longitudinal cohort study in Southern Sweden. BMC Pregnancy Childbirth 2016, 16, 327. [Google Scholar]
- Kettunen, P.; Koistinen, E.; Hintikka, J. The connections of pregnancy-, delivery-, and infant-related risk factors and negative life events on postpartum depression and their role in first and recurrent depression. Depress. Res. Treat. 2016, 2016, 2514317. [Google Scholar] [CrossRef] [Green Version]
- Matijasevich, A.; Munhoz, T.N.; Tavares, B.F.; Barbosa, A.P.P.N.; da Silva, D.M.; Abitante, M.S.; Dall’Agnol, T.A.; Santos, I.S. Validation of the Edinburgh postnatal depression scale (EPDS) for screening of major depressive episode among adults from the general population. BMC Psychiatry 2014, 14, 284. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abdulqader Alrehaili, R.; Albelowi, R. The Prevalence of Postpartum Depression and the Related Risk Factors in Primary Health Care, Al-Madinah, Saudi Arabia. Cureus 2022, 14, e22681. [Google Scholar] [CrossRef] [PubMed]
- Al-Modayfer, O.; Alatiq, Y.; Khair, O.; Abdelkawi, S. Postpartum depression and related risk factors among Saudi females. Int. J. Cult. Ment. Health 2015, 8, 316–324. [Google Scholar] [CrossRef]
- Alsayed, N.A.; Altayyeb, J.F.; Althuniyyan, L.S.; Alzubaidi, S.K.; Farahat, F. Prevalence of Postpartum Depression and Associated Risk Factors Among Women in Jeddah, Western Saudi Arabia. Cureus 2021, 13, e14603. [Google Scholar] [CrossRef] [PubMed]
- Al Nasr, R.S.; Altharwi, K.; Derbah, M.S.; Gharibo, S.O.; Fallatah, S.A.; Alotaibi, S.G.; Almutairi, K.A.; Asdaq, S.M.B. Prevalence and predictors of postpartum depression in Riyadh, Saudi Arabia: A cross sectional study. PLoS ONE 2020, 15, e0228666. [Google Scholar] [CrossRef] [Green Version]
- Alasoom, L.I.; Koura, M.R. Predictors of postpartum depression in the eastern province capital of Saudi Arabia. J. Fam. Med. Prim. Care 2014, 3, 146. [Google Scholar]
- Alharbi, A.A.; Abdulghani, H.M. Risk factors associated with postpartum depression in the Saudi population. Neuropsychiatr. Dis. Treat. 2014, 10, 311. [Google Scholar]
- Gelaye, B.; Rondon, M.B.; Araya, R.; Williams, M.A. Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. Lancet Psychiatry 2016, 3, 973–982. [Google Scholar] [CrossRef] [Green Version]
- Budhathoki, N.; Dahal, M.; Bhusal, S.; Ojha, H.; Pandey, S.; Basnet, S. Violence against women by their husband and postpartum depression. J. Nepal Health Res. Counc. 2012, 10, 176–180. [Google Scholar]
- Nair, L.; Adetayo, O.A. Cultural Competence and Ethnic Diversity in Healthcare. Plast. Reconstr. Surg. Glob. Open 2019, 7, e2219. [Google Scholar] [CrossRef]
- Wang, Z.; Liu, J.; Shuai, H.; Cai, Z.; Fu, X.; Liu, Y.; Xiao, X.; Zhang, W.; Krabbendam, E.; Liu, S. Mapping global prevalence of depression among postpartum women. Transl. Psychiatry 2021, 11, 543. [Google Scholar] [CrossRef] [PubMed]
- Lanes, A.; Kuk, J.L.; Tamim, H. Prevalence and characteristics of postpartum depression symptomatology among Canadian women: A cross-sectional study. BMC Public Health 2011, 11, 302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fisher, J.; Mello, M.C.d.; Patel, V.; Rahman, A.; Tran, T.; Holton, S.; Holmes, W. Prevalence and determinants of common perinatal mental disorders in women in low-and lower-middle-income countries: A systematic review. Bull. World Health Organ. 2012, 90, 139–149. [Google Scholar]
- Alshikh Ahmad, H.; Alkhatib, A.; Luo, J. Prevalence and risk factors of postpartum depression in the Middle East: A systematic review and meta–analysis. BMC Pregnancy Childbirth 2021, 21, 542. [Google Scholar] [CrossRef]
- James-Hawkins, L.; Shaltout, E.; Nur, A.A.; Nasrallah, C.; Qutteina, Y.; Abdul Rahim, H.F.; Hennink, M.; Yount, K.M. Human and economic resources for empowerment and pregnancy-related mental health in the Arab Middle East: A systematic review. Arch. Women’s Ment. Health 2019, 22, 1–14. [Google Scholar] [CrossRef]
- Almutairi, A.; McCarthy, A. A multicultural nursing workforce and cultural perspectives in Saudi Arabia: An overview. TheHealth 2012, 3, 71–74. [Google Scholar]
- Karout, N.; Abdelaziz, S.; Goda, M.; AlTuwaijri, S.; Almostafa, N.; Ashour, R.; Alradi, H. Cultural diversity: A qualitative study on Saudi Arabian women’s experience and perception of maternal health services. J. Nurs. Educ. Pract. 2013, 3, 172–182. [Google Scholar] [CrossRef]
- Ghubash, R.; Abou-Saleh, M.T.; Daradkeh, T.K. The validity of the Arabic Edinburgh postnatal depression scale. Soc. Psychiatry Psychiatr. Epidemiol. 1997, 32, 474–476. [Google Scholar] [CrossRef]
- Naja, S.; Al-Kubaisi, N.; Chehab, M.; Al-Dahshan, A.; Abuhashem, N.; Bougmiza, I. Psychometric properties of the Arabic version of EPDS and BDI-II as a screening tool for antenatal depression: Evidence from Qatar. BMJ Open 2019, 9, e030365. [Google Scholar]
- Khalifa, D.S.; Glavin, K.; Bjertness, E.; Lien, L. Postnatal depression among Sudanese women: Prevalence and validation of the Edinburgh Postnatal Depression Scale at 3 months postpartum. Int. J. Women’s Health 2015, 7, 677. [Google Scholar] [CrossRef] [Green Version]
- Statistics GAF. GASTAT Releases the Results of the Household’s Income and Expenditure Survey. 2018. Available online: https://www.stats.gov.sa/en/node/53971 (accessed on 28 October 2022).
- Mughal, S.; Azhar, Y.; Siddiqui, W. Postpartum Depression; StatPearls: Treasure Island, FL, USA, 2021. [Google Scholar]
- Al Hinai, F.I.; Al Hinai, S.S. Prospective study on prevalence and risk factors of postpartum depression in Al-dakhliya governorate in oman. Oman Med. J. 2014, 29, 198–202. [Google Scholar] [CrossRef] [PubMed]
- Turkcapar, A.F.; Kadıoğlu, N.; Aslan, E.; Tunc, S.; Zayıfoğlu, M.; Mollamahmutoğlu, L. Sociodemographic and clinical features of postpartum depression among Turkish women: A prospective study. BMC Pregnancy Childbirth 2015, 15, 108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yamamoto, N.; Abe, Y.; Arima, K.; Nishimura, T.; Akahoshi, E.; Oishi, K.; Aoyagi, K. Mental health problems and influencing factors in Japanese women 4 months after delivery. J. Physiol. Anthropol. 2014, 33, 32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pham, D.; Cormick, G.; Amyx, M.M.; Gibbons, L.; Doty, M.; Brown, A.; Norwood, A.; Daray, F.M.; Althabe, F.; Belizán, J.M. Factors associated with postpartum depression in women from low socioeconomic level in Argentina: A hierarchical model approach. J. Affect. Disord. 2018, 227, 731–738. [Google Scholar] [CrossRef] [PubMed]
- Maita, H.; Kobayashi, T.; Osawa, H. Postpartum depression and health related quality of life: A necessary assessment. Int. J. Fam. Commun. Med. 2017, 1, 11–17. [Google Scholar]
- Rus Prelog, P.; Vidmar Šimic, M.; Premru Sršen, T.; Rus Makovec, M. Contextual-relationship and stress-related factors of postpartum depression symptoms in nulliparas: A prospective study from Ljubljana, Slovenia. Reprod. Health 2019, 16, 145. [Google Scholar] [CrossRef] [Green Version]
- Hahn-Holbrook, J.; Cornwell-Hinrichs, T.; Anaya, I. Economic and Health Predictors of National Postpartum Depression Prevalence: A Systematic Review, Meta-analysis, and Meta-Regression of 291 Studies from 56 Countries. Front. Psychiatry 2018, 8, 248. [Google Scholar] [CrossRef] [Green Version]
- Tannous, L.; Gigante, L.P.; Fuchs, S.C.; Busnello, E.D.A. Postnatal depression in Southern Brazil: Prevalence and its demographic and socioeconomic determinants. BMC Psychiatry 2008, 8, 1. [Google Scholar]
- Miyake, Y.; Tanaka, K.; Sasaki, S.; Hirota, Y. Employment, income, and education and risk of postpartum depression: The Osaka Maternal and Child Health Study. J. Affect. Disord. 2011, 130, 133–137. [Google Scholar] [CrossRef]
- Silverman, M.E.; Reichenberg, A.; Savitz, D.A.; Cnattingius, S.; Lichtenstein, P.; Hultman, C.M.; Larsson, H.; Sandin, S. The risk factors for postpartum depression: A population-based study. Depress. Anxiety 2017, 34, 178–187. [Google Scholar] [CrossRef]
- Suhitharan, T.; Pham, T.P.; Chen, H.; Assam, P.N.; Sultana, R.; Han, N.L.; Tan, E.C.; Sng, B.L. Investigating analgesic and psychological factors associated with risk of postpartum depression development: A case-control study. Neuropsychiatr. Dis. Treat. 2016, 12, 1333–1339. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moameri, H.; Ostadghaderi, M.; Khatooni, E.; Doosti-Irani, A. Association of postpartum depression and cesarean section: A systematic review and meta-analysis. Clin. Epidemiol. Glob. Health 2019, 7, 471–480. [Google Scholar] [CrossRef] [Green Version]
- Xie, R.-H.; Lei, J.; Wang, S.; Xie, H.; Walker, M.; Wen, S.W. Cesarean section and postpartum depression in a cohort of Chinese women with a high cesarean delivery rate. J. Women’s Health 2011, 20, 1881–1886. [Google Scholar] [CrossRef] [PubMed]
- Almutairi, A.F.; Salam, M.; Alanazi, S.; Alweldawi, M.; Alsomali, N.; Alotaibi, N. Impact of help-seeking behavior and partner support on postpartum depression among Saudi women. Neuropsychiatr. Dis. Treat. 2017, 13, 1929–1936. [Google Scholar] [CrossRef] [Green Version]
- Shorey, S.; Ing, C.; Ng, E.; Chan, Y.; Tam, W.; Chong, Y.-S. Prevalence and incidence of postpartum depression among healthy mothers: A systematic review and meta-analysis. J. Psychiatr. Res. 2018, 104, 235–248. [Google Scholar] [CrossRef]
- Arifin, S.R.M.; Cheyne, H.; Maxwell, M. Review of the prevalence of postnatal depression across cultures. AIMS Public Health 2018, 5, 260. [Google Scholar]
| Characteristics | Normal n (%) | Positive for PPD n (%) |
|---|---|---|
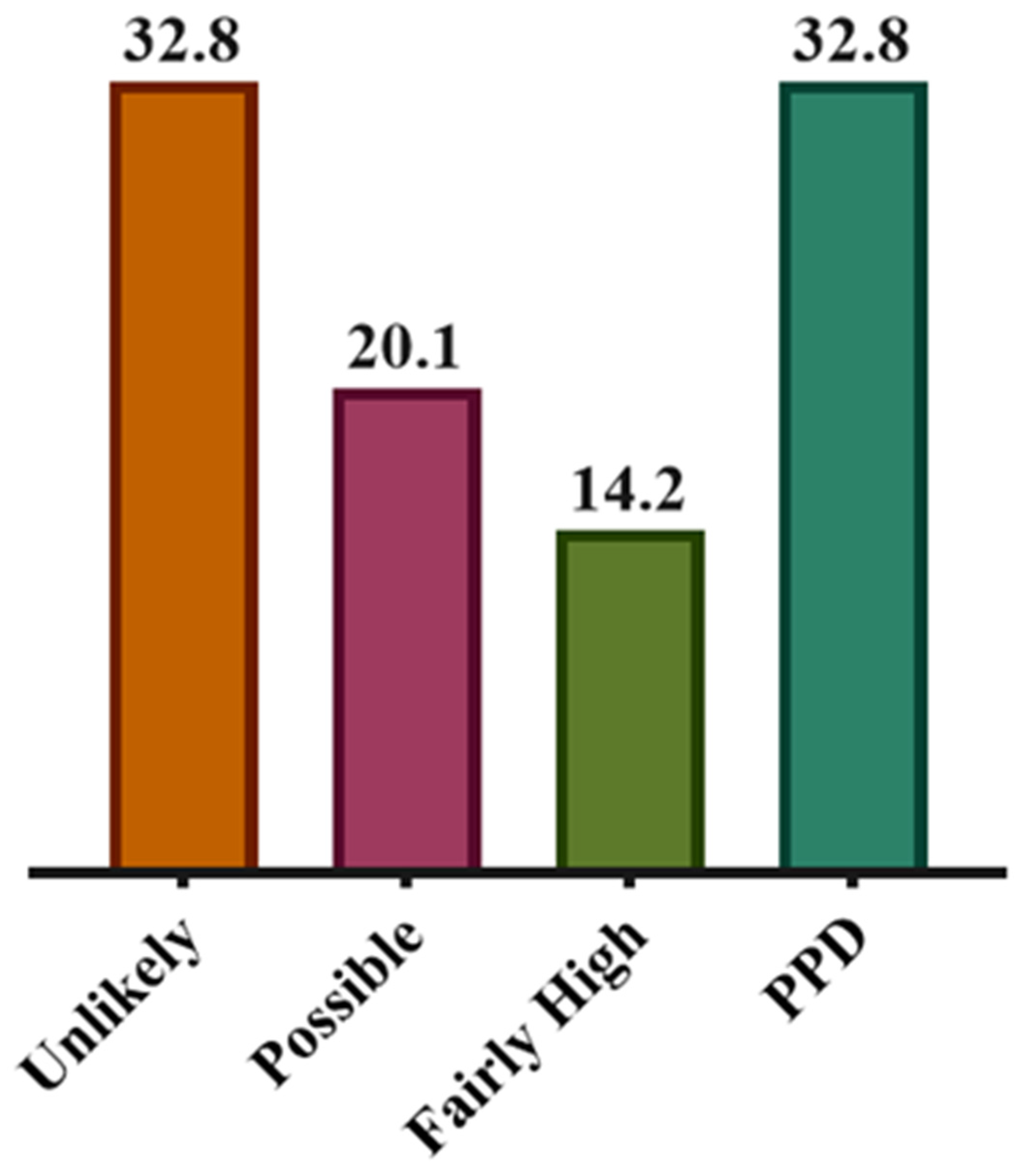
| Total | 264 (67.2) | 129 (32.8) |
| Age, Years (Mean ± SD) | 32.43 ± 7.42 | 33.00 ± 7.72 |
| Age Distribution, Years | ||
| <30 | 84 (35.3) | 33 (32.7) |
| ≥30 | 154 (64.7) | 68 (67.3) |
| Comorbidity | ||
| No | 206 (79.5) | 89 (71.2) |
| Yes | 53 (20.5) | 36 (28.8) |
| Previous Depression Diagnosis | ||
| No | 240 (94.9) | 101 (79.5) |
| Yes | 13 (5.1) | 26 (20.5) |
| Marital Status | ||
| Married | 239 (91.6) | 114 (89.8) |
| Divorced | 18 (6.9) | 9 (7.1) |
| Widowed | 4 (1.5) | 4 (3.1) |
| Education | ||
| College/University/Higher | 118 (44.9) | 52 (40.6) |
| High School | 92 (35.0) | 34 (26.6) |
| Middle School | 40 (15.2) | 22 (17.2) |
| Primary School | 13 (4.9) | 20 (15.6) |
| Employment | ||
| Employed | 111 (42.7) | 40 (31.3) |
| Unemployed | 149 (57.3) | 88 (68.7) |
| Income, SAR * | ||
| >10,000 | 80 (30.8) | 32 (25.2) |
| <5000 | 122 (46.9) | 54 (42.5) |
| 5000–10,000 | 58 (22.3) | 41 (32.3) |
| Feeding Status | ||
| Breastfeed | 49 (20.2) | 35 (28.9) |
| Bottle Feed | 68 (28.1) | 35 (28.9) |
| Both | 125 (51.7) | 51 (42.2) |
| Planned Pregnancy | ||
| Yes | 104 (41.8) | 51 (42.5) |
| No | 145 (58.2) | 69 (57.5) |
| Delivery Disposition | ||
| Normal | 190 (76.9) | 77 (63.1) |
| C-Section | 57 (23.1) | 45 (36.9) |
| Last Baby Gender | ||
| Male | 122 (49.8) | 72 (58.1) |
| Female | 123 (50.2) | 52 (41.9) |
| No. of Pregnancies | ||
| 1–2 | 91 (37.0) | 32 (26.9) |
| 3–5 | 113 (45.9) | 61 (51.3) |
| >5 | 42 (17.1) | 26 (21.8) |
| Characteristics | OR (95% CI) | p Value |
|---|---|---|
| Age Distribution, Years | ||
| <30 | Reference | |
| ≥30 | 1.124 (0.686–1.841) | 0.643 |
| Comorbidity | ||
| No | Reference | |
| Yes | 1.572 (0.962–2.569) | 0.071 |
| Previous Depression Diagnosis | ||
| No | Reference | |
| Yes | 4.752 (2.348–9.620) | <0.0001 |
| Marital Status | ||
| Married | Reference | |
| Divorced | 1.048 (0.457–2.406) | 0.911 |
| Widowed | 2.096 (0.515–8.534) | 0.301 |
| Education | ||
| College/University/Higher | Reference | |
| High School | 0.839 (0.503–1.398) | 0.500 |
| Middle School | 1.248 (0.675–2.306) | 0.479 |
| Primary School | 3.491 (1.615–7.545) | 0.001 |
| Employment | ||
| Employed | Reference | |
| Unemployed | 1.639 (1.048–2.563) | 0.030 |
| Income, SAR * | ||
| >10,000 | Reference | |
| <5000 | 1.107 (0.658–1.862) | 0.703 |
| 5000–10,000 | 1.767 (0.997–3.133) | 0.051 |
| Feeding Status | ||
| Breastfeed | Reference | |
| Bottle Feed | 0.721 (0.397–1.307) | 0.281 |
| Both | 0.571 (0.332–0.983) | 0.043 |
| Planned Pregnancy | ||
| Yes | Reference | |
| No | 0.970 (0.624–1.508) | 0.894 |
| Delivery Disposition | ||
| Normal | Reference | |
| C-Section | 1.948 (1.215–3.123) | 0.006 |
| Last Baby Gender | ||
| Male | Reference | |
| Female | 0.716 (0.463–1.108) | 0.134 |
| No. of Pregnancies | ||
| 1–2 | Reference | |
| 3–5 | 1.535 (0.923–2.554) | 0.099 |
| >5 | 1.760 (0.934–3.317) | 0.080 |
| Characteristics | OR (95% CI) | p Value |
|---|---|---|
| Previous Depression Diagnosis | ||
| No | Reference | |
| Yes | 3.817 (1.751–8.320) | 0.001 |
| Education | ||
| College/University/Higher | Reference | |
| High School | 0.671 (0.376–1.197) | 0.177 |
| Middle School | 0.945 (0.468–1.909) | 0.876 |
| Primary School | 2.595 (1.104–6.103) | 0.029 |
| Employment | ||
| Employed | Reference | |
| Unemployed | 1.910 (1.142–3.196) | 0.014 |
| Feeding Status | ||
| Breastfeed | Reference | |
| Bottle Feed | 0.768 (0.397–1.487) | 0.434 |
| Both | 0.564 (0.308–1.033) | 0.064 |
| Delivery Disposition | ||
| Normal | Reference | |
| C-Section | 2.342 (1.380–3.975) | 0.002 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alzahrani, J.; Al-Ghamdi, S.; Aldossari, K.; Al-Ajmi, M.; Al-Ajmi, D.; Alanazi, F.; Aldossary, A.; Alharbi, A. Postpartum Depression Prevalence and Associated Factors: An Observational Study in Saudi Arabia. Medicina 2022, 58, 1595. https://doi.org/10.3390/medicina58111595
Alzahrani J, Al-Ghamdi S, Aldossari K, Al-Ajmi M, Al-Ajmi D, Alanazi F, Aldossary A, Alharbi A. Postpartum Depression Prevalence and Associated Factors: An Observational Study in Saudi Arabia. Medicina. 2022; 58(11):1595. https://doi.org/10.3390/medicina58111595
Chicago/Turabian StyleAlzahrani, Jamaan, Sameer Al-Ghamdi, Khaled Aldossari, Mansour Al-Ajmi, Dhafer Al-Ajmi, Faisal Alanazi, Abdullah Aldossary, and Ahmed Alharbi. 2022. "Postpartum Depression Prevalence and Associated Factors: An Observational Study in Saudi Arabia" Medicina 58, no. 11: 1595. https://doi.org/10.3390/medicina58111595
APA StyleAlzahrani, J., Al-Ghamdi, S., Aldossari, K., Al-Ajmi, M., Al-Ajmi, D., Alanazi, F., Aldossary, A., & Alharbi, A. (2022). Postpartum Depression Prevalence and Associated Factors: An Observational Study in Saudi Arabia. Medicina, 58(11), 1595. https://doi.org/10.3390/medicina58111595






