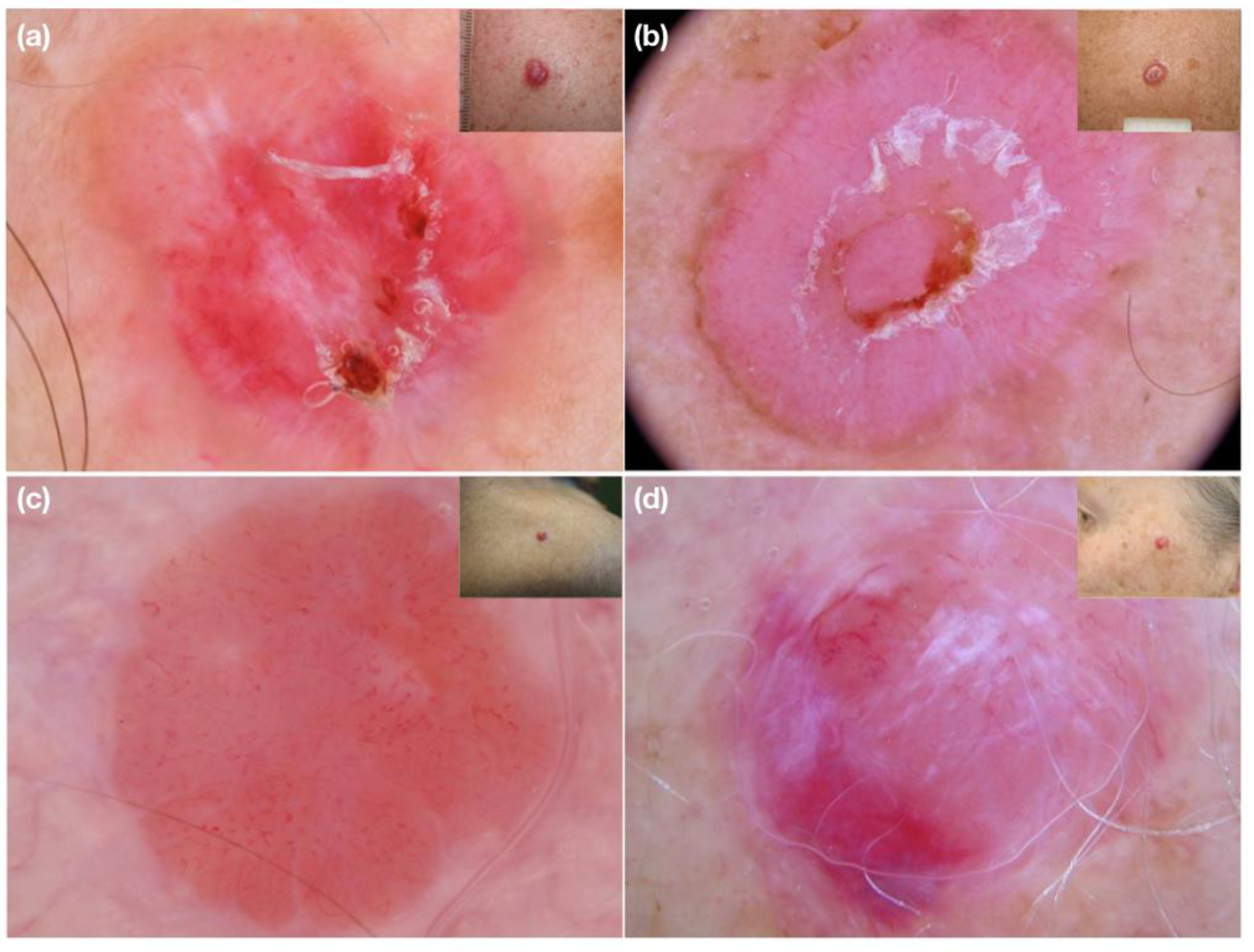
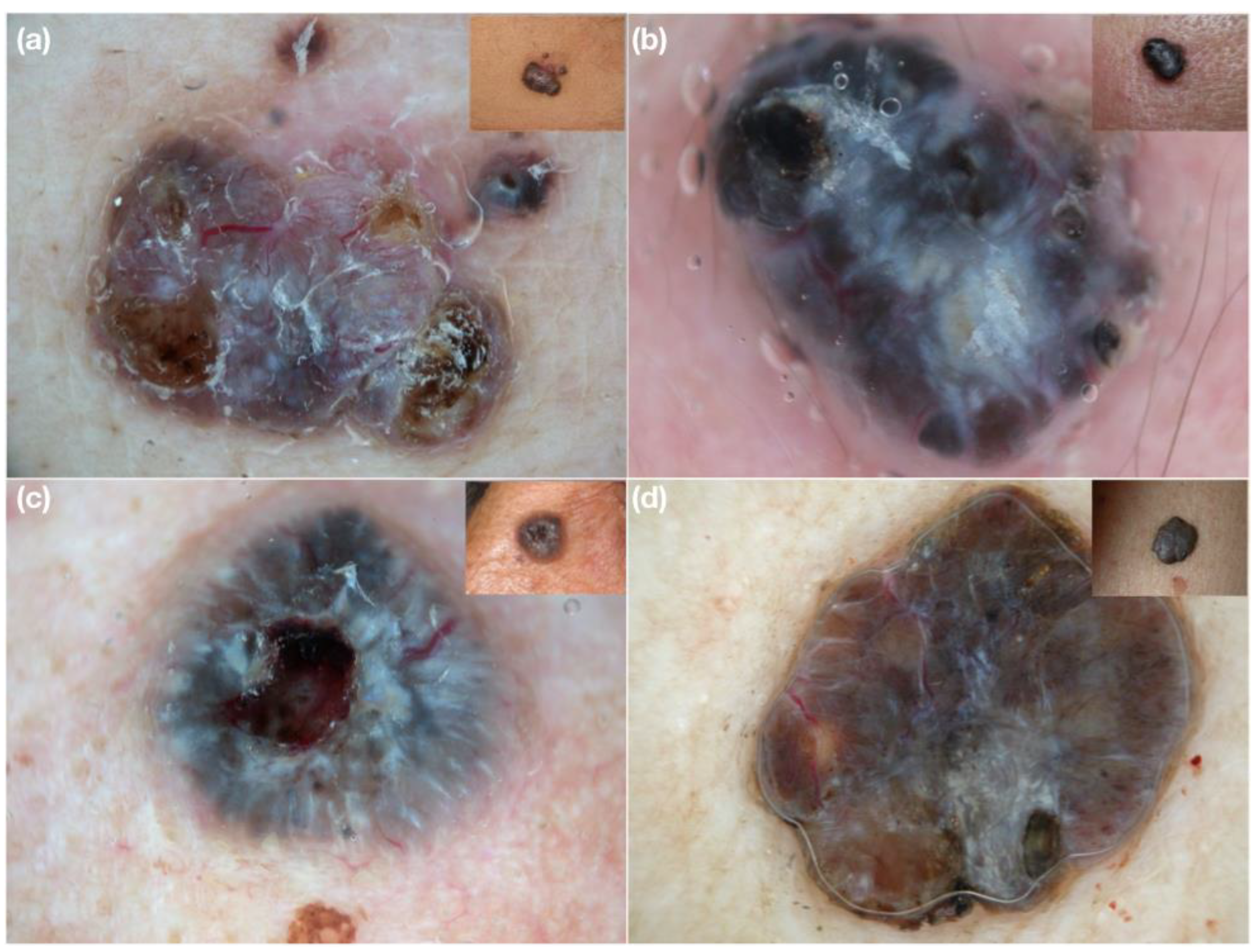
Vascular Diameter as Clue for the Diagnosis of Clinically and/or Dermoscopically Equivocal Pigmented and Non-Pigmented Basal Cell Carcinomas and Nodular Melanomas
Abstract
:1. Introduction
2. Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Conforti, C.; Giuffrida, R.; Vezzoni, R.; Resende, F.S.S.; di Meo, N.; Zalaudek, I. Dermoscopy and the experienced clinicians. Int J. Dermatol 2019. online ahead of print. [Google Scholar] [CrossRef]
- Lin, M.J.; Xie, C.; Pan, Y.; Jalilian, C.; Kelly, J.W. Dermoscopy improves diagnostic accuracy for clinically amelanotic nodules. Australas J. Dermatol. 2019, 60, 45–49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Argenziano, G.; Longo, C.; Cameron, A.; Cavicchini, S.; Gourhant, J.Y.; Lallas, A.; McColl, I.; Rosendahl, C.; Thomas, L.; Tiodorovic-Zivkovic, D.; et al. Blue-black rule: A simple dermoscopic clue to recognize pigmented nodular melanoma. Br. J. Dermatol. 2011, 165, 1251–1255. [Google Scholar] [CrossRef] [PubMed]
- Lupu, M.; Caruntu, C.; Popa, M.I.; Voiculescu, V.M.; Zurac, S.; Boda, D. Vascular patterns in basal cell carcinoma: Dermoscopic, confocal and histopathological perspectives. Oncol. Lett. 2019, 17, 4112–4125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giuffrida, R.; Conforti, C.; Di Meo, N.; Deinlein, T.; Guida, S.; Zalaudek, I. Use of noninvasive imaging in the management of skin cancer. Curr. Opin. Oncol. 2020, 32, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Farnetani, F.; Scope, A.; Coco, V.; Guida, S.; Cesinaro, A.M.; Piana, S.; Peris, K.; Pellacani, G.; Longo, C. Paradigmatic cases of pigmented lesions: How to not miss melanoma. J. Dermatol. 2016, 43, 1433–1437. [Google Scholar] [CrossRef] [PubMed]
- Pizzichetta, M.A.; Stanganelli, I.; Bono, R.; Soyer, H.P.; Magi, S.; Canzonieri, V.; Lanzanova, G.; Annessi, G.; Massone, C.; Cerroni, L.; et al. Dermoscopic features of difficult melanoma. Dermatol. Surg. 2007, 33, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Argenziano, G.; Soyer, H.P.; Chimenti, S.; Talamini, R.; Corona, R.; Sera, F.; Binder, M.; Cerroni, L.; De Rosa, G.; Ferrara, G.; et al. Dermoscopy of pigmented skin lesions: Results of a consensus meeting via the Internet. J. Am. Acad. Dermatol. 2003, 48, 679–693. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marghoob, A.A.; Braun, R. Proposal for a revised 2-step algorithm for the classification of lesions of the skin using dermoscopy. Arch. Dermatol. 2010, 146, 426–428. [Google Scholar] [CrossRef] [PubMed]
- Zalaudek, I.; Kreusch, J.; Giacomel, J.; Ferrara, G.; Catricalà, C.; Argenziano, G. How to diagnose nonpigmented skin tumors: A review of vascular structures seen with dermoscopy: Part I. Melanocytic skin tumors. J. Am. Acad. Dermatol. 2010, 63, 361–374. [Google Scholar] [CrossRef] [PubMed]
- Togawa, Y. Review of vasculature visualized on dermoscopy. J. Dermatol. 2017, 44, 525–532. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ayhan, E.; Ucmak, D.; Akkurt, Z. Vascular structures in dermoscopy. An. Bras. Dermatol. 2015, 90, 545–553. [Google Scholar] [CrossRef] [PubMed]
- Weber, P.; Tschandl, P.; Sinz, C.; Kittler, H. Dermatoscopy of Neoplastic Skin Lesions: Recent Advances, Updates, and Revisions. Curr. Treat. Options Oncol. 2018, 19, 56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lallas, A.; Apalla, Z.; Argenziano, G.; Longo, C.; Moscarella, E.; Specchio, F.; Raucci, M.; Zalaudek, I. The dermatoscopic universe of basal cell carcinoma. Dermatol. Pract. Concept. 2014, 4, 11–24. [Google Scholar] [CrossRef] [PubMed]



| Number of Correct Diagnoses | % Improvement vs. Clinical Diagnosis | |
|---|---|---|
| Clinical | 65/128 (50.8%) | |
| Dermoscopic | 105/128 (82.0%) | 61.5% |
| Focusing on the diameter of vessels | 110/128 (85.9%) | 69.2% |
| Dermoscopic Evaluations | Nodular Melanoma | Nodular BCC | |||
|---|---|---|---|---|---|
| n = 71/128 (55.5%) | Non-Pigmented | Pigmented | Non-Pigmented | Pigmented | |
| Arborizing vessels, n (%) | 35 (27.3%) | 1 (0.8%) | - | 25 (19.5%) | 9 (7.0%) |
| Comma vessels, n (%) | 1 (0.8%) | - | - | 1 (0.8%) | - |
| Linear irregular vessels, n (%) | 7 (5.46%) | 4 (3.1%) | - | 2 (1.5%) | 1 (0.8%) |
| Dotted vessels, n (%) | 1 (0.8%) | 1 (0.8%) | - | - | - |
| Curved vessels, n (%) | 1 (0.8%) | 1 (0.8%) | - | - | - |
| Hairpin-like vessels, n (%) | 1 (0.8%) | 1 (0.8%) | - | - | - |
| Corkcrew vessels, n (%) | 1 (0.8%) | 1 (0.8%) | - | - | - |
| Polymorphous vessels, n (%) | 17 (13.2%) | 14 (10.9%) | 3 (2.3%) | - | |
| Small vessels, n (%) | 3 (2.3%) | 3 (2.3%) | - | - | - |
| Large prominent vessels, n (%) | 4 (3.1%) | - | - | - | 4 (3.1%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giuffrida, R.; Conforti, C.; Blum, A.; Buljan, M.; Guarneri, F.; Hofmann-Wellenhof, R.; Longo, C.; Paoli, J.; Rosendahl, C.; Soyer, H.P.; et al. Vascular Diameter as Clue for the Diagnosis of Clinically and/or Dermoscopically Equivocal Pigmented and Non-Pigmented Basal Cell Carcinomas and Nodular Melanomas. Medicina 2022, 58, 1761. https://doi.org/10.3390/medicina58121761
Giuffrida R, Conforti C, Blum A, Buljan M, Guarneri F, Hofmann-Wellenhof R, Longo C, Paoli J, Rosendahl C, Soyer HP, et al. Vascular Diameter as Clue for the Diagnosis of Clinically and/or Dermoscopically Equivocal Pigmented and Non-Pigmented Basal Cell Carcinomas and Nodular Melanomas. Medicina. 2022; 58(12):1761. https://doi.org/10.3390/medicina58121761
Chicago/Turabian StyleGiuffrida, Roberta, Claudio Conforti, Andreas Blum, Marija Buljan, Fabrizio Guarneri, Rainer Hofmann-Wellenhof, Caterina Longo, John Paoli, Cliff Rosendahl, H. Peter Soyer, and et al. 2022. "Vascular Diameter as Clue for the Diagnosis of Clinically and/or Dermoscopically Equivocal Pigmented and Non-Pigmented Basal Cell Carcinomas and Nodular Melanomas" Medicina 58, no. 12: 1761. https://doi.org/10.3390/medicina58121761









