Dual Mobility Cups as the Routine Choice in Total Hip Arthroplasty
Abstract
1. Introduction
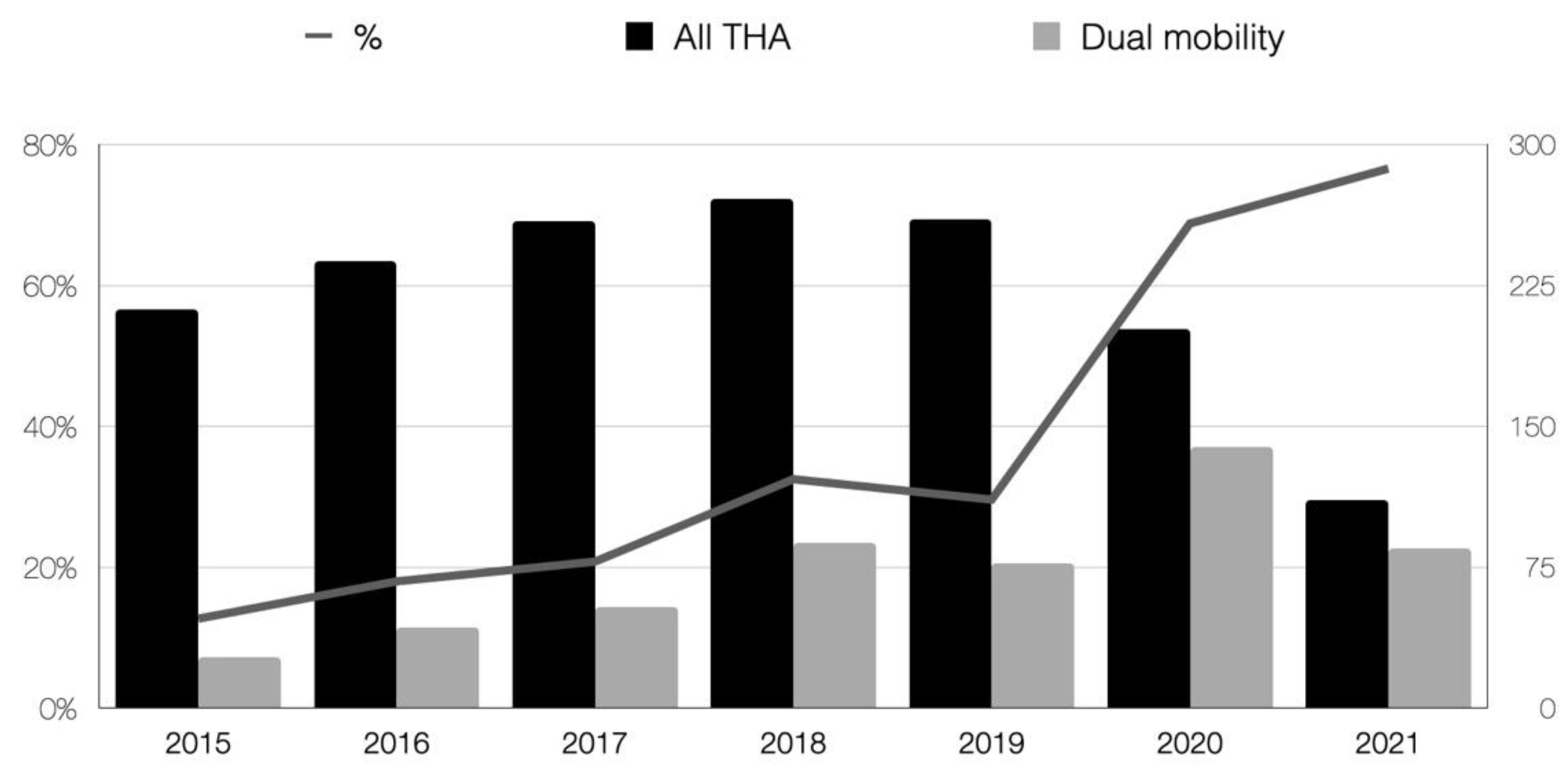
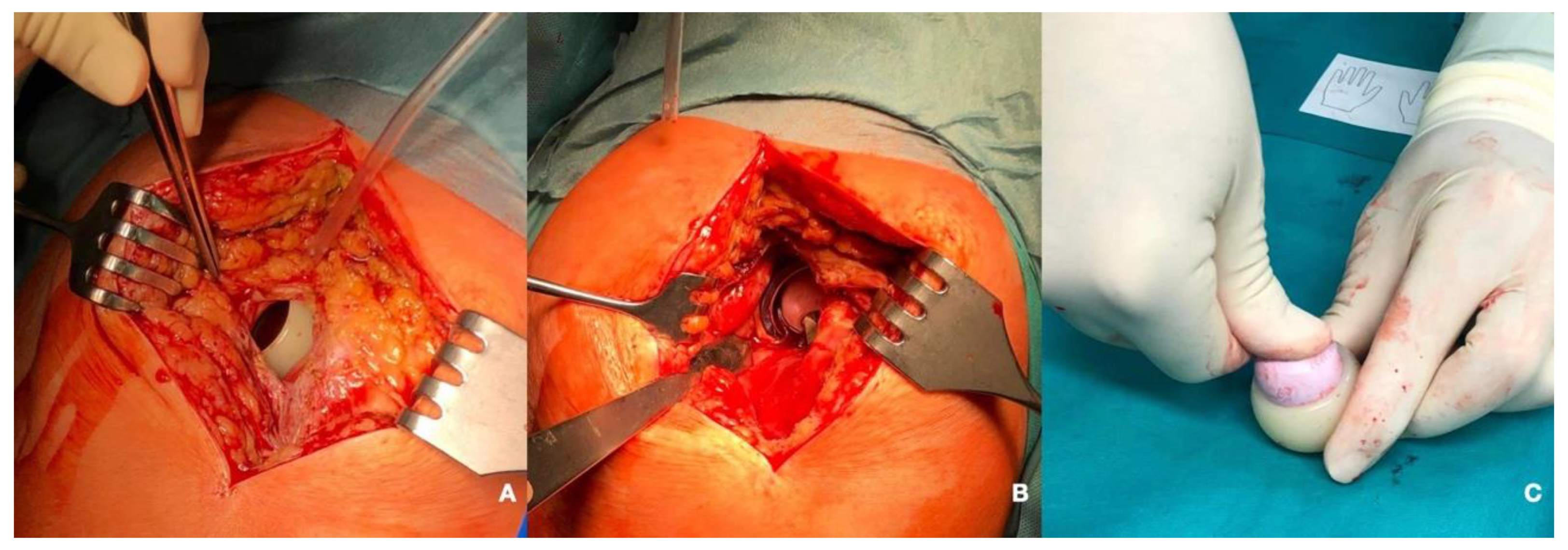
2. Materials and Methods
Statistical Analysis
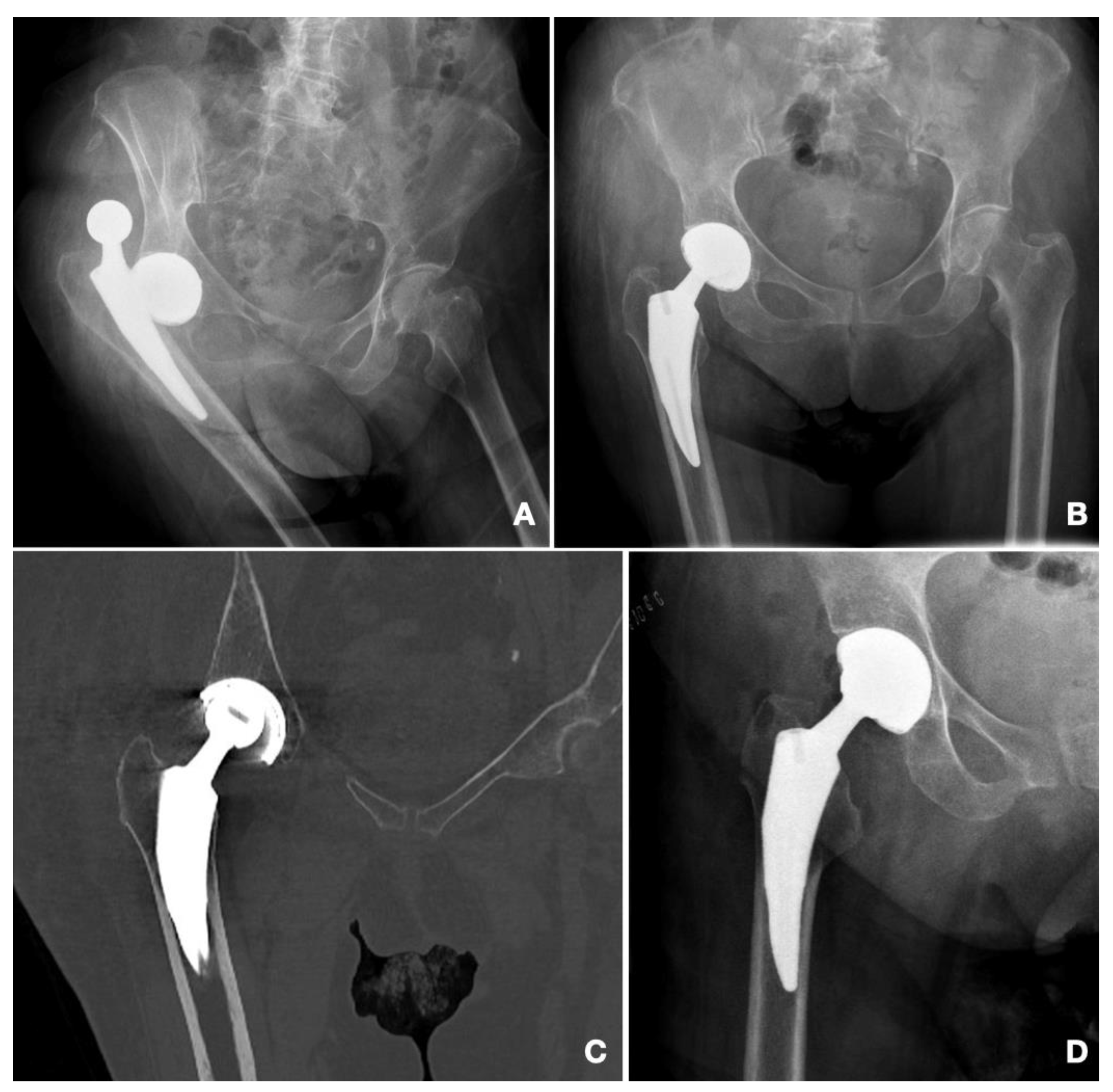
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- De Martino, I.; D’Apolito, R.; Soranoglou, V.G.; Poultsides, L.A.; Sculco, P.K.; Sculco, T.P. Dislocation Following Total Hip Arthroplasty Using Dual Mobility Acetabular Components: A Systematic Review. Bone Jt. J. 2017, 99-B, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Cuthbert, R.; Wong, J.; Mitchell, P.; Kumar Jaiswal, P. Dual Mobility in Primary Total Hip Arthroplasty: Current Concepts. EFORT Open Rev. 2019, 4, 640–646. [Google Scholar] [CrossRef] [PubMed]
- Hermena, S.; Tawfeek, W.; Latimer, P. Intraprosthetic Dislocation of Dual-Mobility Total Hip Arthroplasty: The Unforeseen Complication. Cureus 2021, 13, e19858. [Google Scholar] [CrossRef] [PubMed]
- Portal Estadístico. Registry of Activity in Specialized Health Care. RAE-CMBD. Madrid. Ministry of Health. Government of Spain. Available online: https://www.Sanidad.Gob.Es/EstadEstudios/Estadisticas/Cmbdhome.Htm (accessed on 10 January 2022).
- Blakeney, W.G.; Epinette, J.-A.; Vendittoli, P.-A. Dual Mobility Total Hip Arthroplasty: Should Everyone Get One? EFORT Open Rev. 2019, 4, 541–547. [Google Scholar] [CrossRef] [PubMed]
- Vajapey, S.P.; Fideler, K.L.; Lynch, D.; Li, M. Use of Dual Mobility Components in Total Hip Arthroplasty: Indications and Outcomes. J. Clin. Orthop. Trauma 2020, 11, S760–S765. [Google Scholar] [CrossRef] [PubMed]
- Kunutsor, S.K.; Barrett, M.C.; Beswick, A.D.; Judge, A.; Blom, A.W.; Wylde, V.; Whitehouse, M.R. Risk Factors for Dislocation after Primary Total Hip Replacement: A Systematic Review and Meta-Analysis of 125 Studies Involving Approximately Five Million Hip Replacements. Lancet Rheumatol. 2019, 1, e111–e121. [Google Scholar] [CrossRef]
- Dubin, J.A.; Westrich, G.H. Lack of Early Dislocation for Dual Mobility vs. Fixed Bearing Total Hip Arthroplasty: A Multi-Center Analysis of Comparable Cohorts. J. Orthop. 2020, 21, 1–5. [Google Scholar] [CrossRef]
- Darrith, B.; Courtney, P.M.; Della Valle, C.J. Outcomes of Dual Mobility Components in Total Hip Arthroplasty: A Systematic Review of the Literature. Bone Jt. J. 2018, 100-B, 11–19. [Google Scholar] [CrossRef]
- Assi, C.; Barakat, H.; Mansour, J.; Samaha, C.; Yammine, K. Primary Total Hip Arthroplasty: Mid-Term Outcomes of Dual-Mobility Cups in Patients at High Risk of Dislocation. HIP Int. 2021, 31, 174–180. [Google Scholar] [CrossRef]
- Pituckanotai, K.; Arirachakaran, A.; Tuchinda, H.; Putananon, C.; Nualsalee, N.; Setrkraising, K.; Kongtharvonskul, J. Risk of Revision and Dislocation in Single, Dual Mobility and Large Femoral Head Total Hip Arthroplasty: Systematic Review and Network Meta-Analysis. Eur. J. Orthop. Surg. Traumatol. 2018, 28, 445–455. [Google Scholar] [CrossRef]
- Mufarrih, S.H.; Qureshi, N.Q.; Masri, B.; Noordin, S. Outcomes of Total Hip Arthroplasty Using Dual-Mobility Cups for Femoral Neck Fractures: A Systematic Review and Meta-Analysis. HIP Int. 2021, 31, 12–23. [Google Scholar] [CrossRef] [PubMed]
- Young, J.R.; O’Connor, C.M.; Anoushiravani, A.A.; DiCaprio, M.R. The Use of Dual Mobility Implants in Patients Who Are at High Risk for Dislocation After Primary Total Hip Arthroplasty. JBJS Rev. 2020, 8, e20.00028. [Google Scholar] [CrossRef] [PubMed]
- Prudhon, J.-L.; Ferreira, A.; Verdier, R. Dual Mobility Cup: Dislocation Rate and Survivorship at Ten Years of Follow-Up. Int. Orthop. 2013, 37, 2345–2350. [Google Scholar] [CrossRef] [PubMed]
- Vielpeau, C.; Lebel, B.; Ardouin, L.; Burdin, G.; Lautridou, C. The Dual Mobility Socket Concept: Experience with 668 Cases. Int. Orthop. 2011, 35, 225–230. [Google Scholar] [CrossRef]
- Acker, A.; Fischer, J.-F.; Aminian, K.; Lécureux, E.; Jolles, B.M. Total Hip Arthroplasty Using a Cementless Dual-Mobility Cup Provides Increased Stability and Favorable Gait Parameters at Five Years Follow-Up. Orthop. Traumatol. Surg. Res. 2017, 103, 21–25. [Google Scholar] [CrossRef]
- Batailler, C.; Fary, C.; Verdier, R.; Aslanian, T.; Caton, J.; Lustig, S. The Evolution of Outcomes and Indications for the Dual-Mobility Cup: A Systematic Review. Int. Orthop. 2017, 41, 645–659. [Google Scholar] [CrossRef]
- Cha, Y.-H.; Yoo, J.-I.; Kim, J.-T.; Park, C.-H.; Ahn, Y.-S.; Choy, W.-S.; Ha, Y.-C.; Koo, K.-H. Dual Mobility Total Hip Arthroplasty in the Treatment of Femoral Neck Fractures. Bone Jt. J. 2020, 102, 10. [Google Scholar] [CrossRef]
- Cnudde, P.H.J.; Nåtman, J.; Hailer, N.P.; Rogmark, C. Total, Hemi, or Dual-Mobility Arthroplasty for the Treatment of Femoral Neck Fractures in Patients with Neurological Disease: Analysis of 9,638 Patients from the Swedish Hip Arthroplasty Register. Bone Jt. J. 2022, 104-B, 134–141. [Google Scholar] [CrossRef]
- Philippot, R.; Boyer, B.; Farizon, F. Intraprosthetic Dislocation: A Specific Complication of the Dual-Mobility System. Clin. Orthop. 2013, 471, 965–970. [Google Scholar] [CrossRef]
- Epinette, J.-A. Clinical Outcomes, Survivorship and Adverse Events with Mobile-Bearings versus Fixed-Bearings in Hip Arthroplasty-a Prospective Comparative Cohort Study of 143 ADM versus 130 Trident Cups at 2 to 6-Year Follow-Up. J. Arthroplast. 2015, 30, 241–248. [Google Scholar] [CrossRef]
- Vigdorchik, J.M.; D’Apuzzo, M.R.; Markel, D.C.; Malkani, A.L.; Raterman, S.; Sharpe, K.P.; Cornell, C.N.; Westrich, G.H. Lack of Early Dislocation Following Total Hip Arthroplasty with a New Dual Mobility Acetabular Design. Hip Int. J. Clin. Exp. Res. Hip Pathol. Ther. 2015, 25, 34–38. [Google Scholar] [CrossRef] [PubMed]
- Raphael, B.S.; Dines, J.S.; Akerman, M.; Root, L. Long-Term Followup of Total Hip Arthroplasty in Patients with Cerebral Palsy. Clin. Orthop. 2010, 468, 1845–1854. [Google Scholar] [CrossRef] [PubMed]
- Tarasevicius, S.; Robertsson, O.; Dobozinskas, P.; Wingstrand, H. A Comparison of Outcomes and Dislocation Rates Using Dual Articulation Cups and THA for Intracapsular Femoral Neck Fractures. Hip Int. J. Clin. Exp. Res. Hip Pathol. Ther. 2013, 23, 22–26. [Google Scholar] [CrossRef] [PubMed]
- Barlow, B.T.; McLawhorn, A.S.; Westrich, G.H. The Cost-Effectiveness of Dual Mobility Implants for Primary Total Hip Arthroplasty: A Computer-Based Cost-Utility Model. J. Bone Jt. Surg. 2017, 99, 768–777. [Google Scholar] [CrossRef] [PubMed]
- Epinette, J.-A.; Lafuma, A.; Robert, J.; Doz, M. Cost-Effectiveness Model Comparing Dual-Mobility to Fixed-Bearing Designs for Total Hip Replacement in France. Orthop. Traumatol. Surg. Res. OTSR 2016, 102, 143–148. [Google Scholar] [CrossRef]
- Enocson, A.; Hedbeck, C.-J.; Tidermark, J.; Pettersson, H.; Ponzer, S.; Lapidus, L.J. Dislocation of Total Hip Replacement in Patients with Fractures of the Femoral Neck. Acta Orthop. 2009, 80, 184–189. [Google Scholar] [CrossRef]
- Matharu, G.S.; Judge, A.; Deere, K.; Blom, A.W.; Reed, M.R.; Whitehouse, M.R. The Effect of Surgical Approach on Outcomes Following Total Hip Arthroplasty Performed for Displaced Intracapsular Hip Fractures: An Analysis from the National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. J. Bone Jt. Surg. Am. 2020, 102, 21–28. [Google Scholar] [CrossRef]
- Tsikandylakis, G.; Mohaddes, M.; Cnudde, P.; Eskelinen, A.; Kärrholm, J.; Rolfson, O. Head Size in Primary Total Hip Arthroplasty. EFORT Open Rev. 2018, 3, 225–231. [Google Scholar] [CrossRef]
- Cebatorius, A.; Robertsson, O.; Stucinskas, J.; Smailys, A.; Leonas, L.; Tarasevicius, S. Choice of Approach, but Not Femoral Head Size, Affects Revision Rate Due to Dislocations in THA after Femoral Neck Fracture: Results from the Lithuanian Arthroplasty Register. Int. Orthop. 2015, 39, 1073–1076. [Google Scholar] [CrossRef]
- Tigani, D.; Prudhon, J.L.; Amendola, L.; Aslanian, T. Letter to the Editor on “Early Intraprosthetic Dislocation in Dual-Mobility Implants: A Systematic Review. Arthroplast. Today 2018, 4, 132. [Google Scholar] [CrossRef]
- Aslanian, T. All Dual Mobility Cups Are Not the Same. Int. Orthop. 2017, 41, 573–581. [Google Scholar] [CrossRef] [PubMed]
- Nevelos, J.; Johnson, A.; Heffernan, C.; Macintyre, J.; Markel, D.C.; Mont, M.A. What Factors Affect Posterior Dislocation Distance in THA? Clin. Orthop. 2013, 471, 519–526. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Heffernan, C.; Banerjee, S.; Nevelos, J.; Macintyre, J.; Issa, K.; Markel, D.C.; Mont, M.A. Does Dual-Mobility Cup Geometry Affect Posterior Horizontal Dislocation Distance? Clin. Orthop. 2014, 472, 1535–1544. [Google Scholar] [CrossRef] [PubMed]
| ID | Cup | Time after Index Surgery | Mechanism | Reduction | Redislocation | Remarks | Need for Revision | Functional Status (Parker) |
|---|---|---|---|---|---|---|---|---|
| 1 | G7 | 5 | Atraumatic | Closed | - | No | Walks with one simple aid | |
| 2 | G7 | 45 | Atraumatic | Closed | 26 days after | Death < 1 year | No | Walks with walking frame |
| 3 | G7 | 1 | Atraumatic | Open | 4 days after | Death < 1 year | 1st episode: Stem and Cup revision 2nd episode: Girdlestone | No walking |
| 4 | Apogee | 13 | Traumatic | Open | No walking | |||
| 5 | G7 | 6 | Atraumatic | Closed | 1 day after 9 days after | 2nd episode: Cup revision 3rd episode: Cup revision | No walking | |
| 6 | G7 | 72 | Atraumatic | Closed | Walks with one simple aid | |||
| 7 | G7 | 376 | Traumatic | Open | Intraprosthetic dislocation | Revision of dual mobility head | Walks with walking frame | |
| 8 | G7 | 23 | Atraumatic | Open | Dislocation associated with Vancouver B2 fracture | Revision of stem | Walks with one simple aid |
| Group A (Non Dislocated) n = 523 | Group B (Dislocated) n = 8 | p Value | |
|---|---|---|---|
| Age (years) | 72.0 (SD: 11.7) | 78.49 (SD: 5.96) | 0.122 |
| Sex (%) | Male: 197 (37.6%) Female: 326 (62.4%) | Male: 2 (0.25%) Female: 6 (0.75%) | 0.716 |
| Side | Left: 261 (49.9%) Right: 262 (51.1%) | Left: 4 (50%) Right: 4 (50%) | 1 |
| Indication | NOF#: 247 (47.2%) HOA: 276 (52.8%) | NOF#: 8 (100%) HOA: 0 | 0.003 |
| Head size (mm) | 28 mm: 515 (98.5%) 22 mm: 8 (1.5%) | 28 mm: 6 (75%) 22 mm: 2 (25%) | 0.008 |
| Cup size (mm) | 51.2 (SD: 3.34) | 48.7 (SD: 2.81) | 0.038 |
| Cup inclination (°) | 44.8 (SD: 7.86) | 41.9 (SD: 6.83) | 0.299 |
| Surgical time (min) | 73.8 (SD: 23.72) | 75 (SD: 13.09) | 0.890 |
| Approach | WJ: 421 (80.5%) PL: 102 (19.5%) | WJ: 3 (37.5%) PL: 5 (62.5%) | 0.011 |
| Length of stay (days) | 7.1 (SD: 3.43) | 11.7 (SD: 7.74) | <0.0001 |
| Mortality (1 year) | 25 (4.7%) | 2 (25%) | 0.06 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aguado-Maestro, I.; de Blas-Sanz, I.; Sanz-Peñas, A.E.; Campesino-Nieto, S.V.; Diez-Rodríguez, J.; Valle-López, S.; Espinel-Riol, A.; Fernández-Díez, D.; García-Alonso, M. Dual Mobility Cups as the Routine Choice in Total Hip Arthroplasty. Medicina 2022, 58, 528. https://doi.org/10.3390/medicina58040528
Aguado-Maestro I, de Blas-Sanz I, Sanz-Peñas AE, Campesino-Nieto SV, Diez-Rodríguez J, Valle-López S, Espinel-Riol A, Fernández-Díez D, García-Alonso M. Dual Mobility Cups as the Routine Choice in Total Hip Arthroplasty. Medicina. 2022; 58(4):528. https://doi.org/10.3390/medicina58040528
Chicago/Turabian StyleAguado-Maestro, Ignacio, Inés de Blas-Sanz, Ana Elena Sanz-Peñas, Silvia Virginia Campesino-Nieto, Jesús Diez-Rodríguez, Sergio Valle-López, Alberto Espinel-Riol, Diego Fernández-Díez, and Manuel García-Alonso. 2022. "Dual Mobility Cups as the Routine Choice in Total Hip Arthroplasty" Medicina 58, no. 4: 528. https://doi.org/10.3390/medicina58040528
APA StyleAguado-Maestro, I., de Blas-Sanz, I., Sanz-Peñas, A. E., Campesino-Nieto, S. V., Diez-Rodríguez, J., Valle-López, S., Espinel-Riol, A., Fernández-Díez, D., & García-Alonso, M. (2022). Dual Mobility Cups as the Routine Choice in Total Hip Arthroplasty. Medicina, 58(4), 528. https://doi.org/10.3390/medicina58040528






