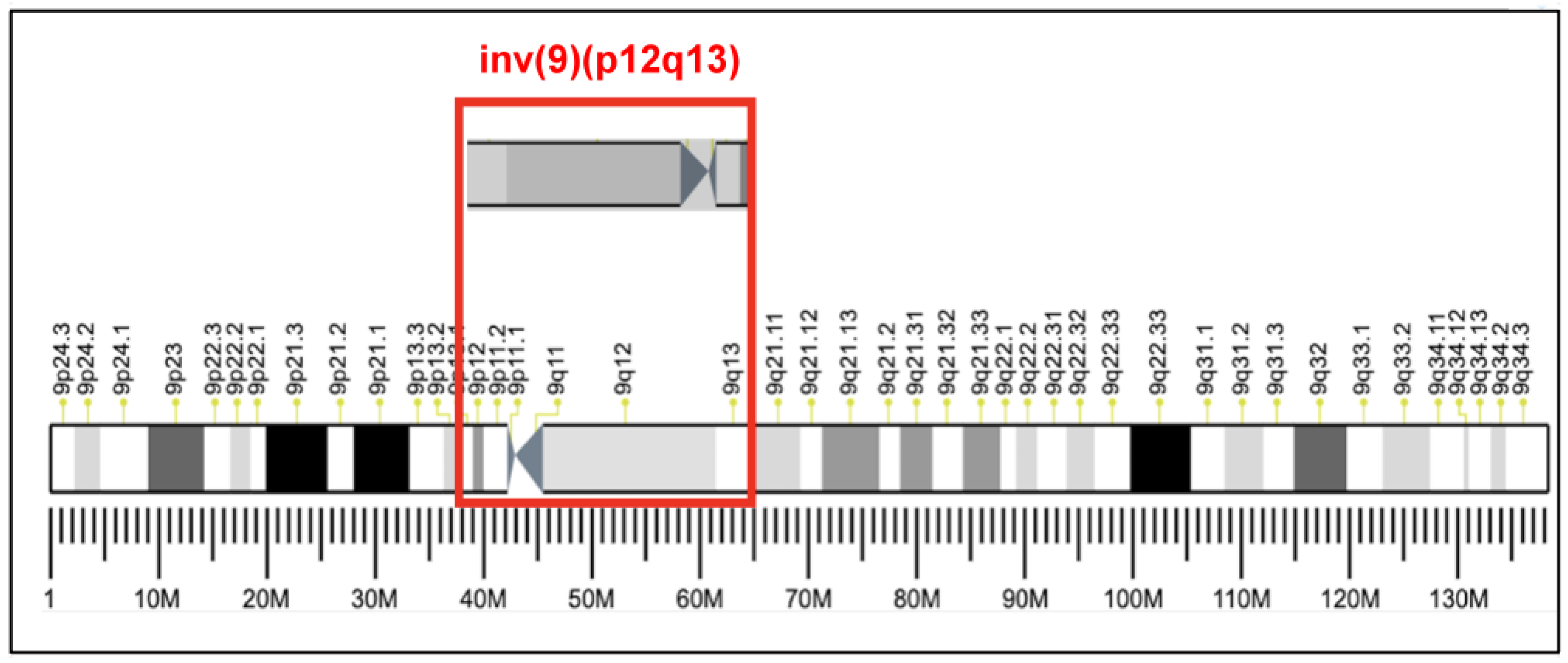
Successful Live Twin Birth through IVF/ICSI from a Couple with an Infertile Father with Pericentric Inversion of Chromosome 9 (p12q13): A Case with a High Aneuploidy Rate
Abstract
:1. Introduction
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Li, S.-J.; Cheng, Y.-X.; Shang, Y.; Zhou, D.-N.; Zhang, Y.; Yin, T.-L.; Yang, J. Chromosomal polymorphisms associated with reproductive outcomes after IVF-ET. J. Assist. Reprod. Genet. 2020, 37, 1703–1710. [Google Scholar] [CrossRef] [PubMed]
- Šípek, A.; Panczak, A.; Mihalová, R.; Hrčková, L.; Suttrová, E.; Sobotka, V.; Lonský, P.; Kaspříková, N.; Gregor, V. Pericentric inversion of human chromosome 9 epidemiology study in Czech males and females. Folia Biol. 2015, 61, 140–146. [Google Scholar]
- Schaffer, L.G.; McGowan-Jordan, J.; Schmid, M. (Eds.) ISCN 2013: An International System for Human Cytogenetic Nomenclature; Karger: Basel, Switzerland, 2012. [Google Scholar]
- Mozdarani, H.; Meybodi, A.M.; Karimi, H. Impact of pericentric inversion of Chromosome 9 [inv (9) (p11q12)] on infertility. Indian J. Hum. Genet. 2007, 13, 26–29. [Google Scholar] [CrossRef] [Green Version]
- Kumar, M.; Thatai, A.; Chapadgaonkar, S.S. Homozygosity and heterozygosity of the pericentric inversion of chromosome 9 and its clinical impact. J. Clin. Diagn. Res. 2012, 6, 816–820. [Google Scholar] [CrossRef]
- Tho, S.P.; Byrd, J.R.; McDonough, P.G. Chromosome polymorphism in 110 couples with reproductive failure and subsequent pregnancy outcome. Fertil. Steril. 1982, 38, 688–694. [Google Scholar] [CrossRef]
- Dana, M.; Stoian, V. Association of pericentric inversion of chromosome 9 and infertility in romanian population. Maedica 2012, 7, 25–29. [Google Scholar] [PubMed]
- Kosyakova, N.; Grigorian, A.; Liehr, T.; Manvelyan, M.; Simonyan, I.; Mkrtchyan, H.; Aroutiounian, R.; Polityko, A.D.; Kulpanovich, A.I.; Egorova, T.; et al. Heteromorphic variants of chromosome 9. Mol. Cytogenet. 2013, 6, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Young, D.; Klepacka, D.; McGarvey, M.; Schoolcraft, W.B.; Katz-Jaffe, M.G. Infertility patients with chromosome inversions are not susceptible to an inter-chromosomal effect. J. Assist. Reprod. Genet. 2019, 36, 509–516. [Google Scholar] [CrossRef] [PubMed]
- Liang, S.; Yang, J.; Wu, H.; Teng, X.; Duan, T. Effects of chromosome 9 inversion on IVF/ICSI: A 7-year retrospective cohort study. Mol. Genet. Genom. Med. 2019, 7, e856. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Merrion, K.; Maisenbacher, M. Pericentric inversion (Inv) 9 variant-reproductive risk factor or benign finding? J. Assist. Reprod. Genet. 2019, 36, 2557–2561. [Google Scholar] [CrossRef] [Green Version]
- Schlegel, P.N.; Sigman, M.; Collura, B.; De Jonge, C.J.; Eisenberg, M.L.; Lamb, D.J.; Mulhall, J.P.; Niederberger, C.; Sandlow, J.I.; Sokol, R.Z.; et al. Diagnosis and Treatment of Infertility in Men: AUA/ASRM Guideline PART II. J. Urol. 2021, 205, 44–51. [Google Scholar] [CrossRef]
- Esteves, S.C. A clinical appraisal of the genetic basis in unexplained male infertility. J. Hum. Reprod. Sci. 2013, 6, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Gullo, G.; Scaglione, M.; Cucinella, G.; Chiantera, V.; Perino, A.; Greco, M.E.; Laganà, A.S.; Marinelli, E.; Basile, G.; Zaami, S. Neonatal outcomes and long-term follow-up of children born from frozen embryo, a narrative review of latest research findings. Medicina 2022, 58, 1218. [Google Scholar] [CrossRef] [PubMed]
- Schaeffer, E.; Porchia, L.; Lapez-Luna, A.; Dinorah, H.-M.D.; Lopez-Bayghen, E. Aneuploidy Rates Inversely Correlate with Implantation during In Vitro Fertilization Procedures: In Favor of PGT; Chapter in Medical Genetics; IntechOpen: London, UK, 2018; pp. 1–19. [Google Scholar] [CrossRef] [Green Version]
- Serapinas, D.; Valantinavičienė, E.; Machtejevienė, E.; Bartkevičiūtė, A.; Bartkevičienė, D. Evaluation of chromosomal structural anomalies in fertility disorders. Medicina 2021, 57, 37. [Google Scholar] [CrossRef] [PubMed]
- Yan, J.; Qin, Y.; Zhao, H.; Sun, Y.; Gong, F.; Li, R.; Sun, X.; Ling, X.; Li, H.; Hao, C.; et al. Live birth with or without preimplantation genetic testing for aneuploidy. N. Engl. J. Med. 2021, 385, 2047–2058. [Google Scholar] [CrossRef]
- Shao, Y.; Li, J.; Lu, J.; Li, H.; Zhu, Y.; Jiang, W.; Yan, J. Clinical outcomes of preimplantation genetic testing (PGT) application in couples with chromosomal inversion, a study in the Chinese Han population. Reprod. Biol. Endocrinol. 2020, 18, 79. [Google Scholar] [CrossRef]
| Blastocyst Number | PGT-A Result | Karyotype | NGS Report or Conditions of Blastocysts | Related Diseases |
|---|---|---|---|---|
| 1 | Aneuploid | 45,XY,−s8,−15 | Partial deletion of chromosome 8 Monosomy of chromosome 15 | 1. Maybe related to Multiple Myeloma 2. Prader-Willi Syndrome (PWS) is 15q11—13 of deletion |
| 2 | Aneuploid | 47,XY,+13 | Trisomy of chromosome 13 | Patau’s syndrome |
| 3 | Aneuploid | 45,XY,−12 | Monosomy of chromosome 12 | Fatal |
| 4 | Aneuploid | Multiple chromosomal abnormalities | Fatal | |
| 5 | Euploid | 46,XX | Qualified for transfer | - |
| 6 | Euploid | 46,XX | Qualified for transfer | - |
| 7 | Aneuploid | 45,XX,−7 | Monosomy of chromosome 7 | Myelodysplastic Syndromes |
| 8 | No result | Whole genome amplification failure | - | |
| 9 | Aneuploid | 46,XY,−s4,+s4,−s6,+s6 | Partial deletion and duplication of chromosome 4 and 6 | Fatal |
| 10 | Aneuploid | 51,XX,+9,+13,+14,+18,+20 | Trisomy of chromosome 9, 13, 14, 18 and 20 | Fatal |
| 11 | Aneuploid | Multiple chromosomal abnormalities | Fatal | |
| 12 | Euploid | 46,XX | Developmental arrest after thawing and cultivation | - |
| 13 | Aneuploid | 47,XY,+13 | Trisomy of chromosome 13 | Patau’s syndrome |
| 14 | Aneuploid | Multiple chromosomal abnormalities | Fatal |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ting, N.-S.; Chen, Y.-H.; Chen, S.-F.; Chen, P.-C. Successful Live Twin Birth through IVF/ICSI from a Couple with an Infertile Father with Pericentric Inversion of Chromosome 9 (p12q13): A Case with a High Aneuploidy Rate. Medicina 2022, 58, 1646. https://doi.org/10.3390/medicina58111646
Ting N-S, Chen Y-H, Chen S-F, Chen P-C. Successful Live Twin Birth through IVF/ICSI from a Couple with an Infertile Father with Pericentric Inversion of Chromosome 9 (p12q13): A Case with a High Aneuploidy Rate. Medicina. 2022; 58(11):1646. https://doi.org/10.3390/medicina58111646
Chicago/Turabian StyleTing, Ning-Shiuan, Ying-Hsi Chen, Shih-Fen Chen, and Pao-Chu Chen. 2022. "Successful Live Twin Birth through IVF/ICSI from a Couple with an Infertile Father with Pericentric Inversion of Chromosome 9 (p12q13): A Case with a High Aneuploidy Rate" Medicina 58, no. 11: 1646. https://doi.org/10.3390/medicina58111646




