Comparing Perioperative Outcome Measures of the Dynamic Hip Screw and the Femoral Neck System
Abstract
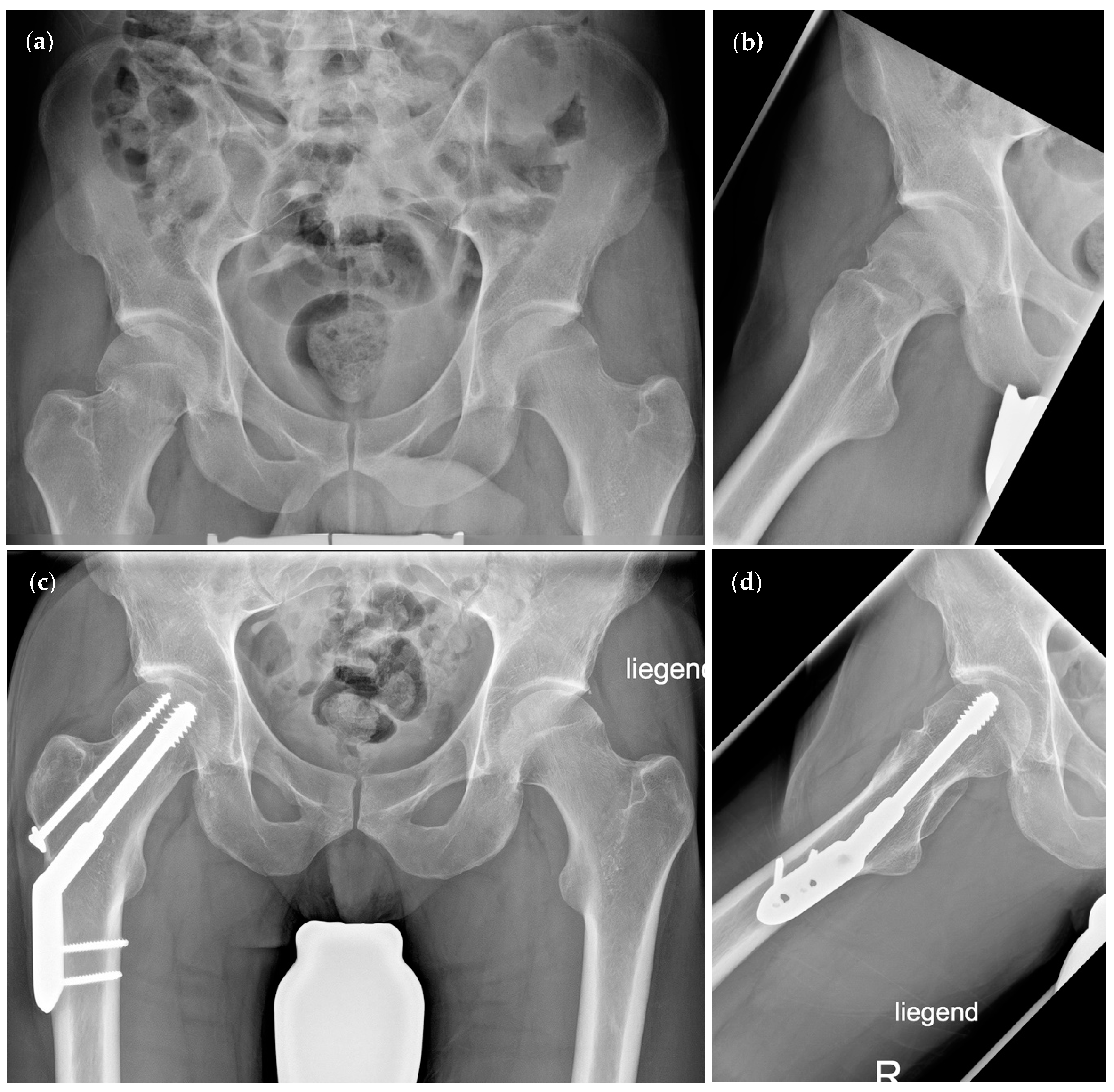
:1. Introduction
2. Methods
3. Results
3.1. Demographics
3.2. Outcome Measures
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gullberg, B.; Johnell, O.; Kanis, J.A. World-wide projections for hip fracture. Osteoporos Int. 1997, 7, 407–413. Available online: https://pubmed.ncbi.nlm.nih.gov/9425497/ (accessed on 4 January 2022). [CrossRef] [PubMed]
- Dyer, S.M.; Crotty, M.; Fairhall, N.; Magaziner, J.; Beaupre, L.A.; Cameron, I.D.; Sherrington, C. A critical review of the long-term disability outcomes following hip fracture. BMC Geriatr. 2016, 16, 158. Available online: https://pubmed.ncbi.nlm.nih.gov/27590604/ (accessed on 4 January 2022). [CrossRef] [PubMed] [Green Version]
- Klestil, T.; Röder, C.; Stotter, C.; Winkler, B.; Nehrer, S.; Lutz, M.; Klerings, I.; Wagner, G.; Gartlehner, G.; Nussbaumer-Streit, B. Impact of timing of surgery in elderly hip fracture patients: A systematic review and meta-analysis. Sci. Rep. 2018, 8, 13933. Available online: https://pubmed.ncbi.nlm.nih.gov/30224765/ (accessed on 4 January 2022). [CrossRef] [PubMed] [Green Version]
- Fischer, H.; Maleitzke, T.; Eder, C.; Ahmad, S.; Stöckle, U.; Braun, K.F. Management of proximal femur fractures in the elderly: Current concepts and treatment options. Eur. J. Med Res. 2021, 26, 86. Available online: https://pubmed.ncbi.nlm.nih.gov/34348796/ (accessed on 4 January 2022). [CrossRef] [PubMed]
- Bhandari, M.; Swiontkowski, M. Management of Acute Hip Fracture. N. Engl. J. Med. 2017, 377, 2053–2062. Available online: https://pubmed.ncbi.nlm.nih.gov/29166235/ (accessed on 4 January 2022). [CrossRef]
- Pauwels, F. Der Schenkelhalsbruch. In Gesammelte Abhandlungen zur funktionellen Anat des Bewegungsapparates; Springer: Berlin/Heidelberg, Germany, 1965; pp. 1–138. Available online: https://link.springer.com/chapter/10.1007/978-3-642-86841-2_1 (accessed on 2 February 2022).
- Garden, R.S. Low-Angle Fixation in Fractures of the Femoral Neck. J. Bone Jt. Surgery. Br. Vol. 1961, 43-B, 647–663. Available online: https://online.boneandjoint.org.uk/doi/abs/10.1302/0301-620X.43B4.647 (accessed on 2 February 2022). [CrossRef]
- Freitas, A.; Júnior, J.V.T.; dos Santos, A.F.; Aquino, R.J.; Leão, V.N.; de Alcântara, W.P. Biomechanical study of different internal fixations in Pauwels type III femoral neck fracture—A finite elements analysis. J. Clin. Orthop. Trauma 2021, 14, 145–150. [Google Scholar] [CrossRef]
- Li, L.; Zhao, X.; Yang, X.; Tang, X.; Liu, M. Dynamic hip screws versus cannulated screws for femoral neck fractures: A systematic review and meta-analysis. J. Orthop. Surg. Res. 2020, 15, 352. Available online: https://pubmed.ncbi.nlm.nih.gov/32843048/ (accessed on 4 January 2022). [CrossRef]
- DePuy Synthes. Femoral Neck System (FNS). 2019. Available online: https://www.jnjmedicaldevices.com/sites/default/files/user_uploaded_assets/pdf_assets/2019-09/FNS Value Brief.pdf (accessed on 4 January 2022).
- DePuy Synthes. Femoral Neck System Operationstechnik. 2018. Available online: http://synthes.vo.llnwd.net/o16/LLNWMB8/INT Mobile/Synthes International/Product Support Material/legacy_Synthes_PDF/DSEM-TRM-0614-0098-3a_LR.pdf (accessed on 4 January 2022).
- Cha, Y.; Song, J.-U.; Yoo, J.-I.; Park, K.H.; Kim, J.-T.; Park, C.H.; Choy, W.-S. Improved control over implant anchorage under the use of the femoral neck system for fixation of femoral neck fractures: A technical note. BMC Musculoskelet. Disord. 2021, 22, 621. Available online: https://pubmed.ncbi.nlm.nih.gov/34256741/ (accessed on 4 January 2022). [CrossRef]
- Stoffel, K.; Zderic, I.; Gras, F.; Sommer, C.; Eberli, U.; Mueller, D.; Oswald, M.; Gueorguiev, B. Biomechanical Evaluation of the Femoral Neck System in Unstable Pauwels III Femoral Neck Fractures: A Comparison with the Dynamic Hip Screw and Cannulated Screws. J. Orthop. Trauma 2017, 31, 131–137. Available online: https://pubmed.ncbi.nlm.nih.gov/27755333/ (accessed on 4 January 2022). [CrossRef] [PubMed]
- He, C.; Lu, Y.; Wang, Q.; Ren, C.; Li, M.; Yang, M.; Xu, Y.; Li, Z.; Zhang, K.; Ma, T. Comparison of the clinical efficacy of a femoral neck system versus cannulated screws in the treatment of femoral neck fracture in young adults. BMC Musculoskelet. Disord. 2021, 22, 994. Available online: https://pubmed.ncbi.nlm.nih.gov/34844578/ (accessed on 4 January 2022). [CrossRef] [PubMed]
- Hu, H.; Cheng, J.; Feng, M.; Gao, Z.; Wu, J.; Lu, S. Clinical outcome of femoral neck system versus cannulated compression screws for fixation of femoral neck fracture in younger patients. J. Orthop. Surg. Res. 2021, 16, 370. Available online: https://pubmed.ncbi.nlm.nih.gov/34107990/ (accessed on 4 January 2022). [CrossRef] [PubMed]
- Tang, Y.; Zhang, Z.; Wang, L.; Xiong, W.; Fang, Q.; Wang, G. Femoral neck system versus inverted cannulated cancellous screw for the treatment of femoral neck fractures in adults: A preliminary comparative study. J. Orthop. Surg. Res. 2021, 16, 504. Available online: https://pubmed.ncbi.nlm.nih.gov/34399801/ (accessed on 4 January 2022). [CrossRef]
- Vazquez, O.; Gamulin, A.; Hannouche, D.; Belaieff, W. Osteosynthesis of non-displaced femoral neck fractures in the elderly population using the femoral neck system (FNS): Short-term clinical and radiological outcomes. J. Orthop. Surg. Res. 2021, 16, 477. Available online: https://pubmed.ncbi.nlm.nih.gov/34348753/ (accessed on 4 January 2022). [CrossRef] [PubMed]
- Zhou, X.-Q.; Li, Z.-Q.; Xu, R.-J.; She, Y.-S.; Zhang, X.-X.; Chen, G.-X.; Yu, X. Comparison of Early Clinical Results for Femoral Neck System and Cannulated Screws in the Treatment of Unstable Femoral Neck Fractures. Orthop Surg. 2021, 13, 1802–1809. Available online: https://pubmed.ncbi.nlm.nih.gov/34351048/ (accessed on 4 January 2022). [CrossRef] [PubMed]
- Charlson, M.; Szatrowski, T.P.; Peterson, J.; Gold, J. Validation of a combined comorbidity index. J. Clin. Epidemiol. 1994, 47, 1245–1251. Available online: https://pubmed.ncbi.nlm.nih.gov/7722560/ (accessed on 4 January 2022). [CrossRef]
- Motulsky, H.J.; Brown, R.E. Detecting outliers when fitting data with nonlinear regression—A new method based on robust nonlinear regression and the false discovery rate. BMC Bioinform. 2006, 7, 123. Available online: https://bmcbioinformatics.biomedcentral.com/articles/10.1186/1471-2105-7-123 (accessed on 3 February 2022). [CrossRef] [PubMed] [Green Version]
- Chaplin, V.; Matharu, G.; Knebel, R. Complications following hemiarthroplasty for displaced intracapsular femoral neck fractures in the absence of routine follow-up. Ann. R. Coll. Surg. Engl. 2013, 95, 271–274. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cintean, R.; Pankratz, C.; Hofmann, M.; Gebhard, F.; Schütze, K. Early Results in Non-Displaced Femoral Neck Fractures Using the Femoral Neck System. Geriatr. Orthop. Surg. Rehabil. 2021, 12. Available online: https://pubmed.ncbi.nlm.nih.gov/34733579/ (accessed on 4 January 2022). [CrossRef] [PubMed]
- HrubIna, M.; SkOták, M.; BěHOunek, J. Osteosyntéza zlomenin proximálního femuru metodou DHS: Infekční komplikace DHS Osteosynthesis for Proximal Femoral Fractures: Infectious Complications. ACHOT 2013, 80, 351–355. [Google Scholar]
- Stassen, R.C.; Jeuken, R.M.; Boonen, B.; Meesters, B.; de Loos, E.R.; van Vugt, R. First clinical results of 1-year follow-up of the femoral neck system for internal fixation of femoral neck fractures. Arch. Orthop. Trauma. Surg. 2021. Available online: https://pubmed.ncbi.nlm.nih.gov/34734328/ (accessed on 4 January 2022). [CrossRef]
- Schopper, C.; Zderic, I.; Menze, J.; Müller, D.; Rocci, M.; Knobe, M.; Shoda, E.; Richards, G.; Gueorguiev, B.; Stoffel, K. Higher stability and more predictive fixation with the Femoral Neck System versus Hansson Pins in femoral neck fractures Pauwels II. J. Orthop. Transl. 2020, 24, 88–95. Available online: https://pubmed.ncbi.nlm.nih.gov/32775200/ (accessed on 4 January 2022). [CrossRef]
- Cheng, H.; Clymer, J.W.; Chen, B.P.-H.; Sadeghirad, B.; Ferko, N.C.; Cameron, C.G.; Hinoul, P. Prolonged operative duration is associated with complications: A systematic review and meta-analysis. J. Surg. Res. 2018, 229, 134–144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nanty, L.; Canovas, F.; Rodriguez, T.; Faure, P.; Dagneaux, L. Femoral neck shortening after internal fixation of Garden I fractures increases the risk of femoral head collapse. Orthop. Traumatol. Surg. Res. 2019, 105, 999–1004. [Google Scholar] [CrossRef] [PubMed]
- Linde, F.; Andersen, E.; Hvass, I.; Madsen, F.; Pallesen, R. Avascular femoral head necrosis following fracture fixation. Injury 1986, 17, 159–163. [Google Scholar] [CrossRef]
- Melisik, M.; Hrubina, M.; Daniel, M.; Cibula, Z.; Rovnak, M.; Necas, L. Ultra-short cementless anatomical stem for intracapsular femoral neck fractures in patients younger than 60 years. Acta Orthop. Belg. 2021, 87, 619–627. [Google Scholar] [CrossRef] [PubMed]



| DHS (n = 19) | FNS (n = 12) | Statistics | ||
|---|---|---|---|---|
| Age (years) | 60.47 ± 17 | 66.5 ± 10.98 | p = 0.34 | |
| (95% CI 52.28–68.67) | (95% CI 59.52–73.48) | |||
| Gender | Female (% of group) | 10 (52.63%) | 6 (50%) | p = 1 |
| Male (% of group) | 9 (47.37%) | 6 (50%) | ||
| ASA | 2.32 ± 0.75 | 2.42 ± 0.67 | p = 0.81 | |
| (95% CI 1.96–2.68) | (95% CI 1.99–2.84) | |||
| CCI | 3.16 ± 3.39 | 4.42 ± 3.7 | p = 0.38 | |
| (95% CI 1.53–4.79) | (95% CI 2.06–6.77) | |||
| Preoperative Pauwels angle (°) | 50.93 ± 14.07 | 47.66 ± 14.44 | p = 0.41 | |
| (95% CI 44.15–57.71) | (95% CI 38.49–56.83) | |||
| Postoperative Pauwels angle (°) | 46.74 ± 7.71 | 43.34 ± 7.93 | p = 0.22 | |
| (95% CI 43.03–50.46) | (95% CI 38.3–48.38) | |||
| Preoperative CCD angle (°) | 129.5 ± 16.21 | 130.8 ± 13.25 | p = 0.8 | |
| (95% CI 121.7–137.3) | (95% CI 122.4–139.2) | |||
| Postoperative CCD angle (°) | 135.9 ± 7.27 | 136 ± 5.24 | p = 0.85 | |
| (95% CI 132.4–139.4) | (95% CI 132.7–139.4) | |||
| Pauwels classification | Type I (% of group) | 1 (5.26%) | 1 (8.33%) | p = 0.72 * |
| Type II (% of group) | 10 (52.63%) | 7 (58.33%) | ||
| Type III (% of group) | 8 (42.11%) | 4 (33.33%) | ||
| Garden classification | Type I (% of group) | 2 (10.53%) | 1 (8.33%) | p = 0.45 ** |
| Type II (% of group) | 9 (47.37%) | 8 (66.67%) | ||
| Type III (% of group) | 4 (21.05%) | 2 (16.67%) | ||
| Type IV (% of group) | 4 (21.05%) | 1 (8.33%) | ||
| TTS (min) | 44.74 ± 10.66 | 48.83 ± 34.15 | p = 0.16 | |
| (95% CI 39.6–49.87) | (95% CI 27.13–70.53) | |||
| In situ fixation | Yes (% of group) | 2 (10.53%) | 2 (16.67%) | p = 0.63 |
| No (% of group) | 17 (89.47%) | 10 (83.33%) | ||
| Perioperative volume therapy (L) | 1616 ± 661.2 | 1291 ± 784.2 | p = 0.46 | |
| (95% CI 1297–1934) | (95% CI 793.1–1790) | |||
| Postoperative weight bearing | Partial weight bearing (% of group) | 18 (94.74%) | 10 (83.33%) | p = 0.54 |
| Full weight bearing (% of group) | 1 (5.26%) | 2 (16.67%) | ||
| Discharge status | Stationary rehabilitation (% of group) | 5 (26.32%) | 7 (58.33%) | p = 0.13 |
| Home (% of group) | 14 (73.68%) | 5 (41.67%) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Niemann, M.; Braun, K.F.; Ahmad, S.S.; Stöckle, U.; Märdian, S.; Graef, F. Comparing Perioperative Outcome Measures of the Dynamic Hip Screw and the Femoral Neck System. Medicina 2022, 58, 352. https://doi.org/10.3390/medicina58030352
Niemann M, Braun KF, Ahmad SS, Stöckle U, Märdian S, Graef F. Comparing Perioperative Outcome Measures of the Dynamic Hip Screw and the Femoral Neck System. Medicina. 2022; 58(3):352. https://doi.org/10.3390/medicina58030352
Chicago/Turabian StyleNiemann, Marcel, Karl F. Braun, Sufian S. Ahmad, Ulrich Stöckle, Sven Märdian, and Frank Graef. 2022. "Comparing Perioperative Outcome Measures of the Dynamic Hip Screw and the Femoral Neck System" Medicina 58, no. 3: 352. https://doi.org/10.3390/medicina58030352
APA StyleNiemann, M., Braun, K. F., Ahmad, S. S., Stöckle, U., Märdian, S., & Graef, F. (2022). Comparing Perioperative Outcome Measures of the Dynamic Hip Screw and the Femoral Neck System. Medicina, 58(3), 352. https://doi.org/10.3390/medicina58030352








