Malunion of the Tibia: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Patient Evaluation
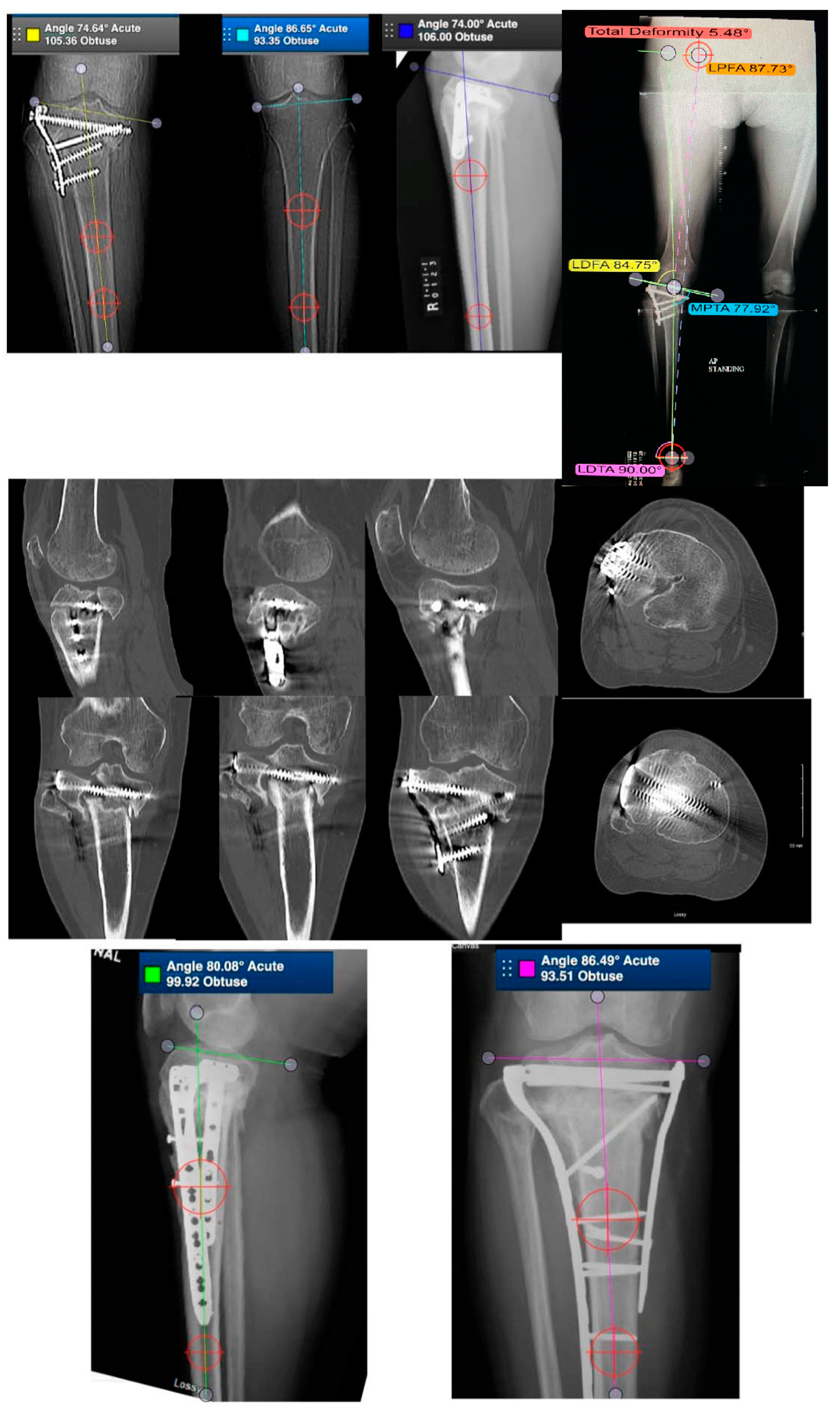
3.2. Tibial Plateau Malunion
3.2.1. Demographics and Complications
3.2.2. Lateral Plateau
3.2.3. Medial Plateau
3.2.4. Posteromedial Plateau
3.2.5. Bicondylar Plateau
3.2.6. Plateau Widening
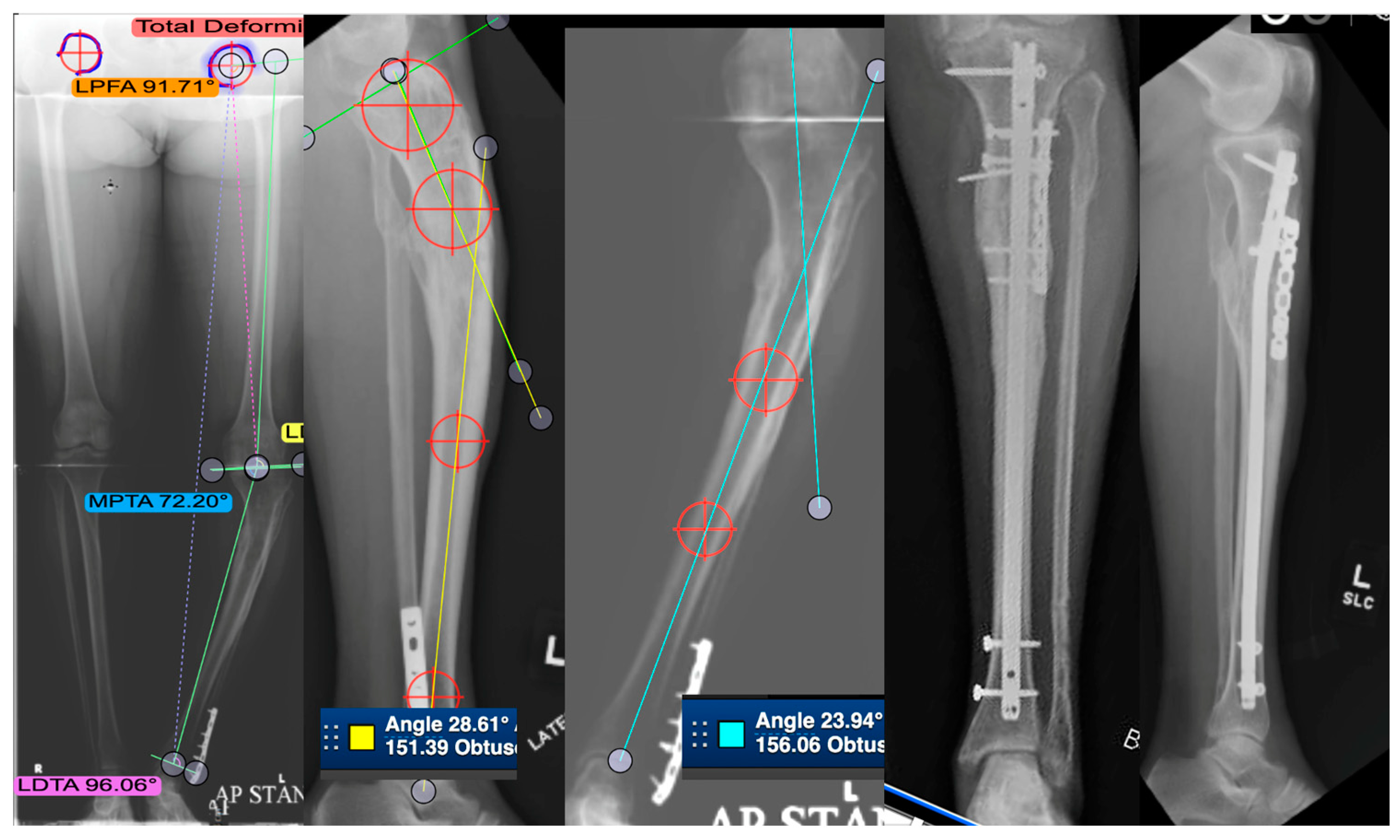
3.3. Tibial Shaft Malunion
Demographics and Complications
3.4. Distal Tibial Malunion
3.4.1. Demographics and Complications
3.4.2. Patients, Surgical Fixation, and Outcomes
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Sarmiento, A.; Sobol, P.A.; Hoy, A.L.S.; Ross, S.D.; Racette, W.L.; Tarr, R.R. Prefabricated functional braces for the treatment of fractures of the tibial diaphysis. J. Bone Jt. Surg Am. 1984, 66, 1328–1339. [Google Scholar] [CrossRef]
- Santoro, D.; Tantavisut, S.; Aloj, D.; Karam, M.D. Diaphyseal osteotomy after post-traumatic malalignment. Curr. Rev. Musculoskelet. Med. 2014, 7, 312–322. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Anglen, J.O.; Healy, W.L. Tibial plateau fractures. Orthopedics 1988, 11, 1527–1534. [Google Scholar] [CrossRef] [PubMed]
- Krettek, C.; Hawi, N.; Jagodzinski, M. Intracondylar segment osteotomy: Correction of intra-articular malalignment after fracture of the tibial plateau. Unfallchirurg 2013, 116, 413–426. [Google Scholar] [CrossRef]
- Papagelopoulos, P.J.; Partsinevelos, A.A.; Themistocleous, G.S.; Mavrogenis, A.F.; Korres, D.S.; Soucacos, P.N. Complications after tibia plateau fracture surgery. Injury 2006, 37, 475–484. [Google Scholar] [CrossRef]
- Marti, R.K.; Kerkhoffs, G.M.; Rademakers, M.V. Correction of lateral tibial plateau depression and valgus malunion of the proximal tibia. Oper. Orthop. Traumatol. 2007, 19, 101–113. [Google Scholar] [CrossRef] [Green Version]
- Kerkhoffs, G.M.; Rademakers, M.V.; Altena, M.; Marti, R.K. Combined intra-articular and varus opening wedge osteotomy for lateral depression and valgus malunion of the proximal part of the tibia. J. Bone Jt. Surg. Am. 2008, 90, 1252–1257. [Google Scholar] [CrossRef]
- Insall, J.N.; Dorr, L.D.; Scott, R.D.; Scott, W.N. Rationale of the Knee Society clinical rating system. Clin. Orthop. Relat. Res. 1989, 248, 13–14. [Google Scholar] [CrossRef]
- Yang, P.; Du, D.; Zhou, Z.; Lu, N.; Fu, Q.; Ma, J.; Zhao, L.; Chen, A. 3D printing-assisted osteotomy treatment for the malunion of lateral tibial plateau fracture. Injury 2016, 47, 2816–2821. [Google Scholar] [CrossRef]
- Mastrokalos, D.S.; Panagopoulos, G.N.; Koulalis, D.; Soultanis, K.C.; Kontogeorgakos, V.A.; Papagelopoulos, P.J. Reconstruction of a Neglected Tibial Plateau Fracture Malunion with an Open-Book Osteotomy: A Case Report. JBJS Case Connect. 2017, 7, e21. [Google Scholar] [CrossRef]
- Kfuri, M.; Schatzker, J. Corrective Intra-articular Osteotomies for Tibial Plateau Malunion. J. Knee Surg. 2017, 30, 784–792. [Google Scholar] [PubMed]
- Fürnstahl, P.; Vlachopoulos, L.; Schweizer, A.; Fucentese, S.F.; Koch, P.P. Complex Osteotomies of Tibial Plateau Malunions Using Computer-Assisted Planning and Patient-Specific Surgical Guides. J. Orthop. Trauma 2015, 29, e270–e276. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Nielen, D.L.; Smith, C.S.; Helfet, D.L.; Kloen, P. Early Revision Surgery for Tibial Plateau Non-union and Mal-union. HSS J. 2017, 13, 81–89. [Google Scholar] [CrossRef] [Green Version]
- Pagkalos, J.; Molloy, R.; Snow, M. Bi-planar intra-articular deformity following malunion of a Schatzker V tibial plateau fracture: Correction with intra-articular osteotomy using patient-specific guides and arthroscopic resection of the tibial spine bone block. Knee 2018, 25, 959–965. [Google Scholar] [CrossRef] [PubMed]
- Hosokawa, T.; Arai, Y.; Nakagawa, S.; Kubo, T. Total knee arthroplasty with corrective osteotomy for knee osteoarthritis associated with malunion after tibial plateau fracture: A case report. BMC Res. Notes 2017, 10, 223. [Google Scholar] [CrossRef]
- Saengnipanthkul, S. Uni-condyle high tibial osteotomy for malunion of medial plateau fracture: Surgical technique and case report. J. Med. Assoc. Thai. 2012, 95, 1619–1624. [Google Scholar]
- Wu, C.C. Salvage of proximal tibial malunion or nonunion with the use of angled blade plate. Arch. Orthop. Trauma Surg. 2006, 126, 82–87. [Google Scholar] [CrossRef]
- Keller, C.S. The principles of the treatment of tibial shaft fractures: A review of 10,146 cases from the literature. Orthopedics 1983, 6, 993–999. [Google Scholar] [CrossRef]
- Johnson, E.E. Multiplane correctional osteotomy of the tibia for diaphyseal malunion. Clin. Orthop. Relat. Res. 1987, 215, 223–232. [Google Scholar] [CrossRef]
- Paley, D.; Chaudray, M.; Pirone, A.M.; Lentz, P.; Kautz, D. Treatment of malunions and mal-nonunions of the femur and tibia by detailed preoperative planning and the Ilizarov techniques. Orthop. Clin. N. Am. 1990, 21, 667–691. [Google Scholar] [CrossRef]
- Wu, C.C.; Chen, W.J.; Shih, C.H. Tibial shaft malunion treated with reamed intramedullary nailing: A revised technique. Arch. Orthop. Trauma Surg. 2000, 120, 152–156. [Google Scholar] [CrossRef] [PubMed]
- Murphy, S.B.; Simon, S.R.; Kijewski, P.K.; Wilkinson, R.H.; Griscom, N.T. Femoral anteversion. J. Bone Jt. Surg. Am. 1987, 69, 1169–1176. [Google Scholar] [CrossRef]
- Graehl, P.M.; Hersh, M.R.; Heckman, J.D. Supramalleolar osteotomy for the treatment of symptomatic tibial malunion. J. Orthop. Trauma 1987, 1, 281–292. [Google Scholar] [CrossRef]
- Mast, J.W.; Teitge, R.A.; Gowda, M. Preoperative planning for the treatment of nonunions and the correction of malunions of the long bones. Orthop. Clin. N. Am. 1990, 21, 693–714. [Google Scholar] [CrossRef]
- Sanders, R.; Anglen, J.O.; Mark, J.B. Oblique osteotomy for the correction of tibial malunion. J. Bone Jt. Surg. Am. 1995, 77, 240–246. [Google Scholar] [CrossRef]
- Sangeorzan, B.J.; Hansen, S.T.; Judd, R.P. Mathematically directed single-cut osteotomy for correction of tibial malunion. J. Orthop. Trauma 1989, 3, 267–275. [Google Scholar] [CrossRef]
- Mayo, K.A.; Benirschke, S.K. Treatment of tibial malunions and nonunions with reamed intramedullary nails. Orthop. Clin. N. Am. 1990, 21, 715–724. [Google Scholar] [CrossRef]
- Feldman, D.S.; Shin, S.S.; Madan, S.; Koval, K.J. Correction of tibial malunion and nonunion with six-axis analysis deformity correction using the Taylor Spatial Frame. J. Orthop. Trauma 2003, 17, 549–554. [Google Scholar] [CrossRef] [Green Version]
- Purcell, K.F.; Russell, G.V.; Graves, M.L. The Clamshell Osteotomy for Diaphyseal Malunion in Deformity Correction and Fracture Surgery. Medicina (Kaunas) 2021, 57, 951. [Google Scholar] [CrossRef]
- Fragomen, A.T.; Kurtz, A.; Barclay, J.R.; Nguyen, J.; Rozbruch, S.R. A Comparison of Femoral Lengthening Methods Favors the Magnetic Internal Lengthening Nail When Compared with Lengthening Over a Nail. HSS J. 2018, 14, 166–176. [Google Scholar] [CrossRef] [PubMed]
- Zelle, B.A.; Bhandari, M.; Espiritu, M.; Koval, K.J.; Zlowodzki, M. Treatment of distal tibia fractures without articular involvement: A systematic review of 1125 fractures. J. Orthop. Trauma 2006, 20, 76–79. [Google Scholar] [CrossRef] [PubMed]
- Kane, J.M.; Raikin, S.M. Addressing hindfoot arthritis with concomitant tibial malunion or nonunion with retrograde tibiotalocalcaneal nailing: A novel treatment approach. J. Bone Jt. Surg. Am. 2014, 96, 574–580. [Google Scholar] [CrossRef] [PubMed]
- Schoenleber, S.J.; Hutson, J.J., Jr. Treatment of hypertrophic distal tibia nonunion and early malunion with callus distraction. Foot Ankle Int. 2015, 36, 400–407. [Google Scholar] [CrossRef]
- Nehme, A.; Tannous, Z.; Wehbe, J.; Mecharrafieh, R.; Maalouf, G. Arthroscopically assisted reconstruction and percutaneous screw fixation of a pilon tibial malunion. J. Foot Ankle Surg. 2007, 46, 502–507. [Google Scholar] [CrossRef]
- Rammelt, S.; Zwipp, H. Intra-articular Osteotomy for Correction of Malunions and Nonunions of the Tibial Pilon. Foot Ankle Clin. 2016, 21, 63–76. [Google Scholar] [CrossRef]
- Rademakers, M.V.; Kerkhoffs, G.M.M.J.; Sierevelt, I.N.; Raaymakers, E.L.F.B.; Marti, R.K. Operative treatment of 109 tibial plateau fractures: Five- to 27-year follow-up results. J. Orthop. Trauma 2007, 21, 5–10. [Google Scholar] [CrossRef]
- van der Schoot, D.K.; Outer, A.J.D.; Bode, P.J.; Obermann, W.R.; Van Vugt, A.B. Degenerative changes at the knee and ankle related to malunion of tibial fractures. 15-year follow-up of 88 patients. J. Bone Jt. Surg. Br. 1996, 78, 722–725. [Google Scholar] [CrossRef]
- Weinberg, D.S.; Park, P.J.; Liu, R.W. Association between Tibial Malunion Deformity Parameters and Degenerative Hip and Knee Disease. J. Orthop. Trauma 2016, 30, 510–515. [Google Scholar] [CrossRef]
- Milner, S.A.; Davis, T.R.C.; Muir, K.R.; Greenwood, D.C.; Doherty, M. Long-term outcome after tibial shaft fracture: Is malunion important? J. Bone Jt. Surg. Am. 2002, 84, 971–980. [Google Scholar] [CrossRef]
- Tarr, R.R.; Resnick, C.T.; Wagner, K.S.; Sarmiento, A. Changes in tibiotalar joint contact areas following experimentally induced tibial angular deformities. Clin. Orthop. Relat. Res. 1985, 199, 72–80. [Google Scholar] [CrossRef]
- AONA Trauma. Online Osteotomy Course Week 1 [Video]. YouTube. Available online: https://www.youtube.com/watch?v=REFXfzoHUY0&t=39s (accessed on 18 April 2020).



| Study | Patients (#) | Surgical Treatment | Outcomes | |
|---|---|---|---|---|
| Lateral | Marti et al. | 21 | Oblique osteotomy w/open-wedge osteotomy for lower-limb alignment correction | Increased range of motion (mean 12°); correction of tibial plateau depression |
| Kerkhoffs et al. | 23 | Combined intra-articular and varus opening-wedge osteotomy | Varus deformities and depression were corrected | |
| Mastrokalos et al. | 1 | Reconstruction w/open-book osteotomy | Pain-free; angular deformity corrected; restoration of normal joint congruency, and alignment of axis of knee; function was at preinjury level at latest follow up | |
| Kfuri and Schatzker | 1 | Intra-articular osteotomy | Pain resolved, range of motion restored, alignment restored | |
| Furnstahl et al. | 1 | Computer-assisted corrective osteotomy w/patient-specific guides | Pain improved in all patients | |
| Van Nielen DL et al. | 1 | Revision surgery of tibial plateau involving intra/extra articular osteotomy (1); anterolateral osteotomy (1) | Pain was alleviated, and full range of motion was achieved | |
| Furnstahl et al. | 1 | Computer-assisted corrective osteotomy w/patient-specific guides | Pain improved in all patients | |
| Yang Di et al. | 7 | 3D-printing-assisted corrective osteotomy | Statistically significant improvements in anatomy and function achieved | |
| Medial | Pagkalos et al. | 1 | Opening-wedge, hemi-tibial plateau intra-articular corrective osteotomy | Symmetrical bony anatomy achieved |
| Furnstahl et al. | 1 | Computer-assisted corrective osteotomy w/patient-specific guides | Pain improved in all patients | |
| Saengnipanthkul | 1 | Unicondyle high-tibial osteotomy | Restored medial tibial plateau and medial posterior slope | |
| Kfuri and Schatzker | 1 | Medial wedge-opening osteotomy | Bone healing, full range of motion, and return to normal activity | |
| Hosokawa et al. | 1 | Corrective osteotomy | Pain resolved; ROM preserved | |
| Posteromedial | Kfuri and Schatzker | 1 | Corrective osteotomy | ROM restored, return to work activities |
| Bicondylar | Wu CC | 14 | Transverse subtubercle osteotomy with lateral open-wedge medial blade plate | Varus deformities were corrected |
| Van Nielen DL et al. | 1 | Revision surgery of tibial plateau involving intra/extra articular osteotomy (1); anterolateral osteotomy (1) | Pain was alleviated, and full range of motion was achieved | |
| Plateau Widening | Kfuri and Schatzker | 1 | Intra-articular closing-wedge osteotomy | Normal alignment, full ROM achieved, pain-free |
| Study | Patients (#) | Malunion Deformity | Post-Surgical Alignment | |
|---|---|---|---|---|
| Lateral | Marti et al. | 21 | Valgus deformity < 20 degrees; lateral plateau depression < 20 mm | Mean improvement of tibiofibular angle (8.6 degrees); mean improvement in lateral plateau depression (6 mm) |
| Kerkhoffs et al. | 23 | Mean valgus deformity 13 degrees; mean plateau depression 7.7 mm | Mean tibiofibular angle 4.4 degrees; mean lateral plateau depression 1.7 mm | |
| Mastrokalos et al. | 1 | 20-degree valgus deformity with >15 mm lateral plateau depression | No angular deformity or plateau depression | |
| Kfuri and Schatzker | 1 | 5 mm | Normal alignment | |
| Furnstahl et al. | 1 | Plateau depression 3.6 mm; coronal deformity 10; sagittal deformity 7.0 degrees; torsional deformity 12.8 | Plateau depression 1.1 mm; coronal deformity improved to 0.5 degrees; sagittal deformity improved to 1.8 degrees; torsional deformity improved to 1.2 degrees. | |
| Van Nielen DL et al. | 1 | Valgus deformity 8 degrees with posterolateral fragment depression 3 mm | Normal alignment | |
| Furnstahl et al. | 1 | Plateau depression 1.3 mm; coronal deformity 2.4 degrees; sagittal deformity 14.9 degrees; torsional deformity 1.8 degrees | Plateau depression improved to 0.2 mm; coronal deformity worsened to 3.5 degrees; sagittal deformity improved to 4.1 degrees; torsional deformity improved to 0.3 degrees | |
| Yang Di et al. | 7 | Mean plateau depression of 9.4 mm | Plateau depression <1 mm for all patients | |
| Medial | Pagkalos et al. | 1 | Plateau depression 15 mm 9 degrees coronal deformity | Normal alignment |
| Furnstahl et al. | 1 | Plateau depression 6.5 mm; coronal deformity 7.8 degrees; sagittal deformity 2.6 degrees; torsional deformity 2.5 degrees | Plateau depression improved to 1.0 mm; coronal deformity improved to 1.5 degrees; sagittal deformity improved to 0.4 degrees; torsional deformity improved to 0.8 degrees. | |
| Saengnipanthkul | 1 | 15-degree varus deformity; posteromedial slope 29 degrees; | Restored medial tibial plateau and medial posterior slope | |
| Kfuri and Schatzker | 1 | 25-degree varus 5 mm depression | Normal alignment | |
| Hosokawa et al. | 1 | 9-degree varus deformity; 27 degree flexion deformity | Total knee arthroplasty | |
| Posteromedial | Kfuri and Schatzker | 1 | 27-degree varus deformity 5 mm depressed | Normal alignment |
| Bicondylar | Wu CC | 14 | Varus knees with proximal medial tibial angle avg of 72 degrees | Proximal medial tibial angle improved to avg 88 degrees |
| Van Nielson DL et al. | Not stated | Normal alignment | ||
| Plateau Widening | Kfuri and Schatzker | 1 | Not stated | Normal alignment |
| Study | Patients (#) | Surgical Treatment | Outcomes |
|---|---|---|---|
| Graehl et al. | 8 | Supramalleolar dome osteotomy or closed-wedge osteotomy | Improvement in pain in six patients; decrease in limping for 7 patients; improvement in sagittal plane deformity in all patients; coronal plane improvement in 1 of 3 patients with significant presurgical deformity |
| Sanders et al. | 12 | Oblique osteotomy | Correction of sagittal deformity to within 2° of normal; correction in coronal plane within 1° of normal; avg 1.3 cm of lengthening obtained; full range of motion (10); full-weight bearing; and return to previous employment (10); two patients failed initial revision |
| Kempf et al. | 7 | Reamed intramedullary nail | Good correction and all healed |
| Mayo and Benirschke | 23 | Reamed intramedullary nail | All healed, 1 infection with acceptable alignment |
| Sangeorzan et al. | 4 | Single-cut oblique osteotomy | All angular deformities were corrected. One patient developed deep infection, was successfully treated, and had a positive outcome |
| Wu CC et al. | 37 | Reamed intramedullary nailing | All patients’ deformities reached <10° angulation and/or rotation and <2 cm shortening; limping gait was corrected |
| Johnson | 7 | Multiplane corrective osteotomy | Lower-leg deformity and angulation improved in all patients; 2 patients had improved back pain; ipsilateral knee pain relieved (4); ipsilateral ankle discomfort resolved (2); improved back pain (2); gait improved in all patients; fibula nonunion (4) |
| LaFrance et al. | 1 | 2 stage: corrective fibula osteotomy followed by revision ACL reconstruction | Instability resolved |
| Feldman et al. | 11 | Taylor Spatial Frame | Mean alignment: coronal angulation 1.4°, sagittal plane 0.9°, shortening 4.4 mm, rotation 0.6° |
| Lahav and DiMaio | 1 | Opening-wedge osteotomy and total knee arthroplasty | Excellent range of motion and a stable knee to varus and valgus stress. Radiographs at two years illustrated a well-seated TKA and correction of tibial alignment |
| Paley et al. | 17 | Ilizarov | Angular > 5° rotation > 15° lld > 1.5 mean 4.5 cm |
| All corrected within 1.5 cm lld angular deformity < 5° and rotation < 10° |
| Study | Patients (#) | Malunion Deformity | Post-Surgical Alignment |
|---|---|---|---|
| Graehl et al. | 8 | Varus deformity 15 degrees; one patient had an anterior sagittal plane deformity of 14 degrees; two had posterior deformities of 30 degrees and 45 degrees | Average coronal plane alignment 0 degrees; sagittal angulation was 8 degrees of recurvatum on average; only 1 of 3 patients with sagittal deformity were in neutral alignment |
| Mast et al. | 17 | >8-degree coronal, 5–40-degree sagittal, 10 IR-15 ER, leg length discrepancy 1–2 cm | Healed corrected within 5 degrees |
| Sanders et al. | 12 | Mean sagittal plane deformity 13 degrees; mean coronal plane deformity 23 degrees of procurator; average shortening 2.2 cm | Correction of sagittal deformity to within 2° of normal; correction in coronal plane within 1° of normal; avg 1.3 cm of lengthening obtained |
| Sangeorzan et al. | 4 | Varus deformity 15 degrees on average; 9.75 degrees of extension on average; 1 cm of shortening | All corrected to within acceptable limits |
| Wu CC et al. | 37 | Angular or rotational deformity, but no shortening >2 cm | All patients’ deformities reached <10° angulation and/or rotation and <2 cm shortening |
| Johnson | 7 | Varus in six patients averaged 16.6 degrees; shortening averaged 1.29 cm in six patients; posterior bowing averaged 8.2 degrees in five patients. | Lower-leg deformity and angulation improved in all patients |
| LaFrance et al. | 1 | 15-degree apex anterior; valgus 10 alignment | Normal alignment |
| Feldman et al. | 11 | Mean alignment: coronal angulation 11.7°, sagittal plane 10.3°, shortening 6.8 mm, rotation 0.6° | Mean alignment: coronal angulation 1.4°, sagittal plane 0.9°, shortening 4.4 mm, rotation 0.6° |
| Lahav and Dimaio | 1 | Varus malalignment at the knee was 12 degrees; 20-degree varus malunion of the tibia | Normal alignment |
| Paley et al. | 17 | Angular rotation >5° (avg rotation >15°) leg length discrepancy >1.5 (mean 4.5 cm) | All corrected within 1.5 cm leg length discrepancy, angular deformity < 5°, and rotation < 10° |
| Study | Patients (#) | Surgical Treatment | Outcomes |
|---|---|---|---|
| Kane and Raikin | 16 | Single-stage corrective osteotomy w/tibiotalocalcaneal nailing | VAS * pain scores improved from 8.3 to 2.8; AOFAS ** functional scores improved from 43 to 75; all deformities corrected to neutral alignment |
| Schoenleber and Hutson Jr. | 5 | Deformities corrected w/gradual opening wedge osteotomy w/lengthening when indicated | Lower-leg deformity equalized |
| Nehme et al. | 1 | Arthroscopy-assisted mobilization w/percutaneous fixation | Patient regained full physical activities; American foot and ankle score of 100 |
| Study | Patients (#) | Malunion Deformity | Post-Surgical Alignment |
|---|---|---|---|
| Kane and Raikin | 16 | Varus and recurvatum combination was the most commonly seen deformity; average sagittal plane malalignment was 26°, and the average coronal plane malalignment was 21° | All deformities corrected to neutral alignment |
| Schoenleber and Hutson Jr. | 5 | Varus deformities (8–19 degrees);valgus deformities (16 degrees); apex anterior deformities (2–21 degrees); apex posterior deformity (range, 9–20 degrees). | Lower-leg deformity neutralized to less than 5 degrees angulation in all TSF patients and to less than 5 degrees in one plane and less than 10 degrees in the second with the Ilizarov |
| Nehme et al. | 1 | Malunited medial malleolus | Within normal limits |
| Rammelt and Zwipp | 14 | Malunited pilon fractures treated with intra-articular osteotomy presented at 3 mo | 5-year follow up Excellent 1, good 9, fair 2 poor 2 7 revision surgeries and 2 arthrodesis |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Patel, I.; Young, J.; Washington, A.; Vaidya, R. Malunion of the Tibia: A Systematic Review. Medicina 2022, 58, 389. https://doi.org/10.3390/medicina58030389
Patel I, Young J, Washington A, Vaidya R. Malunion of the Tibia: A Systematic Review. Medicina. 2022; 58(3):389. https://doi.org/10.3390/medicina58030389
Chicago/Turabian StylePatel, Ishan, Jacob Young, Austen Washington, and Rahul Vaidya. 2022. "Malunion of the Tibia: A Systematic Review" Medicina 58, no. 3: 389. https://doi.org/10.3390/medicina58030389
APA StylePatel, I., Young, J., Washington, A., & Vaidya, R. (2022). Malunion of the Tibia: A Systematic Review. Medicina, 58(3), 389. https://doi.org/10.3390/medicina58030389






