Abstract
In percutaneous pedicle screw (PPS) fixation of the osteoporotic spine, rigid screw fixation obtaining strong stabilization is important for achieving successful treatment outcomes. However, in patients with severe osteoporosis, it is difficult to obtain PPS fixation with sufficient stability. PPS fixation has potential disadvantages with respect to maintaining secure stabilization in comparison to conventional pedicle screw fixation. In PPS fixation, bone grafting to achieve posterior spine fusion is generally not applicable and transverse connectors between the rods cannot be used to reinforce the fixation. Various augmentation methods, including additional hooks, sublaminar bands, and hydroxyapatite (HA) sticks, are available for conventional pedicle screw fixation. On the other hand, there has been no established augmentation method for PPS fixation. Recently, we developed a novel augmentation technique for PPS fixation using HA granules. This technique allows the percutaneous insertion of HA granules into the screw hole along the guidewire prior to insertion of the PPS. We have used this augmentation technique for PPS fixation in various spine surgeries in patients with osteoporosis. In our previous studies, biomechanical analyses demonstrated that PPS fixation was significantly enhanced by augmentation with HA granules in the osteoporotic lumbar spine. Furthermore, augmentation with HA granules was considered to decrease the incidence of screw loosening and implant failure following PPS fixation in patients with osteoporotic spine. In this article, we describe the surgical procedures of the augmentation method using HA granules and summarize our data from the biomechanical analysis of augmentation for PPS fixation. We also review the surgical outcomes of PPS fixation with augmentation using HA granules.
1. Introduction
In the last decade, percutaneous pedicle screw (PPS) fixation has been widely used for minimally invasive spinal surgery. PPS fixation has been performed for various surgeries to treat spinal trauma, tumors, infection, deformity, and degenerative diseases in the thoraco-lumbar spine [1]. PPS fixation can reduce the damage of the surrounding tissues, intraoperative blood loss, postoperative pain, and recovery time in comparison to conventional pedicle screw fixation [2,3,4].
Osteoporosis is becoming more common as the population ages [5,6]. In pedicle screw fixation for osteoporotic spine, rigid screw fixation and strong stabilization are essential for achieving successful treatment outcomes. However, in osteoporotic patients, it is difficult to obtain screw fixation with sufficient stability due to bone fragility. Therefore, there are certain risk factors for screw loosening and implant failure after surgery with instrumentation for osteoporotic spine [7,8]. Various augmentation methods have been used for conventional pedicle screw fixation in spine surgery for patients with osteoporosis, including additional hooks [9,10,11], sublaminar bands [12,13], cement augmentation [14,15], and hydroxyapatite (HA) sticks [16,17].
PPS fixation has potential disadvantages with respect to maintaining strong stabilization in comparison to conventional pedicle screw fixation. In PPS fixation, bone grafting to achieve posterior spine fusion is generally not applicable [18,19]. Because of the percutaneous technique involving a small incision, transverse connectors between the rods cannot be used to reinforce the PPS fixation [20,21]. Conventional augmentation methods, including additional hooks and sublaminar bands, are not applicable in PPS fixation. However, there has been no standardized augmentation method for PPS fixation.
Recently, we developed a novel augmentation technique for PPS fixation using hydroxyapatite (HA) granules [22]. This technique allows for the percutaneous insertion of HA granules into the screw hole along the guidewire prior to insertion of the PPS [22,23]. We have used this augmentation technique for PPS fixation in various spine surgeries [23,24]. The biomechanical analyses of our previous studies demonstrated that PPS fixation was significantly enhanced by augmentation with HA granules in the osteoporotic lumbar spine [22,23]. Furthermore, augmentation with HA granules was considered to reduce the incidence of screw loosening and implant failure following PPS fixation in patients with osteoporotic spine [22,24,25].
In this article, we describe the surgical procedures of the augmentation method using HA granules and summarize the data obtained from the biomechanical analysis of augmentation for PPS fixation. We also review the surgical outcomes of PPS fixation with augmentation using HA granules.
2. Surgical Procedure of Augmentation of PPS Fixation Using HA Granules
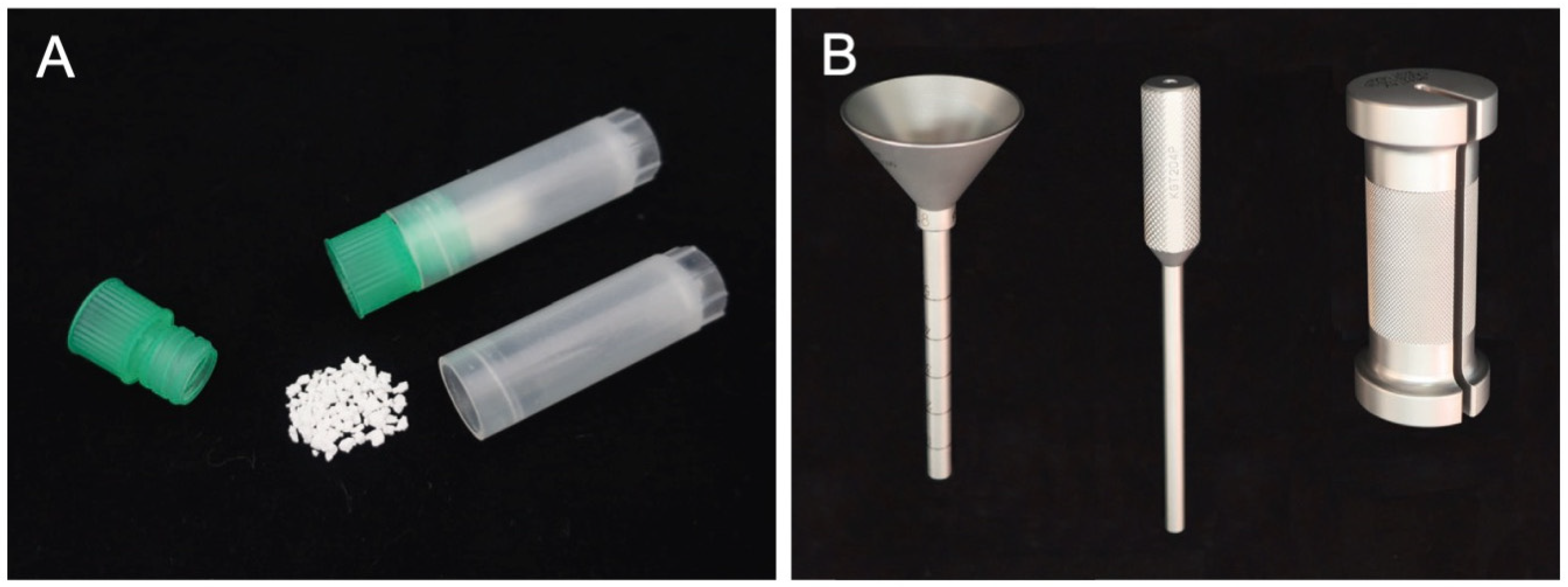
In our augmentation technique for PPS fixation, HA granules can be inserted percutaneously into the screw hole along the guidewire using a dedicated inserter (Figure 1). This method has the advantage that PPS fixation can be enhanced percutaneously without compromising the minimally invasive procedure. We use commercially available HA granules (porosity, 50%; particle size, 1.0–2.0 mm; Apaceram, HOYA Technosurgical Corp., Tokyo, Japan) for the augmentation (Figure 1A) [22,23]. Based on the results of biomechanical analyses in our previous studies [22,23], at least 0.25 g of HA granules are used for the augmentation for each PPS. We created a dedicated device to insert the HA granules percutaneously into the screw hole in order to achieve the augmentation (Figure 1B) [14].
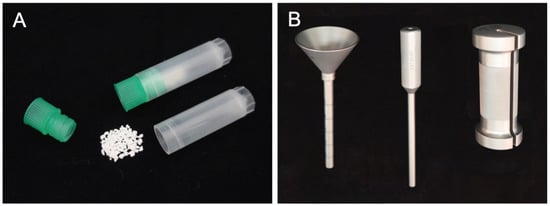
Figure 1.
HA granules and the dedicated inserter for augmentation of PPS fixation. HA granules (porosity, 50%; particle size, 1–2 mm) are used for augmentation (A). The inserter consists of a funnel-shaped external cylinder, internal cylinder, and slide hammer (B).
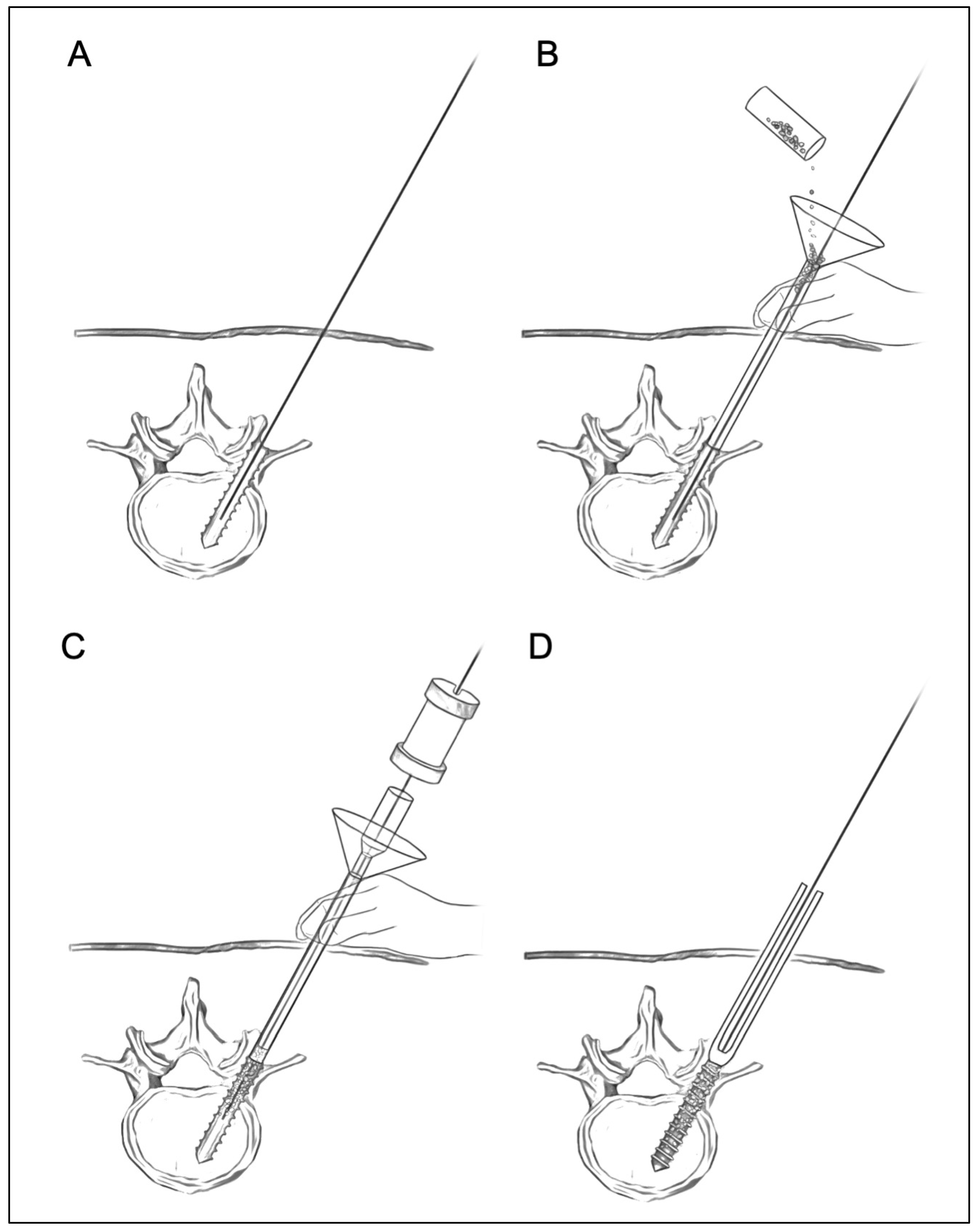
The surgical procedures for the augmentation of PPS fixation are as follows (Figure 2). First, according to the standard method of PPS insertion, the guidewire is inserted into the pedicle and posterior part of the vertebral body using a Jamshidi needle under fluoroscopic guidance. Then, the screw hole is prepared using a cannulated tap along the guidewire (Figure 2A). Secondly, the funnel-shaped external cylinder of the insertion device is placed at the screw hole along the guidewire (Figure 2B). Then, HA granules are inserted into the external cylinder. The tip of the inserter was set at the entry point of the screw hole so that the HA granules were mainly placed within the pedicle but not the vertebral body. Using the internal cylinder and slide hammer, the HA granules are pushed into the screw hole (Figure 2C). The position of the tip of the guidewire must be carefully checked on a lateral fluoroscopic image in order to prevent the guidewire from penetrating the anterior wall of the vertebral body (Figure 3). In addition, an assistant should securely grasp the proximal part of the guidewire with a Kocher forceps to prevent the guidewire from moving forward (Figure 3). After removing the insertion device, the PPS can be inserted into the screw hole along the guidewire (Figure 2D).
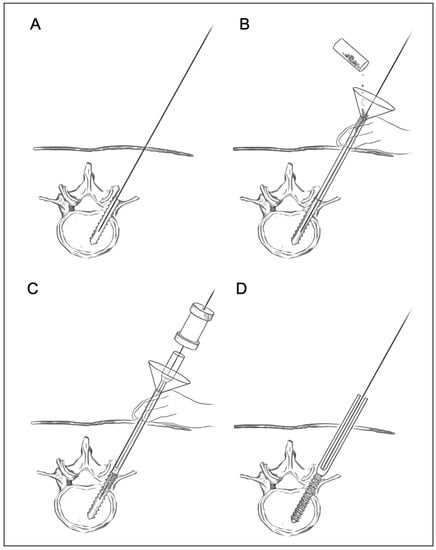
Figure 2.
Surgical procedures for augmentation of PPS fixation using HA granules. A guidewire is inserted into the vertebra, and then tapping is performed (A). The funnel-shaped external cylinder is placed at the screw hole along the guidewire. HA granules are put into the external cylinder (B). Then, the HA granules are pushed into the screw hole using the internal cylinder and slide hammer (C). Finally, screw insertion is performed (D).
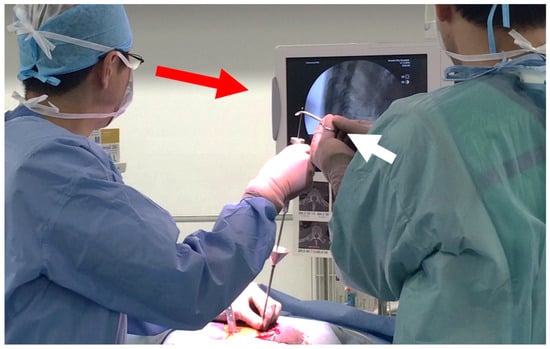
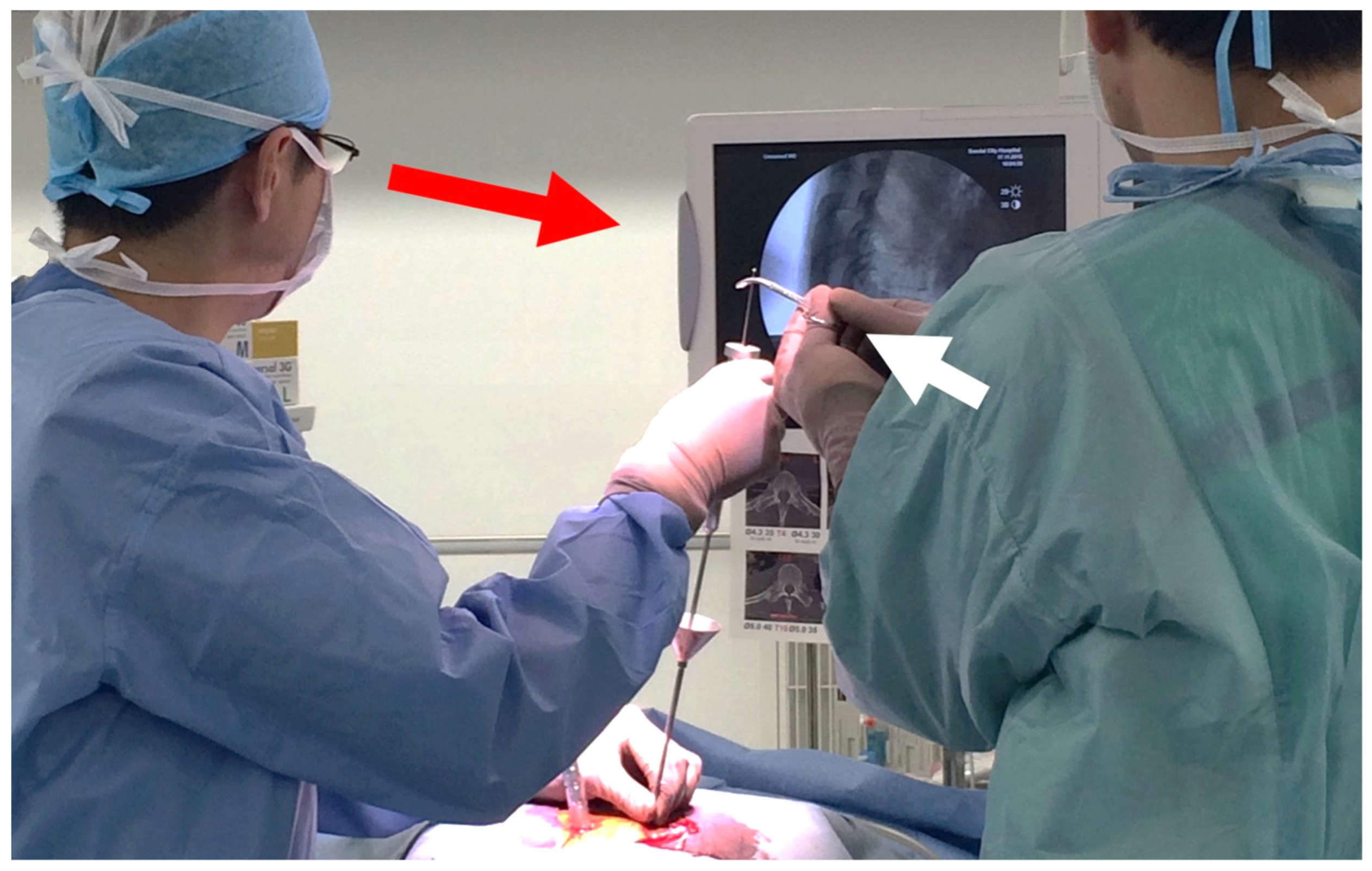
Figure 3.
HA granules are pushed into the screw hole using the internal cylinder and slide hammer. The position of the tip of the guidewire must be carefully checked on a lateral fluoroscopic image in order to prevent the guidewire from penetrating the anterior wall of the vertebral body (red arrow). In addition, an assistant should grasp securely the proximal part of the guidewire with a Kocher forceps to prevent the guidewire from moving forward (white arrow).
3. Biomechanical Analysis of Augmentation of PPS Fixation Using HA Granules
Previous studies indicated that the placement of substances into the tapped screw hole increases the bone–metal interface friction force and enhances the mechanical strength of screw fixation [16,26,27,28,29,30,31]. We previously performed a biomechanical analysis to evaluate the strength and stiffness of PPS fixation augmented with HA granules using a synthetic bone model [22]. The results of that study demonstrated the biomechanical advantages of augmentation with HA granules for PPS fixation in the osteoporotic bone model. The study showed that the maximal insertion torque and the maximal pullout strength were significantly increased in screws with augmentation in comparison to without augmentation. Furthermore, the mechanical strength against cyclic loading was significantly greater in screws with augmentation in comparison to those without augmentation.
In another study, we performed a cadaveric biomechanical analysis of PPS fixation augmented with HA granules [23]. The biomechanical performance in augmenting PPS fixation was evaluated using osteoporotic lumbar vertebrae obtained from cadavers. Our results demonstrated that the augmentation using HA granules significantly increased the maximal pullout strength and maximal insertion torque of the screws placed in the osteoporotic lumbar spine. Moreover, a cyclic loading test revealed that the augmented screws achieved significantly higher mechanical strength.
These findings suggest that PPS fixation can be enhanced by augmentation with HA granules in the osteoporotic lumbar spine. PPS fixation augmented with HA granules may be helpful for decreasing the incidence of screw loosening and implant failure in patients with osteoporotic spine.
4. Postoperative Stability of PPS Fixation in Osteoporotic Patients
To determine whether augmentation with HA granules can improve the postoperative stability of PPS fixation in osteoporotic patients, we previously evaluated the incidence of screw loosening and implant failure after surgery [25]. In this study, we analyzed 32 patients with osteoporotic spine (male, n = 18; female, n = 14; age, 74 ± 11 years) who underwent PPS fixation with augmentation using HA granules at multiple levels (5.9 ± 1.9 levels). Postoperative screw loosening was assessed by radiographic images and the presence of a clear zone around the screw on X-ray and computed tomography (CT) [32,33]. The presence or absence of reoperation due to postoperative implant failure was also investigated. In our results, screw loosening was observed in 21 of 360 screws (5.8%) and 8 of 32 patients at the final follow-up examination (15 ± 9.8 months). Importantly, there were no cases of reoperation due to implant failure. No patients had cardiovascular or neurological complications associated with augmentation with HA granules.
Ohtori et al. showed that 26 of 102 (25.5%) conventional pedicle screws implanted in patients with osteoporotic spine became loose at the 12-month follow-up examination [33]. In addition, Ohba et al. reported that screw loosening was found in 44 of 290 screws (15.2%) at 1 year after PPS fixation [32]. In the results of our study, the incidence of screw loosening (5.8%) was lower than that in previous reports. Thus, augmentation with HA granules may improve the stability of PPS fixation and consequently decrease the incidence of postoperative screw loosening and implant failure.
5. Illustrative Case
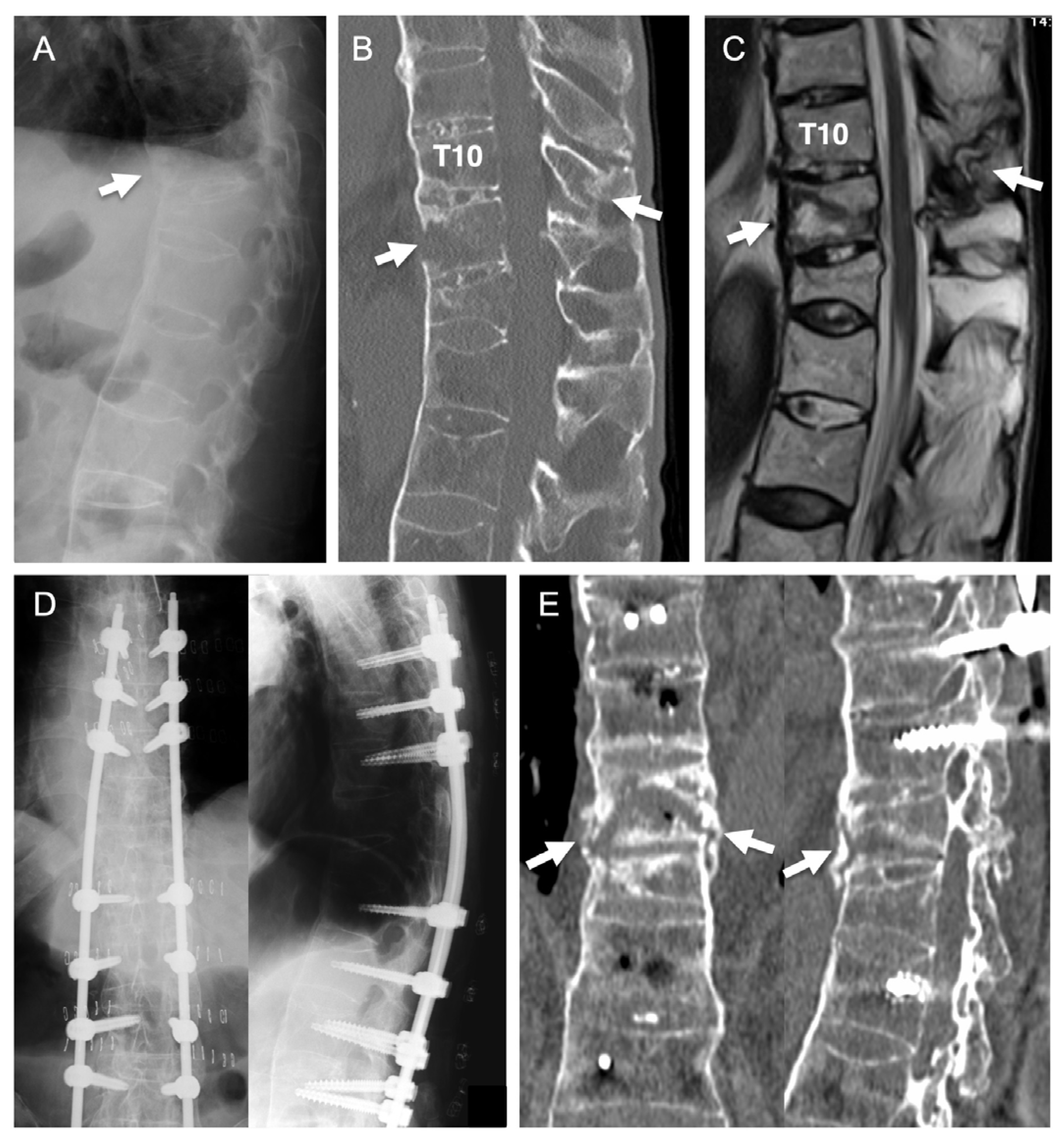
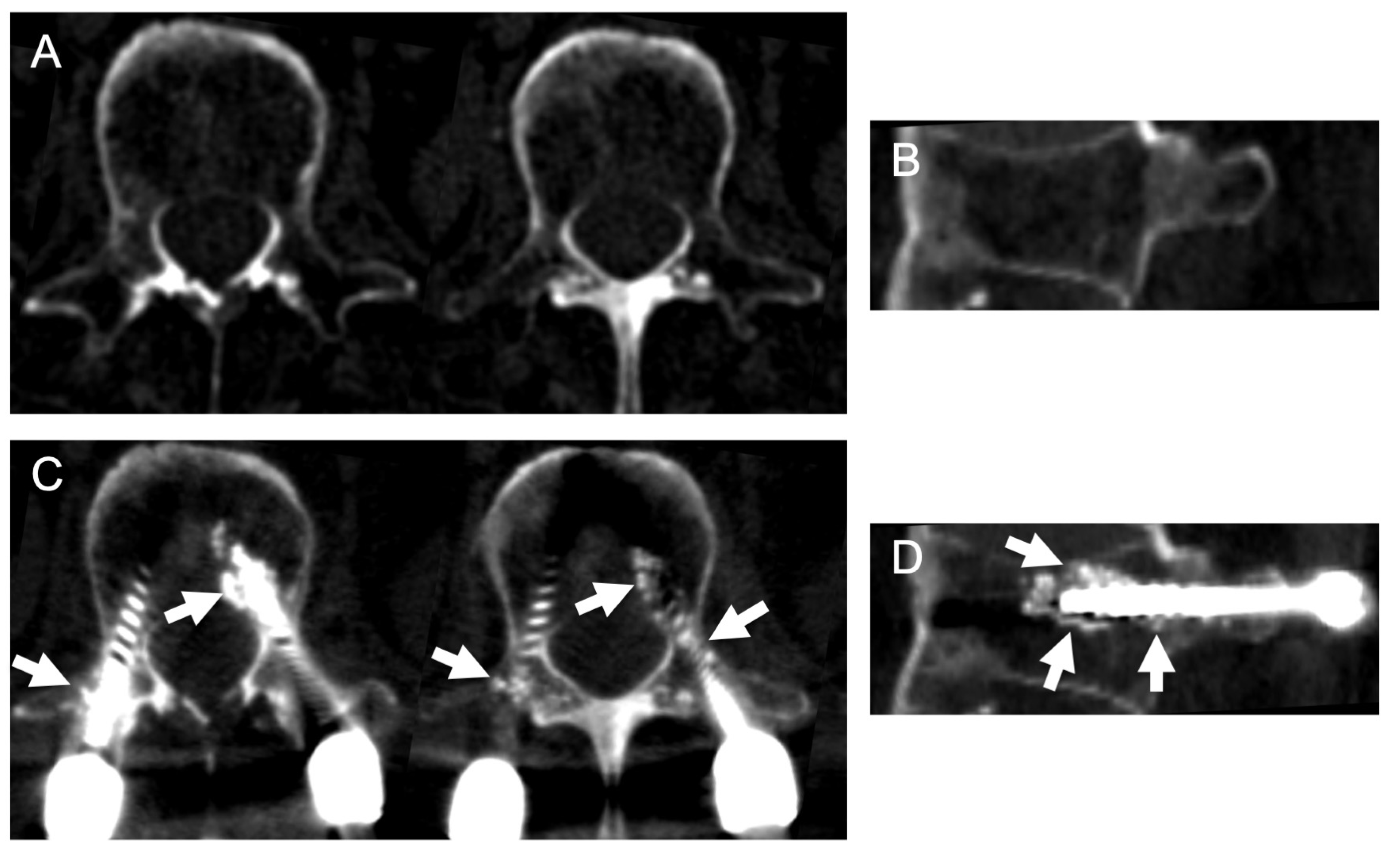
The patient was an 81-year-old man with ankylosing spondylitis and severe osteoporosis. He fell from a stepladder and sustained a thoracic spinal fracture. He had been hospitalized for one month at another hospital. However, his severe back pain did not improve and he was confined to bed. He was then referred to our department for further treatment. An imaging study at our hospital revealed spinal ankylosis and spinal fracture at the T10–11 level (Figure 4A–C). The patient underwent surgery to perform PPS fixation with augmentation using HA granules (Figure 4D). After the operation, his symptoms disappeared and he became able to walk without any support. Postoperative CT revealed HA granules surrounding the screws within the pedicle and vertebral body (Figure 5). Bone union at the fracture site was achieved at 12 months after surgery (Figure 4E). There was no implant failure or screw loosening in the postoperative course.
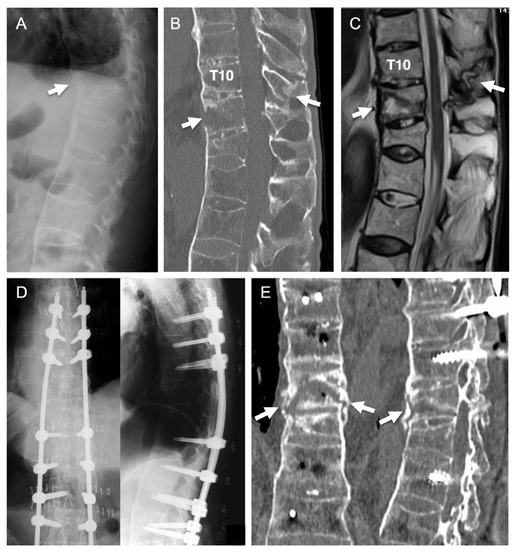
Figure 4.
Illustrative case. Preoperative images showed spinal ankylosis and spinal fracture at the T10–11 levels (arrows in (A–C)). PPS fixation with augmentation using HA granules was performed (D). Bone union at the fracture site was achieved at 12 months after surgery (arrows in (E)).
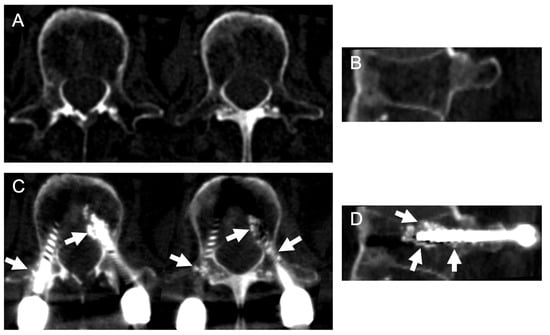
Figure 5.
Computed tomography before (A,B) and after (C,D) surgery. Postoperative axial (C) and sagittal (D) images revealed that the HA granules surrounded the screws within the pedicle and vertebral body (Arrows).
6. Discussion
Spinal surgery with instrumentation in patients with osteoporotic spine is challenging because of their bone fragility [34]. When pedicle screw fixation is performed in patients with osteoporosis, the incidence of loosening or screw back-out is higher [7,8]. Therefore, rigid screw fixation and secure stabilization of the spine are crucial for preventing postoperative implant failure. However, conventional augmentation methods, such as supplemental hooks and sublaminar bands, are normally not applicable to PPS fixation due to the percutaneous surgical procedure [18,19]. In PPS fixation, it is very difficult to insert biomaterials, such as HA sticks and bone cement, into the tapped pedicle because surgeons cannot see the screw hole directly and because a guidewire is placed within the pedicle percutaneously. Importantly, the use of an insertor for HA granules enables PPS augmentation to be achieved percutaneously in a minimally invasive procedure without additional skin incision [22,23]. The data of the biomechanical analysis demonstrated that PPS fixation with augmentation using HA granules produced significantly stronger screw pullout strength and insertion torque [22,23]. In addition, the reinforcement of the screws with HA granules significantly enhanced the resistance to cyclic loads. Furthermore, augmentation with HA granules decreased the incidence of screw loosening in osteoporotic patients after PPS fixation [24,25]. Augmentation using HA granules can be a practical method for minimally invasive spinal surgery with PPS fixation in patients with osteoporosis.
The reinforcement of pedicle screws using polymethylmethacrylate (PMMA) can increase the fixation strength of spinal instrumentation in the osteoporotic spine [15]. A previous study indicated that pedicle screws augmented by PMMA cement showed significantly stronger pullout strength in comparison to non-augmented screws [35]. However, the augmentation method using PMMA cement has several unfavorable issues. PMMA is unable to induce bone remodeling, osteoinduction, osteoconduction, or osteointegration and its presence can inhibit the vascular supply. PMMA cement has exothermic properties that may induce bone necrosis and degeneration of the adjacent discs [36,37]. Furthermore, augmentation with PMMA cement causes a risk of vertebral fracture that can induce nerve root or dural injury during screw removal [38]. In contrast, HA has high bioaffinity and biocompatibility, which induces osteoconduction and osteointegration [39]. HA can be slowly replaced by the host bone [39]. HA induces no exothermic reaction or toxic effects that could damage the surrounding bone or soft tissue following implantation.
Cement-based augmentation is associated with a risk of cement extravasation, which may cause cardiovascular complications [36]. The insertion of PMMA cement into the vertebral body has been widely recognized as a possible cause of pulmonary cement embolism and fat embolism syndrome [40,41,42,43]. Many previous reports have indicated that percutaneous vertebroplasty and balloon kyphoplasty using PMMA is associated with a certain risk of embolic events [44,45]. Indeed, it has been reported that augmentation of pedicle screws with PMMA cement caused severe fat embolism syndrome [46]. Over the past few decades, the augmentation of pedicle screws using HA granules has been widely used in spinal surgeries in various countries [16,17,22,47]. In addition, vertebroplasty with transpedicular HA block grafting has long been performed for the treatment of thoracolumbar vertebral fracture [48,49,50]. However, to our knowledge, there have been no previous reports of symptomatic or asymptomatic pulmonary embolism associated with the augmentation of pedicle screws using HA granules. Only one study reported a case of asymptomatic pulmonary embolism after vertebroplasty with HA ceramic blocks [51]. It has been suggested that the insertion of solid material into the vertebral body may be safer than injecting liquid material with respect to the risk of extravertebral leakage causing embolism [40,51]. Therefore, the insertion of HA granules into the vertebral body may be associated with a lower risk of embolic events in comparison to the injection of PMMA cement [52]. Although the potential risk of an embolic event during spinal surgery should not be ignored, HA granules are considered safer than PMMA cement for the augmentation of PPS fixation.
7. Conclusions
The rigidity and stability of PPS fixation can be enhanced by augmentation with HA granules in the osteoporotic spine. Augmentation with HA granules may help to reduce the incidence of screw loosening and implant failure following PPS fixation. Augmentation using HA granules can be a practical method for minimally invasive spinal surgery with PPS fixation in patients with osteoporosis.
Author Contributions
Conceptualization, H.K.; writing—original draft, H.K.; writing—review and editing, H.K.; visualization, H.K.; investigation, H.K., Y.O., K.H.; data curation, H.K., Y.O., K.H.; supervision, T.A., H.O. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Mobbs, R.J.; Park, A.; Maharaj, M.; Phan, K. Outcomes of percutaneous pedicle screw fixation for spinal trauma and tumours. J. Clin. Neurosci. 2016, 23, 88–94. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Li, H.; Zhou, Y.; Wang, J.; Chu, T.; Zheng, W.; Chen, B.; Li, C. Minimally Invasive Posterior Decompression Combined with Percutaneous Pedicle Screw Fixation for the Treatment of Thoracolumbar Fractures with Neurological Deficits. Spine 2016, 41, B23–B29. [Google Scholar] [CrossRef] [PubMed]
- Regev, G.J.; Lee, Y.P.; Taylor, W.R.; Garfin, S.R.; Kim, C.W. Nerve injury to the posterior rami medial branch during the insertion of pedicle screws: Comparison of mini-open versus percutaneous pedicle screw insertion techniques. Spine 2009, 34, 1239–1242. [Google Scholar] [CrossRef] [PubMed]
- Gu, G.; Zhang, H.; He, S.; Cai, X.; Gu, X.; Jia, J.; Fu, Q.; Zhou, X. Percutaneous Pedicle Screw Placement in the Lumbar Spine: A Comparison Study between the Novel Guidance System and the Conventional Fluoroscopy Method. J. Spinal Disord. Tech. 2015, 28, E522–E527. [Google Scholar] [CrossRef] [PubMed]
- Burge, R.; Dawson-Hughes, B.; Solomon, D.H.; Wong, J.B.; King, A.; Tosteson, A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J. Bone Miner Res. 2007, 22, 465–475. [Google Scholar] [CrossRef] [PubMed]
- Melton, L.J. Epidemiology of spinal osteoporosis. Spine 1997, 22, 2S–11S. [Google Scholar] [CrossRef]
- Okuyama, K.; Abe, E.; Suzuki, T.; Tamura, Y.; Chiba, M.; Sato, K. Can insertional torque predict screw loosening and related failures? An in vivo study of pedicle screw fixation augmenting posterior lumbar interbody fusion. Spine 2000, 25, 858–864. [Google Scholar] [CrossRef]
- Okuyama, K.; Abe, E.; Suzuki, T.; Tamura, Y.; Chiba, M.; Sato, K. Influence of bone mineral density on pedicle screw fixation: A study of pedicle screw fixation augmenting posterior lumbar interbody fusion in elderly patients. Spine J. 2001, 1, 402–407. [Google Scholar] [CrossRef]
- Murakami, H.; Tsai, K.-J.; Attallah-Wasif, E.S.; Yamazaki, K.; Shimamura, T.; Hutton, W.C. A biomechanical assessment of infra-laminar hooks as an alternative to supra-laminar hooks in thoracolumbar fixation. Spine 2006, 31, 967–971. [Google Scholar] [CrossRef]
- Hongo, M.; Gay, R.E.; Zhao, K.D.; Ilharreborde, B.; Huddleston, P.M.; Berglund, L.J.; An, K.-N.; Zhao, C. Junction kinematics between proximal mobile and distal fused lumbar segments: Biomechanical analysis of pedicle and hook constructs. Spine J. 2009, 9, 846–853. [Google Scholar] [CrossRef]
- Hasegawa, K.; Takahashi, H.E.; Uchiyama, S.; Hirano, T.; Hara, T.; Washio, T.; Sugiura, T.; Youkaichiya, M.; Ikeda, M. An experimental study of a combination method using a pedicle screw and laminar hook for the osteoporotic spine. Spine 1997, 22, 958–963. [Google Scholar] [CrossRef] [PubMed]
- Hamasaki, T.; Tanaka, N.; Kim, J.; Okada, M.; Ochi, M.; Hutton, W.C. Pedicle screw augmentation with polyethylene tape: A biomechanical study in the osteoporotic thoracolumbar spine. J. Spinal Disord. Tech. 2010, 23, 127–132. [Google Scholar] [CrossRef] [PubMed]
- Hongo, M.; Ilharreborde, B.; Gay, R.E.; Zhao, C.; Zhao, K.D.; Berglund, L.J.; Zobitz, M.; An, K.-N. Biomechanical evaluation of a new fixation device for the thoracic spine. Eur. Spine J. 2009, 18, 1213–1219. [Google Scholar] [CrossRef] [PubMed]
- Burval, D.J.; McLain, R.F.; Milks, R.; İnceoğlu, S. Primary Pedicle Screw Augmentation in Osteoporotic Lumbar Vertebrae. Spine 2007, 32, 1077–1083. [Google Scholar] [CrossRef] [PubMed]
- Becker, S.; Chavanne, A.; Spitaler, R.; Kropik, K.; Aigner, N.; Ogon, M.; Redl, H. Assessment of different screw augmentation techniques and screw designs in osteoporotic spines. Eur. Spine J. 2008, 17, 1462–1469. [Google Scholar] [CrossRef] [PubMed]
- Matsuzaki, H.; Tokuhashi, Y.; Wakabayashi, K.; Okawa, A.; Hagiwara, H.; Iwahashi, M. Effects of hydroxyapatite solid granule (HA Stick) on pedicle screwing for osteoporotic patients. Clin. Orthop. Surg. 2001, 36, 529–534. (In Japanese) [Google Scholar]
- Shin, S.J.; Lee, J.H.; Lee, J.H. Influence of Hydroxyapatite Stick on Pedicle Screw Fixation in Degenerative Lumbar Spine: Biomechanical and Radiologic Study. Clin. Spine Surg. 2017, 30, E819–E826. [Google Scholar] [CrossRef] [PubMed]
- Foley, K.T.; Holly, L.T.; Schwender, J.D. Minimally invasive lumbar fusion. Spine 2003, 28, S26–S35. [Google Scholar] [CrossRef] [PubMed]
- Foley, K.T.; Gupta, S.K.; Justis, J.R.; Sherman, M.C. Percutaneous pedicle screw fixation of the lumbar spine. Neurosurg. Focus 2001, 10, E10. [Google Scholar] [CrossRef]
- Kuklo, T.R.; Dmitriev, A.E.; Cardoso, M.J.; Lehman, R.A.; Erickson, M.; Gill, N.W. Biomechanical contribution of transverse connectors to segmental stability following long segment instrumentation with thoracic pedicle screws. Spine 2008, 33, E482–E487. [Google Scholar] [CrossRef]
- Chutkan, N.B.; Zhou, H.; Akins, J.P.; Wenger, K.H. Effects of facetectomy and crosslink augmentation on motion segment flexibility in posterior lumbar interbody fusion. Spine 2008, 33, E828–E835. [Google Scholar] [CrossRef] [PubMed]
- Kanno, H.; Aizawa, T.; Hashimoto, K.; Itoi, E. Enhancing percutaneous pedicle screw fixation with hydroxyapatite granules: A biomechanical study using an osteoporotic bone model. PLoS ONE 2019, 14, e0223106. [Google Scholar] [CrossRef] [PubMed]
- Kanno, H.; Aizawa, T.; Hashimoto, K.; Itoi, E. Novel augmentation technique of percutaneous pedicle screw fixation using hydroxyapatite granules in the osteoporotic lumbar spine: A cadaveric biomechanical analysis. Eur. Spine J. 2021, 30, 71–78. [Google Scholar] [CrossRef]
- Kanno, H. Augmentation of percutaneous pedicle screw fixation: Novel method using hydroxyapatite granules and effectiveness of teriparatide. J. MIOS 2018, 87, 81–88. [Google Scholar]
- Kanno, H.; Murotani, M.; Aizawa, T.; Ozawa, H. Reinforcement of percutaneous pedicle screw fixation using hydroxyapatite granules: Prevention of postoperative screw loosening. In Proceedings of the 11th Annual Meeting of Society for Minimally Invasive Spinal Treatment, Tokyo, Japan, 29–30 October 2021; p. 87. [Google Scholar]
- Yi, S.; Rim, D.C.; Park, S.W.; Murovic, J.A.; Lim, J.; Park, J. Biomechanical Comparisons of Pull out Strengths after Pedicle Screw Augmentation with Hydroxyapatite, Calcium Phosphate, or Polymethylmethacrylate in the Cadaveric Spine. World Neurosurg. 2015, 83, 976–981. [Google Scholar] [CrossRef] [PubMed]
- Spivak, J.M.; Neuwirth, M.G.; Labiak, J.J.; Kummer, F.J.; Ricci, J.L. Hydroxyapatite enhancement of posterior spinal instrumentation fixation. Spine 1994, 19, 955–964. [Google Scholar] [CrossRef]
- Hasegawa, K.; Yamamura, S.; Dohmae, Y. Enhancing screw stability in osteosynthesis with hydroxyapatite granules. Arch. Orthop. Trauma Surg. 1998, 117, 175–176. [Google Scholar] [CrossRef] [PubMed]
- Yerby, S.A.; Toh, E.; McLain, R.F. Revision of failed pedicle screws using hydroxyapatite cement. A biomechanical analysis. Spine 1998, 23, 1657–1661. [Google Scholar] [CrossRef]
- Lotz, J.C.; Hu, S.S.; Chiu, D.F.; Yu, M.; Colliou, O.; Poser, R.D. Carbonated apatite cement augmentation of pedicle screw fixation in the lumbar spine. Spine 1997, 22, 2716–2723. [Google Scholar] [CrossRef]
- Spivak, J.M.; Hasharoni, A. Use of hydroxyapatite in spine surgery. Eur. Spine J. 2001, 10 (Suppl. 2), S197–S204. [Google Scholar] [CrossRef]
- Ohba, T.; Ebata, S.; Oba, H.; Koyama, K.; Haro, H. Risk factors for clinically relevant loosening of percutaneous pedicle screws. Spine Surg. Relat. Res. 2019, 3, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Ohtori, S.; Inoue, G.; Orita, S.; Yamauchi, K.; Eguchi, Y.; Ochiai, N.; Kishida, S.; Kuniyoshi, K.; Aoki, Y.; Nakamura, J.; et al. Comparison of teriparatide and bisphosphonate treatment to reduce pedicle screw loosening after lumbar spinal fusion surgery in postmenopausal women with osteoporosis from a bone quality perspective. Spine 2013, 38, E487–E492. [Google Scholar] [CrossRef] [PubMed]
- DeWald, C.J.; Stanley, T. Instrumentation-related complications of multilevel fusions for adult spinal deformity patients over age 65: Surgical considerations and treatment options in patients with poor bone quality. Spine 2006, 31, S144–S151. [Google Scholar] [CrossRef] [PubMed]
- Kueny, R.A.; Kolb, J.P.; Lehmann, W.; Püschel, K.; Morlock, M.M.; Huber, G. Influence of the screw augmentation technique and a diameter increase on pedicle screw fixation in the osteoporotic spine: Pullout versus fatigue testing. Eur. Spine J. 2014, 23, 2196–2202. [Google Scholar] [CrossRef]
- Elder, B.D.; Lo, S.-F.L.; Holmes, C.; Goodwin, C.R.; Kosztowski, T.A.; Lina, I.A.; Locke, J.E.; Witham, T.F. The biomechanics of pedicle screw augmentation with cement. Spine J. 2015, 15, 1432–1445. [Google Scholar] [CrossRef]
- Lieberman, I.H.; Togawa, D.; Kayanja, M.M. Vertebroplasty and kyphoplasty: Filler materials. Spine J. 2005, 5, 305S–316S. [Google Scholar] [CrossRef]
- Derincek, A.; Wu, C.; Mehbod, A.; Transfeldt, E.E. Biomechanical comparison of anatomic trajectory pedicle screw versus injectable calcium sulfate graft-augmented pedicle screw for salvage in cadaveric thoracic bone. J. Spinal Disord. Tech. 2006, 19, 286–291. [Google Scholar] [CrossRef]
- Tamai, N.; Myoui, A.; Tomita, T.; Nakase, T.; Tanaka, J.; Ochi, T.; Yoshikawa, H. Novel hydroxyapatite ceramics with an interconnective porous structure exhibit superior osteoconduction in vivo. J. Biomed. Mater. Res. B Appl. Biomater. 2002, 59, 110–117. [Google Scholar] [CrossRef]
- Krueger, A.; Bliemel, C.; Zettl, R.; Ruchholtz, S. Management of pulmonary cement embolism after percutaneous vertebroplasty and kyphoplasty: A systematic review of the literature. Eur. Spine J. 2009, 18, 1257–1265. [Google Scholar] [CrossRef]
- Abdul-Jalil, Y.; Bartels, J.; Alberti, O.; Becker, R. Delayed presentation of pulmonary polymethylmethacrylate emboli after percutaneous vertebroplasty. Spine 2007, 32, E589–E593. [Google Scholar] [CrossRef]
- Syed, M.I.; Jan, S.; Patel, N.A.; Shaikh, A.; Marsh, R.A.; Stewart, R.V. Fatal fat embolism after vertebroplasty: Identification of the high-risk patient. AJNR Am. J. Neuroradiol. 2006, 27, 343–345. [Google Scholar] [PubMed]
- Ahmadzai, H.; Campbell, S.; Archis, C.; Clark, W.A. Fat embolism syndrome following percutaneous vertebroplasty: A case report. Spine J. 2014, 14, e1–e5. [Google Scholar] [CrossRef] [PubMed]
- Laredo, J.D.; Hamze, B. Complications of percutaneous vertebroplasty and their prevention. Skeletal. Radiol. 2004, 33, 493–505. [Google Scholar] [CrossRef] [PubMed]
- Jang, J.S.; Lee, S.H.; Jung, S.K. Pulmonary embolism of polymethylmethacrylate after percutaneous vertebroplasty: A report of three cases. Spine 2002, 27, E416–E418. [Google Scholar] [CrossRef] [PubMed]
- Temple, J.D.; Ludwig, S.C.; Ross, W.K.; Marshall, W.K.; Larsen, L.; Gelb, D.E. Catastrophic fat embolism following augmentation of pedicle screws with bone cement: A case report. J. Bone Joint Surg. Am. 2002, 84, 639–642. [Google Scholar] [CrossRef] [PubMed]
- Fujibayashi, S.; Takemoto, M.; Neo, M.; Matsuda, S. Strategy for salvage pedicle screw placement: A technical note. Int. J. Spine Surg. 2013, 7, e67–e71. [Google Scholar] [CrossRef]
- Toyone, T.; Tanaka, T.; Kato, D.; Kaneyama, R.; Otsuka, M. The treatment of acute thoracolumbar burst fractures with transpedicular intracorporeal hydroxyapatite grafting following indirect reduction and pedicle screw fixation: A prospective study. Spine 2006, 31, E208–E214. [Google Scholar] [CrossRef]
- Takami, M.; Yamada, H.; Nohda, K.; Yoshida, M. A minimally invasive surgery combining temporary percutaneous pedicle screw fixation without fusion and vertebroplasty with transpedicular intracorporeal hydroxyapatite blocks grafting for fresh thoracolumbar burst fractures: Prospective study. Eur. J. Orthop. Surg. Traumatol. 2014, 24 (Suppl. 1), S159–S165. [Google Scholar] [CrossRef]
- Nishioka, K.; Imae, S.; Kitayama, M.; Miki, J.; Okawa, T.; Itakura, T. Percutaneous vertebroplasty using hydroxyapatite blocks for the treatment of vertebral body fracture. Neurol. Med. Chir. 2009, 49, 501–506. [Google Scholar] [CrossRef][Green Version]
- Satake, K.; Kanemura, T.; Yamaguchi, H.; Matsumoto, A. Pulmonary Embolism After Vertebroplasty with Use of Hydroxyapatite Blocks: A Case Report. JBJS Case Connect 2013, 3, e132. [Google Scholar] [CrossRef]
- Kanno, H. Answer to the Letter to the Editor of T. Morimoto et al. concerning “Novel augmentation technique of percutaneous pedicle screw fixation using hydroxyapatite granules in the osteoporotic lumbar spine: A cadaveric biomechanical analysis” by Kanno; et al. [Eur Spine J. 2021 Jan;30(1):71–78]. Eur. Spine J. 2022, 31, 212–213. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).