Paraneoplastic Wong-Type Dermatomyositis Associated with Gynecological Malignancy
Abstract
:1. Introduction
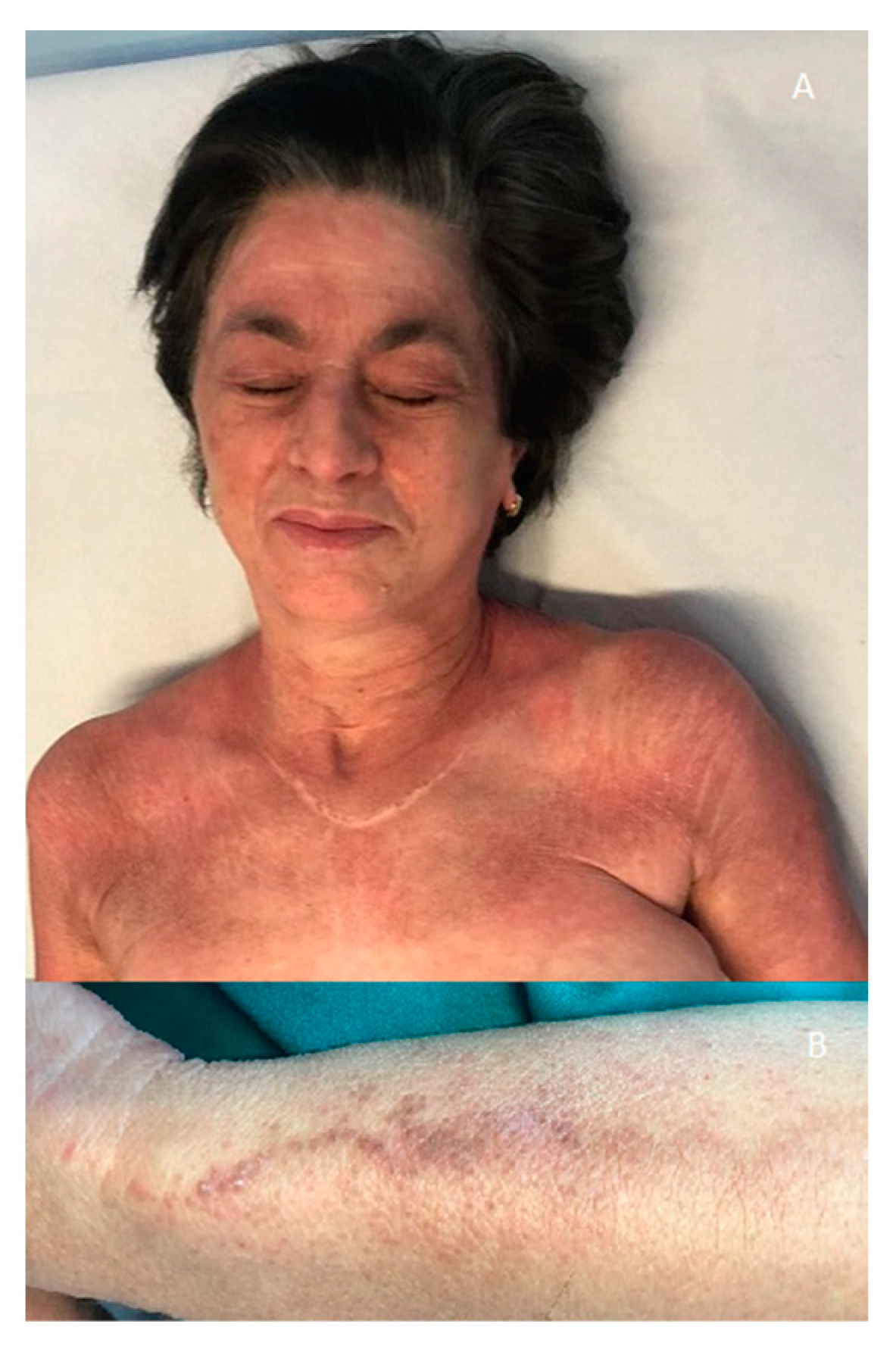
2. Case Report
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schlecht, N.; Sunderkötter, C.; Niehaus, S.; Nashan, D. Update on dermatomyositis in adults. J. Dtsch. Dermatol. Ges. 2020, 18, 995–1013. [Google Scholar] [CrossRef] [PubMed]
- Mutasim, D.F.; Egesi, A.; Spicknall, K.E. Wong-type Dermatomyositis: A mimic of many dermatoses. J. Cutan. Pathol. 2016, 43, 781–786. [Google Scholar] [CrossRef] [PubMed]
- Didona, D.; Fania, L.; Didona, B.; Eming, R.; Hertl, M.; Di Zenzo, G. Paraneoplastic dermatoses: A brief general review and an extensive analysis of paraneoplastic pemphigus and paraneoplastic dermatomyositis. Int. J. Mol. Sci. 2020, 21, 2178. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lundberg, I.E.; Tjarnlund, A.; Bottai, M.; Werth, V.P.; Pilkington, C.; de Visser, M.; Alfredsson, L.; Amato, A.A.; Barohn, R.J.; Liang, M.H.; et al. 2017 European League Against Rheumatism/American College of Rheumatology classification criteria for adult and juvenile idiopathic inflammatory myopathies and their major subgroups. Arthritis Rheumatol. 2017, 69, 2771–22282. [Google Scholar] [CrossRef] [PubMed]
- Didona, D.; Juratli, H.A.; Scarsella, L.; Eming, R.; Hertl, M. The polymorphous spectrum of dermatomyositis: Classic features, newly described skin lesions, and rare variants. Eur. J. Dermatol. 2020, 30, 229–242. [Google Scholar] [CrossRef] [PubMed]
- Wong, K.O. Dermatomyositis: A clinical investigation of twenty three cases in Hong Kong. Br. J. Dermatol. 1969, 81, 544–547. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, M.; Yamamoto, T. Wong-type dermatomyositis: A first report from Japan. J. Dermatol. 2017, 44, e336–e337. [Google Scholar] [CrossRef] [PubMed]
- Bax, C.E.; Grinnell, M.; Concha, J.S.S.; Werth, V.P. Wong-type dermatomyositis in an African American patient. Arthritis Rheumatol. 2020, 73, 630. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Russo, R.; Gasparini, G.; Cozzani, E.; Gravina, B.; Parodi, A. Paraneoplastic Wong-Type Dermatomyositis Associated with Gynecological Malignancy. Medicina 2022, 58, 484. https://doi.org/10.3390/medicina58040484
Russo R, Gasparini G, Cozzani E, Gravina B, Parodi A. Paraneoplastic Wong-Type Dermatomyositis Associated with Gynecological Malignancy. Medicina. 2022; 58(4):484. https://doi.org/10.3390/medicina58040484
Chicago/Turabian StyleRusso, Roberto, Giulia Gasparini, Emanuele Cozzani, Brunella Gravina, and Aurora Parodi. 2022. "Paraneoplastic Wong-Type Dermatomyositis Associated with Gynecological Malignancy" Medicina 58, no. 4: 484. https://doi.org/10.3390/medicina58040484
APA StyleRusso, R., Gasparini, G., Cozzani, E., Gravina, B., & Parodi, A. (2022). Paraneoplastic Wong-Type Dermatomyositis Associated with Gynecological Malignancy. Medicina, 58(4), 484. https://doi.org/10.3390/medicina58040484




