1. Introduction
Osteoarthritis (OA) of the knee joint is a progressive degenerative joint disease affecting 10 to 15% in the age group over 60 years [
1], with more than 250 million affected people worldwide [
2]. Symptoms include pain, stiffness, joint function loss, muscle atrophy, swelling, and reduced mobility [
3]. The main risk factors are age, female gender, genetic predisposition, anatomical anomalies, body mass index above 25 kg/m
2, injuries, and heavy physical work [
4,
5].
Kellgren and Lawrence distinguished four stages [
6]: grade 0 (none), definite absence of X-ray changes of OA; grade 1 (doubtful), doubtful joint space narrowing and possible osteophytic lipping; grade 2 (minimal), definite osteophytes, and potential joint space narrowing; grade 3 (moderate), moderate multiple osteophytes, definite narrowing of joint space and some sclerosis, and possible deformity of bone ends; grade 4 (severe), large osteophytes, marked narrowing of joint space, severe sclerosis, and definite deformity of bone ends [
6]. Conservative therapies are beneficial for patients in grade 1 to 3, while grade 4 usually requires surgical intervention [
7].
Several studies have shown that physiotherapy mitigates the symptoms of knee OA [
8]. Exercises increasing strength and flexibility are most effective. These positive effects are maintained for two to six months after completion of formal treatment [
9].
Although it remains controversial, orally administered components of the extracellular matrix (viscosupplementation), in particular glucosamine sulfate and chondroitin sulfate, might relieve pain in joints of lower extremities, including knee [
10,
11,
12,
13]. Positive effects of viscosupplementation on stiffness and functionality have also been described [
14,
15].
In case of varus deviation of the leg axes, shoe insoles with lateral hindfoot wedges can reduce the adduction moment, thereby relieving the medial compartment [
16]. A meta-analysis of several studies estimated a pain reduction of 1 point on a scale of 0 to 10, while flat insoles yielded a pain reduction of 0.3 points [
17]. In general, insoles are comfortable to wear in shoes and have high compliance. An alternative for this is a soft knee brace. This can align the leg axis and, thus, relieve the medial compartment of the knee [
18,
19].
There are plenty of other conservative therapies. While some, such as dry needling, have been shown to be not effective [
20], others, such as manual therapy, intra-articular viscosupplementation with hyaluronic acid, or platelet rich plasma treatment, have been reported to be effective [
21,
22,
23]. In addition, the gut microbiome could have an impact on the inflammation and pain of OA, but this is still poorly understood [
24].
Most previous studies described the effect of individual forms of therapy, but combinations remain underexplored. In this study, patients with varus knee OA were treated with a conservative trio-therapy, a combination of varus-reducing hindfoot shoe-insoles, oral viscosupplementation, and physiotherapy. We hypothesized that this conservative trio-therapy would reduce pain and improve measured scores in patients with varus knee OA.
2. Materials and Methods
2.1. Patient Recruitment
In this prospective case-study, all patients received the same trio-therapy and were followed for 6 months. Patients were recruited through referrals from general practitioners over a seven-month period. The inclusion criteria were unilateral or bilateral unicompartmental isolated medial varus knee OA with varus > 5° in orthoradiogram/lower limb radiography and Kellgren-Lawrence Grade II to III OA with-out any signs of lateral knee OA or patellofemoral OA in the MRI, age between 18 and 80 years, willingness to participate in the study, and signed patient’s informed consent. The exclusion criteria were unicompartmental medial varus knee OA with Kellgren-Lawrence Grade I or IV, varus knee OA with lateral or patellofemoral OA, valgus knee OA, patellofemoral OA, complete tri-compartmental knee OA, other diseases of the knee joint (e.g., lesions of the anterior or posterior cruciate ligament, lesions of the medial or lateral meniscus, collateral ligament lesions, arthritis, etc.), age < 18 years and >80 years, hip OA, OA of the ankle joint or foot, other leg or spinal disorders, neuromuscular diseases, rheumatoid diseases, osteoporosis, obesity with BMI > 30 kg/m2, and lack of willingness to perform the conservative trio-therapy. With these strict inclusion and exclusion criteria, 80% of the patients had to be excluded from the study. For example, these common combinations had to be excluded: medial degeneration Grade IV, or medial degeneration with medial meniscus degeneration/tear, medial degeneration with patellofemoral OA, and others. In total 12 ‘absolute clean’ patients could be recruited.
2.2. Conservative Trio-Therapy
All patients received a standardized trio-therapy with corrective shoe-insoles, oral viscosupplementation, and physiotherapy for six months.
The orthopedic insoles were equipped with a varus-reducing lateral hindfoot wedge to reduce the leg’s varus, i.e., the knee axis’s lateralizing position; thus, relieving the knee OA medially. For each degree in varus, a correction of 1 mm wedge height was implemented in the lateral orthopedic insole. The insoles were all performed by the same orthopedic technician and fitted in flat mid-height shoes with hard soles. The patients were instructed to wear the shoe throughout the entire day.
Oral viscosupplementation: patients ingested one sachet (21.8 g) of ExtraCellMatrix ECM® Drink (Swiss Alp Health, Belmont-sur-Lausanne, Switzerland) once daily for the first three months. According to Swiss Alp Health recommendations, maintenance dosing during months four to six was two to three sachets per week. The ExtraCellMatrix ECM® Drink consisted of the following ingredients: collagen type I, II, III (10 g), glucosamine sulfate (1270 mg), chondroitin sulfate (500 mg), hyaluronic acid (100 mg), MSM (100 mg), L-lysine (400 mg), L-threonine (300 mg), rosehip, melon extract, edelweiss, gen-tian, agar–agar, paprika extract, minerals (Ca, Mn, Cu, Zn, Se), and vitamins (C, E, D3, K2).
All patients received physiotherapy twice a week for 30 min, over the entire period of six months. Uniform stretching hamstrings, quadriceps calf muscles, strength training of all periarticular knee muscles, and local anti-inflammatory measures to reduce pain and improve functionality, e.g., local lymphatic drainage, were prescribed. The exercises were adjusted to the patient, according to their pain tolerance.
2.3. Scoring
Patients were interviewed at the start of therapy and after three and six months. The level of pain was assessed with the visual analog scale (VAS) on a scale of 0 (no pain) to 10 (most severe pain) [
25]. Functional disability was calculated using the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC-Score) [
26]. This disease-specific questionnaire measures pain in specific situations, stiffness, and physical difficulty in everyday activities [
26]. The number of points achieved was converted into a percentage (%) of physical functional impairment. The average population aged 45 to 64 years achieves a functional impairment of 8% on a scale from 0 to 100%. A change of at least 10% is clinically relevant [
27].
Quality of life was assessed using the short form–36 items (SF-36) questionnaire, before starting therapy and after six months [
27]. This questionnaire records physical and mental health in eight domains. The four domains of physical health are physical functioning (PF), role-physical (RP), bodily pain (BP), and general health (GH). The four domains of mental health are vitality (VT), social functioning (SF), role-emotional (RE), and mental health (MH). The highest possible score per domain is 100 points, on a scale from 0 to 100 points and is achieved by healthy people without limitations or disabilities. The parts general health, vitality, and mental health are ‘bipolar’ and have a broader range in their coverage of negative and positive health states. Here, 50% is achieved with a neutral assessment (neither positive nor negative). One hundred points are achieved in these domains if the patients describe their state of health as positive [
28]. The values of the US-American average population served for comparison with the study results [
28].
Physical sports activity was assessed with the sports frequency score (
Table 1) on all three dates [
29].
2.4. Statistical Analysis
A power calculation before the study started resulted in a minimum number of four patients for a VAS pain score (scale from 0 to 10 points) with the following average values: before intervention OA pain VAS 6, after trio-therapy VAS 2, standard deviation 2, statistical significance p < 0.05, statistical power 0.8. A chi-square likely ratio test was used to assess the statistical significance of differences between the start and end of treatment. The significance level was set at α = 0.05. The results are depicted as average values with ± standard deviations and the range of minimum and maximum values. We also calculated minimal detectable changes (MDC) for a power of 0.8.
3. Results
Of the 12 patients initially enrolled in the study, nine patients could be thoroughly examined and interviewed till the endpoint of six months follow-up. Two patients could not be reached after the first appointment and were, therefore, excluded from the data analysis. Another patient declined the conservative therapy after the first appointment and had surgery on the affected knee. The data of the three drop-out-patients were not used. Therefore, nine patients could be used in the study: seven women and two men, with a mean age of 56 years (range, 51–63 years) and a mean varus deviation of 7° (range, 5–10°).
3.1. Pain Level
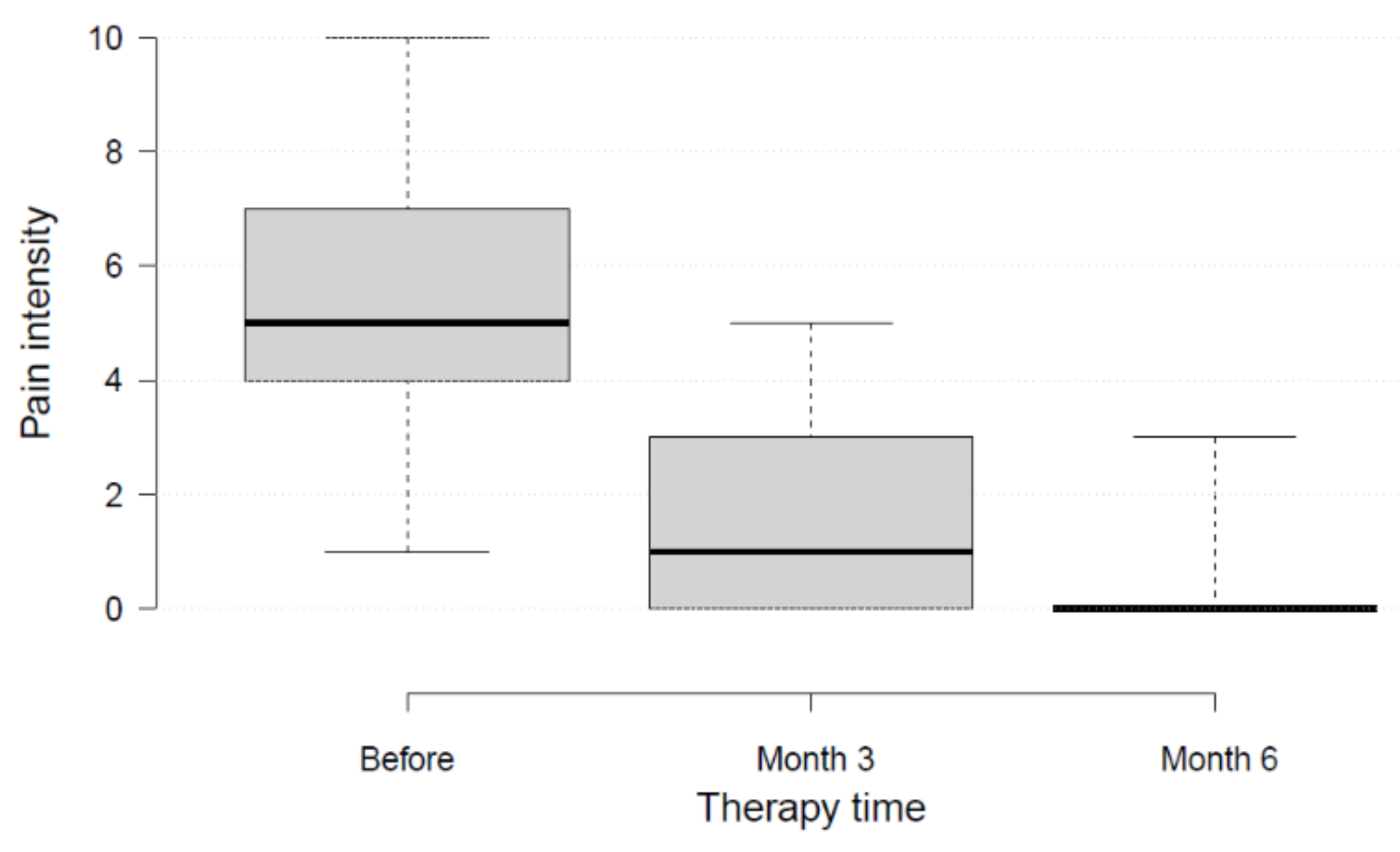
All patients reported a reduction of pain in the affected knee (
Figure 1 and
Figure 2). At the start of therapy, patients reported pain levels of VAS 5.4 ± 2.3 (range, 3–10). After three months of trio-therapy, patients reported pain levels of VAS 1.7 ± 2 (range, 0–5),
p < 0.01. After six months of therapy, patients reported pain levels closed to the minimum value possible: VAS 0.6 ± 1.1 (range, 0–3)
p < 0.01. Seven out of nine patients reported no pain at all (VAS 0) after six months. Most of the improvement was achieved within the first three months. The MDC of 2.5 was reached.
3.2. WOMAC Score
Patients had initial WOMAC scores of 35 ± 15 (range, 10–56) (
Figure 3 and
Figure 4). During therapy, values declined to 4 ± 5 (range, 0–14;
p < 0.05) after three months of therapy, and to 2 ± 4 (range, 0–9;
p < 0.01) after six months. Thus, the patients achieved better scores than the normal population in this age category [
27]. Five out of nine patients achieved the ideal value of 0. Most of the improvement was achieved within the first three months. The MDC of 16.2 was reached.
3.3. Quality of Life
The SF-36 questionnaire assessed quality of life before the start of therapy and after six months (
Figure 5). All four domains of physical health (physical functioning, role-function, bodily pain, general health) showed significant improvements (
p < 0.01). In contrast to the VAS results, the SF-36 showed complete freedom from pain in only two patients. It is important to note that the SF-36 questionnaire refers to the entire body and mental state, while in this study, the VAS only referred to the knee. It is, therefore, possible that the patients had other present problems besides the knee pain.
In the four domains of mental health, the two domains, vitality and mental health showed significant improvements (p < 0.05). The two domains role-emotional and social functioning showed only minor non-significant changes (p > 0.05). The two domains bodily pain and general health did reach the MDC, the other six domains didn’t.
3.4. Sports Frequency Score
Sports physical activity increased by at least 1 level on the sports frequency score in four out of nine patients within the first three months, and six out of nine patients after six months (
Figure 6). Running was most popular, followed by fitness, skiing, cycling, and tennis.
4. Discussion
Knee osteoarthritis (OA) is a common disease in the middle to old age. Patients with a substantial leg axis deviation (varus/valgus) are frequently affected. Surgery or joint re-placement is usually necessary in the long term. Conservative therapies can relieve pain and improve function, at least temporarily and especially in the early stages. Although various conservative treatments are effective, the possibly enhanced benefits of combinatorial therapies are underexplored. In this prospective study, it was shown that a six-month conservative trio-therapy consisting of varus-reducing hindfoot shoe-insoles with a lateral wedge, oral viscosupplementation with ECM, and physiotherapy enormously improved pain, function, quality of life, and sports activity in patients with painful varus knee OA.
The conservative trio-therapy achieved an average pain relief of 5 points (scale 0 to 10 points) and an improved WOMAC functionality of 30 points (scale 0 to 100 points). Seven out of nine patients even became entirely pain-free in the affected joint within six months. In six of the eight domains of the SF-36 questionnaire, there was a significant improvement in life quality. Physical activity also increased in six of the nine patients by at least one level on the sports frequency score.
The success of the combined trio-therapy in this study was striking compared to previous studies using monotherapies. A meta-analysis of studies on physiotherapy alone showed a pain reduction of only 1 point on a scale of 0 to 10 points and improved functionality of only 10 points on a scale of 0 to 100 points [
9]. Insoles alone with lateral side wedges resulted in a pain reduction of 1 point on a scale of 0 to 10 points in previous studies [
17]. Viscosupplementation with chondroitin sulfate alone resulted in a pain reduction of 1 point on a scale of 0 to 10 points compared to the control group [
10]. Surprisingly, the administration of chondroitin sulfate, together with glucosamine sulfate, had an even worse effect than placebo (pain reduction of only 1 point compared to 2 points with placebo) [
12]. However, the combination of physiotherapy and oral viscosupplementation (glucosamine hydrochloride, chondroitin sulfate, bio-curcumin) reduced pain by 2–3 points on VAS and improved function by about 15 points (WOMAC score) [
30]. Nevertheless, previous studies on oral viscosupplementation had methodological shortcomings because OA involving different axis deviations were pooled instead of being analyzed as varus/valgus/neutral separately. Moreover, a prerequisite for the effect of oral viscosupplementation could be that biomechanics should be improved simultaneously using corrective insoles and physiotherapy.
Assuming purely additive effects of the individual components, a pain reduction of 4 points could be expected for the conservative trio-therapy, based on the study data to date. This value is close to the observed results of the present study, of 5 points. Additive effects are compatible with the targeting of different pathophysiological aspects. Overall, the pain reduction and improved function were highly effective, suggesting this conservative combination therapy as the first choice treatment in varus knee OA.
This study has limitations. The patient population of nine patients was small. Nevertheless, according to the power calculation, this was more than sufficient to answer the question. Furthermore, there was no control group in this prospective case-study, so that part of the improvement could have been based on the placebo effect. Therefore, it is not known how much of the changes can be attributed to the three forms of treatment together. Double-blinding is not possible for physiotherapy and insoles, so that the placebo effect cannot be determined precisely. Observations with flat insoles without side wedges suggest only a minimal placebo effect for insoles with lateral side wedges [
17]. A possible placebo effect for oral viscosupplementation was demonstrated, in the range of a maximal 2 points (pain scale from 0 to 10) [
12].
Furthermore, the study had a duration of only six months. Therefore, it is unclear how long the pain reduction lasts and how long a surgical intervention can be delayed compared to patients without a conservative trio-therapy. These questions should be clarified in future studies.
5. Conclusions
The conservative trio-therapy with varus-reducing hindfoot shoe-insoles with a lateral wedge, oral viscosupplementation with ECM, and physiotherapy in patients with varus knee OA showed positive initial clinical results: less pain, higher function, better quality of life, and higher sport activity. Further studies are required to evaluate the long-term effect. If this trio-therapy should become established in daily clinical practice, it would provide a treatment option for most patients with varus knee OA.
Author Contributions
Conceptualization V.V.; methodology V.V.; formal analysis L.P.; investigation V.V., D.H. and L.P.; resources V.V.; data curation L.P.; writing—original draft preparation L.P.; writing—review and editing V.V., D.H., C.C., T.H. and A.B.; visualization L.P.; supervision V.V. All authors have read and agreed to the published version of the manuscript.
Funding
This research had no special funding. See acknowledgments.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee Northwest and Central Switzerland (Project-ID: 2017-01977 on 22 November 2017.)
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available, due to privacy and ethics.
Acknowledgments
We thank Miranda Bunjaku for the administrative support. We would like to thank Patrick Winkler, Ortho Schuh Technik Winkler AG, Basel, Switzerland, for production and cost absorption of the insoles. We would like to thank Swiss Alp Health for providing the oral viscosupplementation ECM for free. Finally, we would like to thank the patients for their participation.
Conflicts of Interest
The authors declare no conflict of interest.
References
- O’Neill, T.W.; McCabe, P.S.; McBeth, J. Update on the epidemiology, risk factors and disease outcomes of osteoarthritis. Best Pract. Res. Clin. Rheumatol. 2018, 32, 312–326. [Google Scholar] [CrossRef] [PubMed]
- Vos, T.; Flaxman, A.D.; Naghavi, M.; Lozano, R.; Michaud, C.; Ezzati, M.; Shibuya, K.; Salomon, J.A.; Abdalla, S.; Aboyans, V.; et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2163–2196. [Google Scholar] [CrossRef] [PubMed]
- Hussain, S.M.; Neilly, D.W.; Baliga, S.; Patil, S.; Meek, R. Knee osteoarthritis: A review of management options. Scott. Med. J. 2016, 61, 7–16. [Google Scholar] [CrossRef]
- Zhang, W.; McWilliams, D.F.; Ingham, S.L.; Doherty, S.A.; Muthuri, S.; Muir, K.R.; Doherty, M. Nottingham knee osteoarthritis risk prediction models. Ann. Rheum. Dis. 2011, 70, 1599–1604. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Valdes, A.M.; Spector, T.D. Genetic epidemiology of hip and knee osteoarthritis. Nat. Rev. Rheumatol. 2010, 7, 23. [Google Scholar] [CrossRef] [PubMed]
- Kellgren, J.H.; Lawrence, J.S. Radiological assessment of osteo-arthrosis. Ann. Rheum. Dis. 1957, 16, 494–502. [Google Scholar] [CrossRef] [Green Version]
- Vaishya, R.; Pariyo, G.B.; Agarwal, A.K.; Vijay, V. Non-operative management of osteoarthritis of the knee joint. J. Clin. Orthop. Trauma 2016, 7, 170–176. [Google Scholar] [CrossRef] [Green Version]
- Van Ginckel, A.; Hall, M.; Dobson, F.; Calders, P. Effects of long-term exercise therapy on knee joint structure in people with knee osteoarthritis: A systematic review and meta-analysis. Semin. Arthritis Rheum. 2019, 48, 941–949. [Google Scholar] [CrossRef]
- Fransen, M.; McConnell, S.; Harmer, A.R.; Van der Esch, M.; Simic, M.; Bennell, K.L. Exercise for osteoarthritis of the knee: A Cochrane systematic review. Br. J. Sports Med. 2015, 49, 1554–1557. [Google Scholar] [CrossRef]
- Singh, J.A.; Noorbaloochi, S.; MacDonald, R.; Maxwell, L.J. Chondroitin for osteoarthritis. Cochrane Database Syst. Rev. 2015, 1, Cd005614. [Google Scholar] [CrossRef] [Green Version]
- Ogata, T.; Ideno, Y.; Akai, M.; Seichi, A.; Hagino, H. Effects of glucosamine in patients with osteoarthritis of the knee: A systematic review and meta-analysis. Clin. Rheumatol. 2018, 37, 2479–2487. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roman-Blas, J.A.; Castaneda, S.; Sanchez-Pernaute, O.; Largo, R.; Herrero-Beaumont, G. Combined Treatment with Chondroitin Sulfate and Glucosamine Sulfate Shows No Superiority Over Placebo for Reduction of Joint Pain and Functional Impairment in Patients with Knee Osteoarthritis: A Six-Month Multicenter, Randomized, Double-Blind, Placebo-Controlled Clinical Trial. Arthritis Rheumatol. 2017, 69, 77–85. [Google Scholar] [CrossRef] [Green Version]
- Simental-Mendia, M.; Sanchez-Garcia, A.; Vilchez-Cavazos, F.; Acosta-Olivo, C.A.; Pena-Martinez, V.M.; Simental-Mendia, L.E. Effect of glucosamine and chondroitin sulfate in symptomatic knee osteoarthritis: A systematic review and meta-analysis of randomized placebo-controlled trials. Rheumatol. Int. 2018, 38, 1413–1428. [Google Scholar] [CrossRef] [PubMed]
- Hochberg, M.C.; Martel-Pelletier, J.; Monfort, J.; Moller, I.; Castillo, J.R.; Arden, N.; Berenbaum, F.; Blanco, F.J.; Conaghan, P.G.; Domenech, G.; et al. Combined chondroitin sulfate and glucosamine for painful knee osteoarthritis: A multicentre, randomised, double-blind, non-inferiority trial versus celecoxib. Ann. Rheum. Dis. 2016, 75, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Machado, G.C.; Eyles, J.P.; Ravi, V.; Hunter, D.J. Dietary supplements for treating osteoarthritis: A systematic review and meta-analysis. Br. J. Sports Med. 2018, 52, 167–175. [Google Scholar] [CrossRef] [Green Version]
- Shaw, K.E.; Charlton, J.M.; Perry, C.K.L.; de Vries, C.M.; Redekopp, M.J.; White, J.A.; Hunt, M.A. The effects of shoe-worn insoles on gait biomechanics in people with knee osteoarthritis: A systematic review and meta-analysis. Br. J. Sports Med. 2018, 52, 238–253. [Google Scholar] [CrossRef] [Green Version]
- Parkes, M.J.; Maricar, N.; Lunt, M.; LaValley, M.P.; Jones, R.K.; Segal, N.A.; Takahashi-Narita, K.; Felson, D.T. Lateral wedge insoles as a conservative treatment for pain in patients with medial knee osteoarthritis: A meta-analysis. JAMA 2013, 310, 722–730. [Google Scholar] [CrossRef] [Green Version]
- Moyer, R.F.; Birmingham, T.B.; Bryant, D.M.; Giffin, J.R.; Marriott, K.A.; Leitch, K.M. Biomechanical effects of valgus knee bracing: A systematic review and meta-analysis. Osteoarthr. Cartil. 2015, 23, 178–188. [Google Scholar] [CrossRef] [Green Version]
- Dessinger, G.M.; LaCour, M.T.; Dennis, D.A.; Kleeman-Forsthuber, L.T.; Komistek, R.D. Can an OA Knee Brace Effectively Offload the Medial Condyle? An In Vivo Fluoroscopic Study. J. Arthroplast. 2021, 36, 1455–1461. [Google Scholar] [CrossRef]
- Sánchez Romero, E.A.; Fernández-Carnero, J.; Calvo-Lobo, C.; Ochoa Sáez, V.; Burgos Caballero, V.; Pecos-Martín, D. Is a Combination of Exercise and Dry Needling Effective for Knee OA? Pain Med. 2020, 1, 349–363. [Google Scholar] [CrossRef]
- Sánchez-Romero, E.A.; González-Zamorano, Y.; Arribas-Romano, A.; Martínez-Pozas, O.; Fernández Espinar, E.; Pedersini, P.; Villafañe, J.H.; Alonso Pérez, J.L.; Fernández-Carnero, J. Efficacy of Manual Therapy on Facilitatory Nociception and Endogenous Pain Modulation in Older Adults with Knee Osteoarthritis: A Case Series. Appl. Sci. 2021, 11, 1895. [Google Scholar] [CrossRef]
- Tsokanos, A.; Livieratou, E.; Billis, E.; Tsekoura, M.; Tatsios, P.; Tsepis, E.; Fousekis, K. The Efficacy of Manual Therapy in Patients with Knee Osteoarthritis: A Systematic Review. Medicina 2021, 57, 696. [Google Scholar] [CrossRef] [PubMed]
- Tognolo, L.; Maccarone, M.C.; De Trane, S.; Scanu, A.; Masiero, S.; Fiore, P. Therapeutic Exercise and Conservative Injection Treatment for Early Knee Osteoarthritis in Athletes: A Scoping Review. Medicina 2022, 58, 69. [Google Scholar] [CrossRef] [PubMed]
- Sánchez Romero, E.A.; Meléndez Oliva, E.; Alonso Pérez, J.L.; Martín Pérez, S.; Turroni, S.; Marchese, L.; Villafañe, J.H. Relationship between the Gut Microbiome and Osteoarthritis Pain: Review of the Literature. Nutrients 2021, 13, 716. [Google Scholar] [CrossRef] [PubMed]
- Huskisson, E.C. Measurement of pain. Lancet 1974, 2, 1127–1131. [Google Scholar] [CrossRef]
- Bellamy, N.; Buchanan, W.W.; Goldsmith, C.H.; Campbell, J.; Stitt, L.W. Validation study of WOMAC: A health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J. Rheumatol. 1988, 15, 1833–1840. [Google Scholar] [PubMed]
- Marot, V.; Murgier, J.; Carrozzo, A.; Reina, N.; Monaco, E.; Chiron, P.; Berard, E.; Cavaignac, E. Determination of normal KOOS and WOMAC values in a healthy population. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 541–548. [Google Scholar] [CrossRef]
- Ware, J.E.; Sherbourne, C.D. The MOS 36-Item Short-Form Health Survey (SF-36): I. Conceptual Framework and Item Selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef]
- Valderrabano, V.; Pagenstert, G.; Horisberger, M.; Knupp, M.; Hintermann, B. Sports and recreation activity of ankle arthritis patients before and after total ankle replacement. Am. J. Sports Med. 2006, 34, 993–999. [Google Scholar] [CrossRef]
- Sterzi, S.; Giordani, L.; Morrone, M.; Lena, E.; Magrone, G.; Scarpini, C.; Milighetti, S.; Pellicciari, L.; Bravi, M.; Panni, I.; et al. The efficacy and safety of a combination of glucosamine hydrochloride, chondroitin sulfate and bio-curcumin with exercise in the treatment of knee osteoarthritis: A randomized, double-blind, placebo-controlled study. Eur. J. Phys. Rehabil. Med. 2016, 52, 321–330. [Google Scholar]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).