Vasovagal Syncope during Office Hysteroscopy—A Frequently Overlooked Unpleasant Complication
Abstract
:1. Introduction
2. Purpose
3. Pathophysiology
4. Risk Factors
5. Diagnosis
6. Acute Management
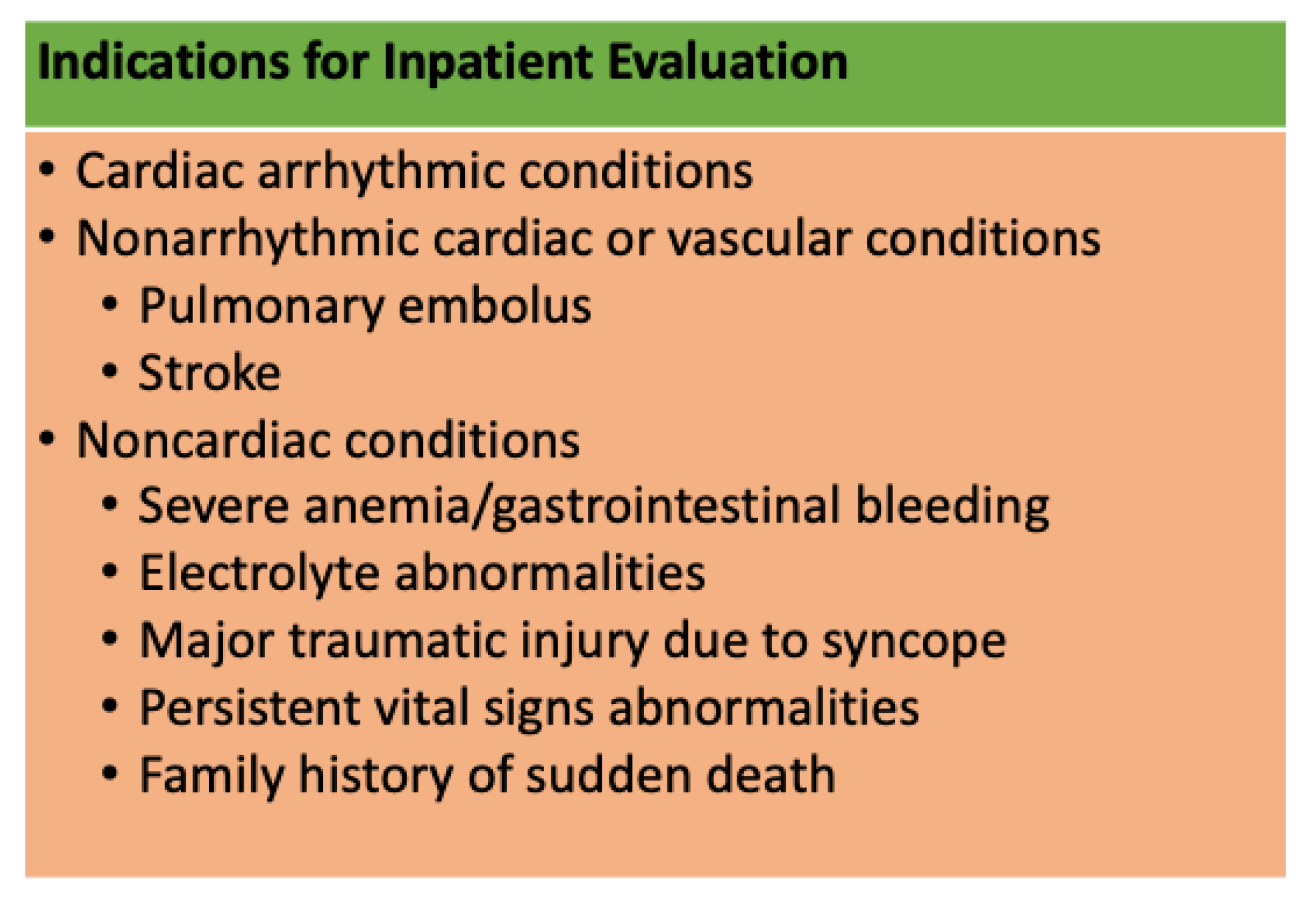
7. Risk Stratification–When to Send to Emergency Department?
8. Severe Complications
9. Summary
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Steiner, C.A.; Karaca, Z.; Moore, B.J.; Imshaug, M.C.; Pickens, G. Surgeries in Hospital-Based Ambulatory Surgery and Hospital Inpatient Settings 2014; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2017.
- Urman, R.D.; Punwani, N.; Shapiro, F.E. Office-based surgical and medical procedures: Educational gaps. Ochsner J. 2012, 12, 383–388. [Google Scholar]
- Amer-Cuenca, J.J.; Marín-Buck, A.; Vitale, S.G.; La Rosa, V.L.; Caruso, S.; Cianci, A.; Lisón, J.F. Non-pharmacological pain control in outpatient hysteroscopies. Minim. Invasive Ther. Allied Technol. 2020, 29, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Salazar, C.A.; Isaacson, K.B. Office Operative Hysteroscopy: An Update. J. Minim. Invasive Gynecol. 2018, 25, 199–208. [Google Scholar] [CrossRef] [PubMed]
- American College of Obstetricians and Gynecologists. The Use of Hysteroscopy for the Diagnosis and Treatment of Intrauterine Pathology: ACOG Committee Opinion, Number 800. Obs. Gynecol. 2020, 135, e138–e148. [Google Scholar] [CrossRef] [PubMed]
- Radvansky, B.M.; Husain, Q.; Cherla, D.V.; Choudhry, O.J.; Eloy, J.A. In-office vasovagal response after rhinologic manipulation. Int. Forum Allergy Rhinol. 2013, 3, 510–514. [Google Scholar] [CrossRef]
- He, Y.; Geng, Q.; Liu, H.; Han, X. First Experience Using 4-Dimensional Hysterosalpingo-Contrast Sonography with SonoVue for Assessing Fallopian Tube Patency. J. Ultrasound Med. 2013, 32, 1233–1243. [Google Scholar] [CrossRef]
- Ma, T.; Readman, E.; Hicks, L.; Porter, J.; Cameron, M.; Ellett, L.; Mcilwaine, K.; Manwaring, J.; Maher, P. Is outpatient hysteroscopy the new gold standard? Results from an 11 year prospective observational study. Aust. N. Z. J. Obstet. Gynaecol. 2017, 57, 74–80. [Google Scholar] [CrossRef]
- Carin, A.J.; Garbin, O. Intra uterine devices removal during office hysteroscopy: About 36 cases. J. Gynecol. Obs. Biol. Reprod. 2015, 44, 653–657. [Google Scholar] [CrossRef]
- Lo, K.W.; Yuen, P. The Role of Outpatient Diagnostic Hysteroscopy in Identifying Anatomic Pathology and Histopathology in the Endometrial Cavity. J. Am. Assoc. Gynecol. Laparosc. 2000, 7, 381–385. [Google Scholar] [CrossRef]
- Shen, W.K.; Sheldon, R.S.; Benditt, D.G.; Cohen, M.I.; Forman, D.E.; Goldberger, Z.D.; Grubb, B.P.; Hamdan, M.H.; Krahn, A.D.; Link, M.S.; et al. 2017 ACC/AHA/HRS Guideline for the Evaluation and Management of Patients with Syncope: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J. Am. Coll. Cardiol. 2017, 70, e39–e110. [Google Scholar] [CrossRef]
- Sheldon, R.S.; Grubb, B.P.; Olshansky, B.; Shen, W.K.; Calkins, H.; Brignole, M.; Raj, S.R.; Krahn, A.D.; Morillo, C.A.; Stewart, J.M.; et al. 2015 heart rhythm society expert consensus statement on the diagnosis and treatment of postural tachy-cardia syndrome, inappropriate sinus tachycardia, and vasovagal syncope. Heart Rhythm. 2015, 12, e41–e63. [Google Scholar] [CrossRef] [PubMed]
- Folino, A.F.; Russo, G.; Buja, G.; Iliceto, S. Contribution of Decreased Atrial Function in the Pathogenesis of Neurally Mediated Syncope. Am. J. Cardiol. 2006, 97, 1017–1024. [Google Scholar] [CrossRef]
- Brignole, M. Vasovagal syncope and vasovagal disease. Hell. J. Cardiol. 2008, 49, 61–64. [Google Scholar]
- Alboni, P.; Brignole, M.; Uberti, E.C.D. Is vasovagal syncope a disease? Europace 2007, 9, 83–87. [Google Scholar] [CrossRef] [PubMed]
- Fenton, A.M.; Hammill, S.C.; Rea, R.F.; Low, P.A.; Shen, W.K. Vasovagal syncope. Ann. Intern. Med. 2000, 133, 714–725. [Google Scholar] [CrossRef]
- Folino, A.F.; Russo, G.; Porta, A.; Buja, G.; Cerutti, S.; Iliceto, S. Modulations of autonomic activity leading to tilt-mediated syncope. Int. J. Cardiol. 2007, 120, 102–107. [Google Scholar] [CrossRef] [PubMed]
- Aydin, M.A.; Salukhe, T.V.; Wilke, I.; Willems, S. Management and therapy of vasovagal syncope: A review. World J. Cardiol. 2010, 2, 308–315. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agostini, A.; Bretelle, F.; Ronda, I.; Roger, V.; Cravello, L.; Blanc, B. Risk of Vasovagal Syndrome During Outpatient Hysteroscopy. J. Am. Assoc. Gynecol. Laparosc. 2004, 11, 245–247. [Google Scholar] [CrossRef]
- Cicinelli, E.; Didonna, T.; Ambrosi, G.; Schonauer, L.M.; Fiore, G.; Matteo, M.G. Topical anaesthesia for diagnostic hysteroscopy and endometrial biopsy in postmenopausal women: A randomised placebo-controlled double-blind study. BJOG: Int. J. Obstet. Gynaecol. 1997, 104, 316–319. [Google Scholar] [CrossRef]
- Newman, B. Vasovagal reactions in high school students: Findings relative to race, risk factor synergism, female sex, and non-high school particpants. Transfusion 2002, 42, 1557–1560. [Google Scholar] [CrossRef]
- Newman, B.H. Vasovagal reaction rates and body weight: Findings in high- and low-risk populations. Transfusion 2003, 43, 1084–1088. [Google Scholar] [CrossRef] [PubMed]
- Takanashi, M.; Odajima, T.; Aota, S.; Sudoh, M.; Yamaga, Y.; Ono, Y.; Yoshinaga, K.; Motoji, T.; Matsuzaki, K.; Satake, M.; et al. Risk factor analysis of vasovagal reaction from blood donation. Transfus. Apher. Sci. 2012, 47, 319–325. [Google Scholar] [CrossRef] [PubMed]
- Thijsen, A.; Masser, B. Vasovagal reactions in blood donors: Risks, prevention and management. Transfus. Med. 2019, 29, 13–22. [Google Scholar] [CrossRef] [PubMed]
- Vidri, R.; Emerick, T.; Alter, B.; Brancolini, S. Managing Vasovagal Reactions in the Outpatient Pain Clinic Setting: A Review for Pain Medicine Physicians Not Trained in Anesthesiology. Pain Med. 2022, 23, 1189–1193. [Google Scholar] [CrossRef]
- Kamar, S.; Hallit, S.; Chamandi, S. Vasovagal syncope related to pain procedures in a pain clinic at a tertiary Lebanese hospital between 2016 and 2019. BMC Res. Notes 2021, 14, 133. [Google Scholar] [CrossRef]
- Serletis, A.; Rose, S.; Sheldon, A.G. Vasovagal syncope in medical students and their first-degree relatives. Eur. Heart J. 2006, 27, 1965–1970. [Google Scholar] [CrossRef] [Green Version]
- Sheldon, R. Syncope Diagnostic Scores. Prog. Cardiovasc. Dis. 2013, 55, 390–395. [Google Scholar] [CrossRef]
- Kaufmann, H. Neurally mediated syncope: Pathogenesis, diagnosis, and treatment. Neurology 1995, 45, S12–S18. [Google Scholar]
- Freeman, R.; Wieling, W.; Axelrod, F.B.; Benditt, D.G.; Benarroch, E.; Biaggioni, I.; Cheshire, W.; Chelimsky, T.; Cortelli, P.; Gibbons, C.H.; et al. Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Auton. Neurosci. 2011, 161, 46–48. [Google Scholar] [CrossRef]
- Wieling, W.; Thijs, R.D.; Van Dijk, N.; Wilde, A.A.M.; Benditt, D.G.; Van Dijk, J.G. Symptoms and signs of syncope: A review of the link between physiology and clinical clues. Brain 2009, 132 Pt 10, 2630–2642. [Google Scholar] [CrossRef]
- Edholm, O.G. Physiological Changes during Fainting. In Visceral Circulation; Ciba Foundation Symposium: London, UK, 1952. [Google Scholar]
- Romme, J.J.C.M.; Van Dijk, N.; Boer, K.R.; Dekker, L.R.C.; Stam, J.; Reitsma, J.B.; Wieling, W. Influence of age and gender on the occurrence and presentation of reflex syncope. Clin. Auton. Res. 2008, 18, 127–133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Newman, B.H.; Graves, S. A study of 178 consecutive vasovagal syncopal reactions from the perspective of safety. Transfusion 2001, 41, 1475–1479. [Google Scholar] [CrossRef] [PubMed]
- Parry, S.W.; Tan, M.P. An approach to the evaluation and management of syncope in adults. BMJ 2010, 340, c880. [Google Scholar] [CrossRef]
- Gauer, R.L. Evaluation of syncope. Am. Fam. Physician 2011, 84, 640–650. [Google Scholar] [PubMed]
- Krediet, C.; Van Dijk, N.; Linzer, M.; Van Lieshout, J.; Wieling, W. Management of vasovagal syncope, controlling or aborting faints by leg crossing and muscle tensing. Circulation 2002, 106, 1684–1689. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van Dijk, N.; Quartieri, F.; Blanc, J.J.; Garcia-Civera, R.; Brignole, M.; Moya, A.; Wieling, W.; PC-Trial Investigators. Effectiveness of physical counterpressure maneuvers in preventing vasovagal syncope: The Physical Counterpressure Manoeuvres Trial (PC-Trial). J. Am. Coll. Cardiol. 2006, 48, 1652–1657. [Google Scholar] [CrossRef] [Green Version]
- Jensen, J.L.; Ohshimo, S.; Cassan, P.; Meyran, D.; Greene, J.; Ng, K.C.; Singletary, E.; Zideman, D.; on behalf of the First Aid and Pediatric Task Forces of the International Liaison Committee on Resuscitation. Immediate Interventions for Presyncope of Vasovagal or Orthostatic Origin: A Systematic Review. Prehospital Emerg. Care 2020, 24, 64–76. [Google Scholar] [CrossRef]
- del Valle, C.S.; Rodriguez, A.; Alonso, M. Pain management in outpatient hysteroscopy. Gynecol. Minim. Invasive Ther. 2016, 5, 141–147. [Google Scholar] [CrossRef] [Green Version]
- Povedano, B.; Arjona, J.E.; Velasco, E.; Monserrat, J.A.; Lorente, J.; Castelo-Branco, C. Complications of hysteroscopic Essure((R)) sterilisation: Report on 4306 procedures performed in a single centre. BJOG 2012, 119, 795–799. [Google Scholar] [CrossRef]
- Ouyang, H.; Quinn, J. Diagnosis and Evaluation of Syncope in the Emergency Department. Emerg. Med. Clin. N. Am. 2010, 28, 471–485. [Google Scholar] [CrossRef]
- Moya, A.; Sutton, R.; Ammirati, F.; Blanc, J.-J.; Brignole, M.; Dahm, J.B.; Deharo, J.-C.; Gajek, J.; Gjesdal, K.; Krahn, A.; et al. Guidelines for the diagnosis and management of syncope (version 2009). Eur. Heart J. 2009, 30, 2631–2671. [Google Scholar] [PubMed] [Green Version]
- Solbiati, M.; Casazza, G.; Dipaola, F.; Rusconi, A.M.; Cernuschi, G.; Barbic, F.; Montano, N.; Sheldon, R.S.; Furlan, R.; Costantino, G. Syncope recurrence and mortality: A systematic review. Eurpace 2015, 17, 300–308. [Google Scholar] [CrossRef] [PubMed]
- Pournazari, P.; Sahota, I.; Sheldon, R. High Remission Rates in Vasovagal Syncope: Systematic Review and Meta-Analysis of Observational and Randomized Studies. JACC Clin. Electrophysiol. 2017, 3, 384–392. [Google Scholar] [CrossRef] [PubMed]
- Soteriades, E.S.; Evans, J.C.; Larson, M.G.; Chen, M.H.; Chen, L.; Benjamin, E.J.; Levy, D. Incidence and Prognosis of Syncope. N. Engl. J. Med. 2002, 347, 878–885. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodriguez, S.; Haimovich, S.; Vitale, S.G.; Alonso, L.; Carugno, J. Vasovagal Syncope during Office Hysteroscopy—A Frequently Overlooked Unpleasant Complication. Medicina 2022, 58, 1626. https://doi.org/10.3390/medicina58111626
Rodriguez S, Haimovich S, Vitale SG, Alonso L, Carugno J. Vasovagal Syncope during Office Hysteroscopy—A Frequently Overlooked Unpleasant Complication. Medicina. 2022; 58(11):1626. https://doi.org/10.3390/medicina58111626
Chicago/Turabian StyleRodriguez, Suset, Sergio Haimovich, Salvatore Giovanni Vitale, Luis Alonso, and Jose Carugno. 2022. "Vasovagal Syncope during Office Hysteroscopy—A Frequently Overlooked Unpleasant Complication" Medicina 58, no. 11: 1626. https://doi.org/10.3390/medicina58111626
APA StyleRodriguez, S., Haimovich, S., Vitale, S. G., Alonso, L., & Carugno, J. (2022). Vasovagal Syncope during Office Hysteroscopy—A Frequently Overlooked Unpleasant Complication. Medicina, 58(11), 1626. https://doi.org/10.3390/medicina58111626