A Novel Technique for Shortening Orthodontic Treatment: The “JET System”
Abstract
:1. Introduction
2. Concepts of JET System
2.1. Zero-Step Method
2.2. Simultaneous Tooth Extraction
2.3. Passive Self-Ligating Brackets (PSL)
2.4. Bi-Dimensional Slots
2.5. Rapid Wire Sequence
2.6. Initial Elastic (Intermaxillary Elastic)
2.7. Indirect Bonding
2.8. Oral Myofunctional Therapy (MFT)
3. Case Presentation
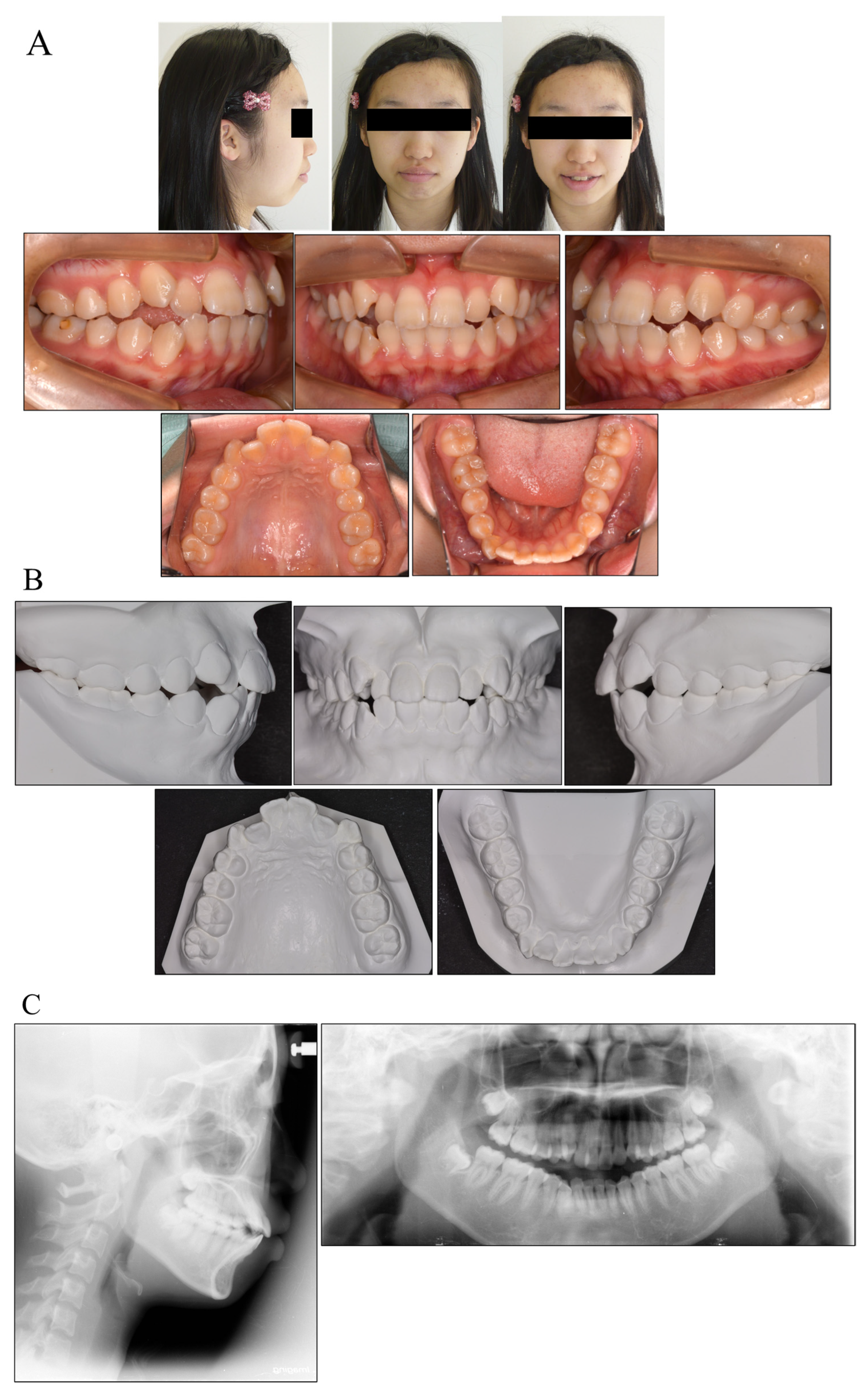
3.1. Diagnosis and Etiology
3.2. Treatment and Objectives
3.3. Treatment Alternatives
3.4. Treatment Progress
3.5. Treatment Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| JET system | Jiyugaoka Enjoyable Treatment system; |
| Ni-Ti | nickel-titanium; |
| SLBs | self-ligating brackets; |
| MFT | myofunctional therapy; |
| RAP | regional acceleratory phenomenon; |
| OTM | orthodontic tooth movement. |
References
- Yamazaki, T.; Tamura, Y.; Nakakuki, M.; Namura, S. An advantage of using the SPEED appliance—Shortening active treatment time. Orthod. Waves 1998, 57, 327–339. [Google Scholar]
- Beckwith, F.R.; Ackerman, R.J., Jr.; Cobb, C.M.; Tira, D.E. An evaluation of factors affecting duration of orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 1999, 115, 439–447. [Google Scholar] [CrossRef]
- Jung, M.H. Factors influencing treatment efficiency: A prospective cohort study. Angle. Orthod. 2020, 91, 1–8. [Google Scholar] [CrossRef]
- Fink, D.F.; Smith, R.J. The duration of orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 1992, 102, 45–51. [Google Scholar] [CrossRef]
- Maveas, D.; Athanasiou, A.E. Factors affecting the duration of orthodontic treatment: A systematic review. Eur. J. Orthod. 2008, 30, 386–395. [Google Scholar] [CrossRef] [Green Version]
- Vig, P.S.; Weintraub, J.A.; Brown, C.; Kowalski, C.J. The duration of orthodontic treatment with and without extractions: A pilot study of five selected practices. Am. J. Orthod. Dentofac. Orthop. 1990, 7, 45–51. [Google Scholar] [CrossRef]
- Alger, D.W. Appointment frequency versus treatment time. Am. J. Orthod. Dentofac. Orthop. 1988, 94, 436–439. [Google Scholar] [CrossRef]
- Shelton, C.E.; Cisneros, G.J.; Nelson, S.E.; Watkins, P. Decreased treatment time due to changes in technique and practice philosophy. Am. J. Orthod. Dentofac. Orthop. 1994, 106, 654–657. [Google Scholar] [CrossRef]
- Aragon, M.L.C.; Bichara, L.M.; Flores-Mir, C.; Almeida, G.; Normando, D. Efficiency of compensatory orthodontic treatment of mild Class III malocclusion with two different bracket systems. Dent. Press. J. Orthod. 2017, 22, 49–55. [Google Scholar] [CrossRef] [Green Version]
- Bizzarro, M.; Generali, C.; Maietta, S.; Martorelli, M.; Ferrillo, M.; Flores-Mir, C.; Perillo, L. Association between 3D palatal morphology and upper arch dimensions in buccally displaced maxillary canines early in mixed dentition. Eur. J. Orthod. 2018, 40, 592–596. [Google Scholar] [CrossRef] [PubMed]
- Redllich, M.; Mayer, Y.; Harari, D.; Lewinstein, I. In vitro study of frictional forces during sliding mechanics of “reduced-friction” brackets. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 69–73. [Google Scholar] [CrossRef]
- Burrow, S.J. Friction and resistance to sliding in orthodontics: A critical review. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 442–447. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, M.; Kalathil, S.; Abraham, K.M. Comparative evaluation of frictional forces in active and passive self-ligating brackets with various archwire alloys. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 675–682. [Google Scholar] [CrossRef] [PubMed]
- Ehsani, S.; Mandich, M.A.; El-Bialy, T.H.; Flores-Mir, C. Frictional resistance in self-ligating orthodontic brackets and conventionally ligated brackets. A systematic review. Angle Orthod. 2009, 79, 592–601. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miura, F.; Mogi, M.; Ohura, Y.; Hamanaka, H. The super-elastic property of the Japanese NiTi alloy wire for use in orthodontics. Am. J. Orthod. Dentofac. Orthop. 1986, 90, 1–10. [Google Scholar] [CrossRef]
- Miura, F.; Mogi, M.; Ohura, Y.; Karibe, M. The super-elastic Japanese NiTi alloy wire for use in orthodontics. Part III. Studies on the Japanese NiTi alloy coil springs. Am. J. Orthod. Dentofac. Orthop. 1988, 94, 89–96. [Google Scholar] [CrossRef]
- Yee, J.A.; Türk, T.; Elekdağ-Türk, S.; LCheng, L.; Darendeliler, M.A. Rate of tooth movement under heavy and light continuous orthodontic forces. Am. J. Orthod. Dentofac. Orthop. 2009, 136, e1–e9. [Google Scholar] [CrossRef]
- Tomizuka, R.; Kanetaka, H.; Shimizu, Y.; Suzuki, A.; Igarashi, K.; Mitani, H. Effects of gradually increasing force generated by permanent rare earth magnets for orthodontic tooth movement. Angle Orthod. 2006, 76, 1004–1009. [Google Scholar] [CrossRef] [PubMed]
- Damon. D.H. The rationale, evolution and clinical application of the self-ligating bracket. Clin. Orthod. Res. 1998, 52, 52–61. [Google Scholar]
- Fleming, P.S.; Johal, A. Self-ligating brackets in orthodontics. A systematic review. Angle Orthod. 2010, 80, 575–584. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, S.S.H.; Greenlee, M.G.; Kim, J.E.; Smith, C.L.; Huang, G.J. Systematic review of self-ligating brackets. Am. J. Orthod. Dentofac. Orthop. 2010, 137, e1–e18. [Google Scholar] [CrossRef]
- Di Biase, A.T.; Nasr, I.H.; Scott, P.; Cobourne, M.T. Duration of treatment and occlusal outcome using Damon3 self-ligated and conventional orthodontic bracket systems in extraction patients: A prospective randomized clinical trial. Am. J. Orthod. Dentofac. Orthop. 2011, 139, e111–e116. [Google Scholar] [CrossRef] [PubMed]
- Ong, E.; McCallum, H.; Griffin, M.P.; Ho, C. Efficiency of self-ligating vs. conventionally ligated brackets during initial alignment. Am. J. Orthod. Dentofac. Orthop. 2010, 138, e1–e7. [Google Scholar] [CrossRef]
- Andreasen, G.F.; Zwanziger, D. A clinical evaluation of the differential force concept as applied to the edgewise bracket. Am. J. Orthod. 1980, 78, 25–40. [Google Scholar] [CrossRef]
- Begg, P.R.; Kesling, P.C. Begg Orthodontic Theory and Technique; W.B. Saunders: Philadelphia, PA, USA, 1977. [Google Scholar]
- Frost, H.M. The biology of fracture healing. An overview for clinicians. Part II. Clin. Orthop. Relat. Res. 1989, 248, 294–309. [Google Scholar]
- Bogoch, E.; Gschwend, N.; Rahn, B.; Moran, E.; Perren, S. Healing of cancellous bone osteotomy in rabbits—Part I: Regulation of bone volume and the regional acceleratory phenomenon in normal bone. J. Orthop. Res. 1993, 11, 285–291. [Google Scholar] [CrossRef]
- Bogoch, E.; Gschwend, N.; Rahn, B.; Moran, E.; Perren, S. Healing of cancellous bone osteotomy in rabbits—Part II: Local reversal of arthritis-induced osteopenia after osteotomy. J. Orthop. Res. 1993, 11, 292–298. [Google Scholar] [CrossRef]
- Miles, P.G. Self-ligating vs. conventional twin brackets during en-masse space closure with sliding mechanics. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 223–225. [Google Scholar] [CrossRef] [PubMed]
- Mezomo, M.; Lima, E.S.; Menezes, L.M.; Weissheimer, A.; Allgayer, S. Maxillary canine retraction with self-ligating and conventional brackets. Angle Orthod. 2011, 81, 292–297. [Google Scholar] [CrossRef] [Green Version]
- Mathews, D.P.; Kokich, V.G. Accelerating tooth movement: The case against corticotomy-induced orthodontics. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 5–13. [Google Scholar] [CrossRef]
- Proffit, W.R.; Fields, H.W.; Sarver, D.M. Comtemporary Orthodontics, 6th ed.; Elsevier Science: Amsterdam, The Netherlands, 2009; p. 295. [Google Scholar]
- Joiner, M. In-house precision bracket placement with the indirect bonding technique. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 850–854. [Google Scholar] [CrossRef] [PubMed]
- Darendeliler, M.A.; Darendeliler, H.; Uner, O. The drum spring (DS) retractor: Constant and continuous force for canine retraction. Eur. J. Orthod. 1997, 19, 115–130. [Google Scholar] [CrossRef] [Green Version]
- Monini, A.d.C.; Gandini, L.G., Jr.; Vianna, A.P.; Martins, R.P.; Jacob, H.B. Tooth movement rate and anchorage lost during canine retraction: A maxillary and mandibular comparison. Angle Orthod. 2019, 89, 559–565. [Google Scholar] [CrossRef] [Green Version]
- Verna, C. Regional Acceleratory Phenomenon. Front. Oral. Biol. 2016, 18, 28–35. [Google Scholar] [PubMed]





| Variable | Japanese Norm (±S.D.) | Pretreatment (15y 11m) | Posttreatment (17y 1m) | 3 Years 6 Months after Debonding (20y 7m) |
|---|---|---|---|---|
| SNA (°) | 81.3 ± 3.5 | 81.6 | 81.6 | 81.6 |
| SNB (°) | 78.9 ± 3.5 | 76.9 | 76.9 | 76.9 |
| ANB (°) | 3.4 ± 1.8 | 4.7 | 4.7 | 4.7 |
| FMA (°) | 28.8 ± 4.1 | 32.6 | 32.6 | 32.6 |
| FMIA (°) | 56.9 ± 6.4 | 44.2 | 57.2 | 56.9 |
| IMPA (°) | 96.3 ± 5.8 | 103.2 | 90.2 | 90.5 |
| FH-U1 (°) | 111.1 ± 5.5 | 113.5 | 101.1 | 101.8 |
| U1-L1 (°) | 124.1 ± 7.6 | 110.7 | 136.1 | 135.1 |
| Gonial angle (°) | 122.2 ± 4.6 | 124.2 | 124.2 | 124.2 |
| E-line:Upper (mm) | +2.0 ± 2.0 | +2.9 | +0.3 | −0.8 |
| E-line:Lower (mm) | +2.0 ± 2.0 | +6.3 | +3.1 | −0.1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Narita, S.; Narita, K.; Yamaguchi, M. A Novel Technique for Shortening Orthodontic Treatment: The “JET System”. Medicina 2022, 58, 150. https://doi.org/10.3390/medicina58020150
Narita S, Narita K, Yamaguchi M. A Novel Technique for Shortening Orthodontic Treatment: The “JET System”. Medicina. 2022; 58(2):150. https://doi.org/10.3390/medicina58020150
Chicago/Turabian StyleNarita, Shinichi, Kiyoko Narita, and Masaru Yamaguchi. 2022. "A Novel Technique for Shortening Orthodontic Treatment: The “JET System”" Medicina 58, no. 2: 150. https://doi.org/10.3390/medicina58020150
APA StyleNarita, S., Narita, K., & Yamaguchi, M. (2022). A Novel Technique for Shortening Orthodontic Treatment: The “JET System”. Medicina, 58(2), 150. https://doi.org/10.3390/medicina58020150






