Is Kinesio Taping Effective for Sport Performance and Ankle Function of Athletes with Chronic Ankle Instability (CAI)? A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Sources and Search Strategy
2.2. Inclusion Criteria
2.3. Exclusion Criteria
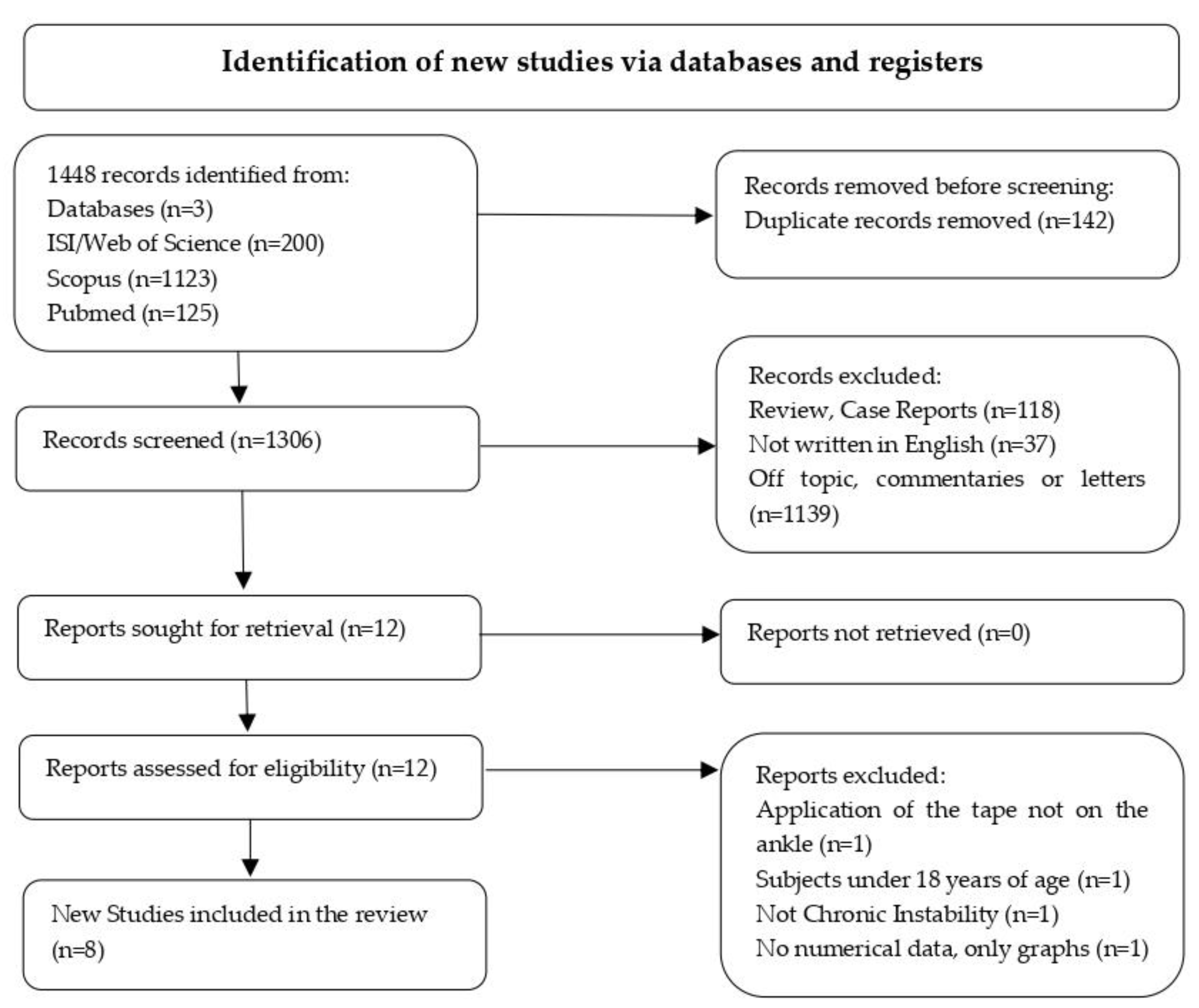
2.4. Screening
2.5. Data Collection
2.6. Quality Appraisal
2.7. Meta-Analysis
3. Results
3.1. Search Yield
3.2. Study Characteristics
3.3. Outcome Measurements
3.4. Quality Assessment
3.5. Meta-Analysis
4. Discussion
4.1. Gait Functions
4.2. Ankle Joint ROM
4.3. Muscle Contraction
4.4. Postural Sway during Movement
4.5. Dynamic Balance
4.6. Lateral Landing from Monopodalic Drop
4.7. Agility
4.8. Time of Application
4.9. Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Thompson, C.; Schabrun, S.; Romero, R.; Bialocerkowski, A.; van Dieen, J.; Marshall, P. Factors Contributing to Chronic Ankle Instability: A Systematic Review and Meta-Analysis of Systematic Reviews. Sports Med. 2018, 48, 189–205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, C.I.; Houtenbos, S.; Lu, Y.H.; Mayer, F.; Wippert, P.M. The epidemiology of chronic ankle instability with perceived ankle instability—A systematic review. J. Foot Ankle Res. 2021, 14, 41. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, T.; Tanaka, M.; Shida, M. Intrinsic Risk Factors of Lateral Ankle Sprain: A Systematic Review and Meta-analysis. Sports Health 2016, 8, 190–193. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Doherty, C.; Delahunt, E.; Caulfield, B.; Hertel, J.; Ryan, J.; Bleakley, C. The Incidence and Prevalence of Ankle Sprain Injury: A Systematic Review and Meta-Analysis of Prospective Epidemiological Studies. Sports Med. 2014, 44, 123–140. [Google Scholar] [CrossRef]
- Gribble, P.A.; Bleakley, C.M.; Caulfield, B.M.; Docherty, C.; Fourchet, F.; Fong, D.T. Evidence Review for the 2016 international ankle consortium consensus statement on the prevalence, impact and long-term consequences of lateral ankle sprains. Br. J. Sports Med. 2016, 50, 496–1505. [Google Scholar] [CrossRef] [Green Version]
- Knowles, S.B.; Marshall, S.W.; Miller, T.; Spicer, R.; Bowling, J.M.; Loomis, D.; Millikan, R.W.; Yang, J.; Mueller, F.O. Cost of injuries from a prospective cohort study of North Carolina high school athletes. Inj. Prev. 2007, 13, 416–421. [Google Scholar] [CrossRef] [Green Version]
- Owoeye, O.B.A.; Palacios-Derflingher, L.M.; Emery, C.A. Prevention of ankle sprain injuries in youth soccer and basketball: Effectiveness of a neuromuscular training program and examining risk factors. Clin. J. Sport Med. 2018, 28, 325–331. [Google Scholar] [CrossRef]
- Bicici, S.; Karatas, N.; Baltaci, G. Effect of athletic taping and kinesiotaping® on measurements of functional performance in basketball players with chronic inversion ankle sprains. Int. J. Sports Phys. Ther. 2012, 7, 154–166. [Google Scholar]
- Whalan, M.; Lovell, R.; McCunn, R.; Sampson, J.A. The incidence and burden of time loss injury in Australian men’s sub-elite football (soccer): A single season prospective cohort study. J. Sci. Med. Sport 2019, 2, 42–47. [Google Scholar] [CrossRef]
- Keogh, J.W.L.; Winwood, P.W. The epidemiology of injuries across the weight-training sports. Sports Med. 2017, 47, 479–501. [Google Scholar] [CrossRef] [Green Version]
- Gabbett, T.J. Incidence, site, and nature of injuries in amateur rugby league over three consecutive seasons. Br. J. Sports Med. 2000, 34, 98–103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Woods, C.; Hawkins, R.; Hulse, M.; Hodson, A. The Football Association Medical Research Programme: An audit of injuries in professional football: An analysis of ankle sprains. Br. J. Sports Med. 2003, 37, 233–288. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Attenborough, A.S.; Hiller, C.E.; Smith, R.M.; Stuelcken, M.; Greene, A.; Sinclair, P.J. Chronic ankle instability in sporting populations. Sports Med. 2014, 44, 1545–1556. [Google Scholar] [CrossRef] [PubMed]
- Herzog, M.M.; Kerr, Z.Y.; Marshall, S.W.; Wikstrom, E.A. Epidemiology of ankle sprains and chronic ankle instability. J. Athl. Train. 2019, 54, 603–610. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De-La-Torre-Domingo, C.; Alguacil-Diego, I.M.; Molina-Rueda, F.; Lopez-Roman, A.; Fernandez-Carnero, J. Effect of kinesiology tape on measurements of balance in subjects with chronic ankle instability: A randomized controlled trial. Arch. Phys. Med. Rehabil. 2015, 96, 2169–2175. [Google Scholar] [CrossRef] [PubMed]
- Hertel, J.; Corbett, R.O. An updated model of chronic ankle instability. J. Athl. Train. 2019, 54, 572–588. [Google Scholar] [CrossRef] [Green Version]
- Hiller, C.E.; Kilbreath, S.L.; Refshauge, K.M. Chronic ankle instability: Evolution of the model. J. Athl. Train. 2011, 46, 133–141. [Google Scholar] [CrossRef] [Green Version]
- Kobayashi, T.; Takabayashi, T.; Kudo, S.; Edama, M. The prevalence of chronic ankle instability and its relationship to foot arch characteristics in female collegiate athletes. Phys. Ther. Sport 2020, 46, 162–168. [Google Scholar] [CrossRef]
- Fong, D.T.; Hong, Y.; Chan, L.K.; Yung, P.S.; Chan, K.M. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007, 37, 73–94. [Google Scholar] [CrossRef] [Green Version]
- Almeida, S.A.; Trone, D.W.; Leone, D.M.; Shaffer, R.A.; Patheal, S.L.; Long, K. Gender differences in musculoskeletal injury rates: A function of symptom reporting? Med. Sci. Sports Exerc. 1999, 31, 1807–1812. [Google Scholar] [CrossRef]
- Gribble, P.A.; Hertel, J.; Denegar, C.R.; Buckley, W.E. The Effects of Fatigue and Chronic Ankle Instability on Dynamic Postural Control. J. Athl. Train. 2004, 39, 321–329. [Google Scholar] [PubMed]
- Cordova, M.L. Effects of ankle support on lower-extremity functional performance: A meta-analysis. Med. Sci. Sports Exerc. 2005, 37, 635. [Google Scholar] [CrossRef] [PubMed]
- Simon, J.; Garcia, W.; Docherty, C.L. The effect of kinesio tape on force sense in people with functional ankle instability. Clin. J. Sport Med. 2014, 24, 289–294. [Google Scholar] [CrossRef] [PubMed]
- Witchalls, J.; Blanch, P.; Waddington, G.; Adams, R. Intrinsic functional deficits associated with increased risk of ankle injuries: A systematic review with meta-analysis. Br. J. Sports Med. 2012, 46, 515–523. [Google Scholar] [CrossRef]
- Fraser, J.J.; Koldenhoven, R.M.; Jaffri, A.H.; Park, J.S.; Saliba, S.F.; Hart, J.M.; Hertel, J. Foot impairments contribute to functional limitation in individuals with ankle sprain and chronic ankle instability. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 1600–1610. [Google Scholar] [CrossRef]
- McCann, R.S.; Crossett, I.D.; Terada, M.; Kosik, K.B.; Bolding, B.A.; Gribble, P.A. Hip strength and star excursion balance test deficits of patients with chronic ankle instability. J. Sci. Med. Sport 2017, 20, 992–996. [Google Scholar] [CrossRef]
- McCann, R.S.; Bolding, B.A.; Terada, M.; Kosik, K.B.; Crossett, I.D.; Gribble, P.A. Isometric Hip Strength and Dynamic Stability of Individuals With Chronic Ankle Instability. J. Athl. Train. 2018, 53, 672–678. [Google Scholar] [CrossRef] [Green Version]
- Song, K.; Burcal, C.J.; Hertel, J.; Wikstrom, E.A. Increased Visual Use in Chronic Ankle Instability: A Meta-analysis. Med. Sci. Sports Exerc. 2016, 48, 2046–2056. [Google Scholar] [CrossRef]
- Burcal, C.J.; Trier, A.Y.; Wikstrom, E.A. Balance Training Versus Balance Training With STARS in Patients with Chronic Ankle Instability: A Randomized Controlled Trial. J. Sport Rehabil. 2017, 26, 347–357. [Google Scholar] [CrossRef]
- Hoch, M.C.; Staton, G.S.; Medina McKeon, J.M.; Mattacola, C.G.; McKeon, P.O. Dorsiflexion and dynamic postural control deficits are present in those with chronic ankle instability. J. Sci. Med. Sport 2012, 15, 574–579. [Google Scholar] [CrossRef]
- Martin, R.L.; Davenport, T.E.; Paulseth, S.; Wukich, D.K.; Godges, J.J. Ankle Stability and Movement Coordination Impairments: Ankle Ligament Sprains Clinical Practice Guidelines Linked to the International Classification of Functioning, Disability and Health. From the Orthopaedic Section of the American Physical Therapy Association. J. Orthop. Sports Phys. Ther. 2013, 43, A1–A40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gribble, P.A.; Delahunt, E.; Bleakley, C.; Caulfield, B.; Docherty, C.; Fourchet, F. Selection criteria for patients with chronic ankle instability in controlled research: A position statement of the International Ankle Consortium. Br. J. Sports Med. 2014, 48, 1014–1018. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Campolo, M.; Babu, J.; Dmochowska, K.; Scariah, S.; Varughese, J. A comparison of two taping techniques (kinesio and mcconnell) and their effect on anterior knee pain during functional activities. Int. J. Sports Phys. Ther. 2013, 2, 105–110. [Google Scholar]
- Sitler, M.R.; Horodyski, M. Effectiveness of prophylactic ankle stabilisers for prevention of ankle injuries. Sports Med. 1995, 20, 53–57. [Google Scholar] [CrossRef]
- Huang, C.Y.; Hsieh, T.H.; Lu, S.C.; Su, F.C. Effect of the Kinesio tape to muscle activity and vertical jump performance in healthy inactive people. Biomed. Eng. Online 2011, 10, 70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anandkumar, S.; Sudarshan, S.; Nagpal, P. Efficacy of kinesio taping on isokinetic quadriceps torque in knee osteoarthritis: A double blinded randomized controlled study. Physiother. Theory Pract. 2014, 30, 375–383. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Lee, B. The effects of kinesio tape on isokinetic muscular function of horse racing jockeys. J. Phys. Ther. Sci. 2013, 25, 1273–1277. [Google Scholar] [CrossRef] [Green Version]
- Parreira, P.C.; Costa, L.C.; Hespanhol, L.C., Jr.; Lopes, A.D.; Costa, L.O. Current evidence does not support the use of Kinesio Taping in clinical practice: A systematic review. J. Physiother. 2014, 60, 31–39. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Gu, Y.; Chen, J.; Luo, W.; He, W.; Han, Z.; Tian, J. Kinesio taping is superior to other taping methods in ankle functional performance improvement: A systematic review and meta-analysis. Clin. Rehabil. 2018, 32, 1472–1481. [Google Scholar] [CrossRef]
- Dolphin, M.; Brooks, G.; Calancie, B.; Rufa, A. Does the Direction of Kinesiology Tape Application Influence Muscle Activation in Asymptomatic Individuals? Int. J. Sports Phys. Ther. 2021, 16, 135–144. [Google Scholar] [CrossRef]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef] [PubMed]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Viera, A.J.; Garrett, J.M. Understanding Interobserver Agreement: The Kappa Statistic. Fam. Med. 2005, 37, 360–363. [Google Scholar] [PubMed]
- Downs, S.H.; Black, N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J. Epidemiol. Community Health 1998, 52, 377–384. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hedges, L.V.; Olkin, I. Statistical Methods for Meta-Analysis, 1st ed.; Academic Press: San Diego, CA, USA, 1985. [Google Scholar]
- Morris, S.B. Estimating effect sizes from pretest-posttest-control group designs. Organ. Res. Methods 2008, 11, 364–386. [Google Scholar] [CrossRef]
- Cohen, J. A Coefficient of Agreement for Nominal Scales. Educ. Psychol. Meas. 1960, 20, 37–46. [Google Scholar] [CrossRef]
- Kim, M.K.; Shin, Y.J. Immediate Effects of Ankle Balance Taping with Kinesiology Tape for Amateur Soccer Players with Lateral Ankle Sprain: A Randomized Cross-Over Design. Med. Sci. Monit. 2017, 23, 5534–5541. [Google Scholar] [CrossRef] [Green Version]
- Sarvestan, J.; Alaei, F.; Kazemi, N.S.; Khial, H.P.; Shirzad, E.; Svoboda, Z. Agility profile in collegiate athletes with chronic ankle sprain: The effect of Athletic and Kinesio taping among both genders. Sport Sci. Health 2018, 14, 407–414. [Google Scholar] [CrossRef]
- Souza, H.H.; Pacheco, I.; Gehrke, L.C.; de Freitas, G.P.; Loureiro-Chaves, R.F.; Pacheco, A.M. Evaluation of the effect of elastic bandage on the ankle basketball players with and without chronic instability. Rev. Bras. Med. Esporte 2018, 24, 460–464. [Google Scholar] [CrossRef]
- Gehrke, L.C.; Londero, L.X.; Loureiro-Chaves, R.F.; Souza, H.H. Effects of athletic taping on performance of basketball athletes with chronic ankle instability. Rev. Bras. Med. Esporte 2018, 24, 477–482. [Google Scholar] [CrossRef]
- Sarvestan, J.; Svoboda, Z. Acute Effect of Ankle Kinesio- and Athletic Taping on Ankle Range of Motion During Various Agility Tests in Athletes With Chronic Ankle Sprain. J. Sport Rehabil. 2019, 29, 527–532. [Google Scholar] [CrossRef] [PubMed]
- Alawna, M.; Mohamed, A.A. Short-term and long-term effects of ankle joint taping and bandaging on balance, proprioception and vertical jump among volleyball players with chronic ankle instability. Phys. Ther. Sport 2020, 46, 145–154. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.C.; Chen, S.J.; Lee, W.C.; Lin, C.F. Effects of Different Ankle Supports on the Single-Leg Lateral Drop Landing Following Muscle Fatigue in Athletes with Functional Ankle Instability. Int. J. Environ. Res. Public Health 2020, 17, 3438. [Google Scholar] [CrossRef] [PubMed]
- Sarvestan, J.; Ataabadi, P.A.; Svoboda, Z.; Kovačikova, Z.; Needle, A.R. The effect of ankle Kinesio™ taping on ankle joint biomechanics during unilateral balance status among collegiate athletes with chronic ankle sprain. Phys. Ther. Sport 2020, 45, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Doherty, C.; Bleakley, C.; Delahunt, E.; Holden, S. Treatment and prevention of acute and recurrent ankle sprain: An overview of systematic reviews with meta-analysis. Br. J. Sports Med. 2017, 51, 113–125. [Google Scholar] [CrossRef]
- Van der Wees, P.J.; Lenssen, A.F.; Hendriks, E.J.; Stomp, D.J.; Dekker, J.; de Bie, R.A. Effectiveness of exercise therapy and manual mobilisation in ankle sprain and functional instability: A systematic review. Aust. J. Physiother. 2006, 52, 27–37. [Google Scholar] [CrossRef] [Green Version]
- Bonnel, F.; Toullec, E.; Mabit, C.; Tourné, Y. Chronic ankle instability: Biomechanics and pathomechanics of ligaments injury and associated lesions. Orthop. Traumatol. Surg. Res. 2010, 96, 424–432. [Google Scholar] [CrossRef]
- Al Adal, S.; Pourkazemi, F.; Mackey, M.; Hiller, C.E. The Prevalence of Pain in People with Chronic Ankle Instability: A Systematic Review. J. Athl. Train. 2019, 54, 662–670. [Google Scholar] [CrossRef]
- Aiken, A.B.; Pelland, L.; Brison, R. Short-term natural recovery of ankle sprains following discharge from emergency departments. J. Orthop. Sports Phys. Ther. 2008, 38, 566–571. [Google Scholar] [CrossRef] [Green Version]
- Patrick, O.M.; Gabriele, P.; Christopher, D.I. Effects of balance training on gait parameters in patients with chronic ankle instability: A randomized controlled trial. Clin. Rehabil. 2009, 23, 609–621. [Google Scholar] [CrossRef]
- Chinn, L.; Dicharry, J.; Hart, J.; Saliba, S. Gait kinematics after taping in participants with chronic ankle instability. J. Athl. Train. 2014, 49, 322–330. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fukuchi, C.A.; Fukuchi, R.K.; Duarte, M. Effects of walking speed on gait biomechanics in healthy participants: A systematic review and meta-analysis. Syst. Rev. 2019, 8, 153. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boyer, K.A.; Johnson, R.T.; Banks, J.J.; Jewell, C.; Hafer, J.F. Systematic review and meta-analysis of gait mechanics in young and older adults. Exp. Gerontol. 2017, 95, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Fransz, D.P.; Huurnink, A.; Kingma, I.; Verhagen, E.A.; van Dieën, J.H. A systematic review and meta-analysis of dynamic tests and related force plate parameters used to evaluate neuromusculoskeletal function in foot and ankle pathology. Clin. Biomech. 2013, 28, 591–601. [Google Scholar] [CrossRef] [Green Version]
- Hof, A.; Gazendam, M.; Sinke, W. The condition for dynamic stability. J. Biomech. 2005, 38, 1–8. [Google Scholar] [CrossRef]
- Romero-Franco, N.; Martínez-López, E.; Lomas-Vega, R.; Hita-Contreras, F.; Martínez-Amat, A. Effects of proprioceptive training program on core stability and center of gravity control in sprinters. J. Strength Cond. Res. 2012, 26, 2071–2077. [Google Scholar] [CrossRef] [Green Version]
- Tanaka, R.; Kubota, T.; Yamasaki, T.; Higashi, A. Validity of the total body centre of gravity during gait using a markerless motion capture system. J. Med. Eng. Technol. 2018, 42, 175–181. [Google Scholar] [CrossRef]
- Bok, S.K.; Lee, T.H.; Lee, S.S. The effects of changes of ankle strength and range of motion according to aging on balance. Ann. Rehabil. Med. 2013, 37, 10. [Google Scholar] [CrossRef]
- Kim, S.G.; Kim, W.S. Effect of ankle range of motion (ROM) and lower-extremity muscle strength on static balance control ability in young adults: A regression analysis. Med. Sci. Monit. 2018, 24, 3168. [Google Scholar] [CrossRef]
- Lin, C.C.; Lee, W.C.; Chen, J.C.; Chen, S.J.; Lin, C.F. The Influence of Kinesio Tape and an Ankle Brace on the Lower Extremity Joint Motion in Fatigued, Unstable Ankles during a Lateral Drop Landing. Int. J. Environ. Res. Public Health 2021, 18, 6081. [Google Scholar] [CrossRef]
- Smith, M.D.; Vitharana, T.N.; Wallis, G.M.; Vicenzino, B. Response profile of fibular repositioning tape on ankle osteokinematics, arthrokinematics, perceived stability and confidence in chronic ankle instability. Musculoskelet. Sci. Pract. 2020, 50, 102. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.G.; Lee, J.H. Immediate effects of ankle balance taping with kinesiology tape on the dynamic balance of young players with functional ankle instability. Technol. Health Care 2015, 23, 333–341. [Google Scholar] [CrossRef]
- Csapo, R.; Alegre, L.M. Effects of Kinesio® taping on skeletal muscle strength-A meta-analysis of current evidence. J. Sci. Med. Sport 2015, 18, 450–456. [Google Scholar] [CrossRef] [PubMed]
- Christou, E.A. Patellar taping increases vastus medialis oblique activity in the presence of patellofemoral pain. J. Electromyogr. Kinesiol. 2004, 14, 495–504. [Google Scholar] [CrossRef] [PubMed]
- Morrissey, D. Proprioceptive shoulder taping. J. Bodyw. Mov. Ther. 2000, 4, 189–194. [Google Scholar] [CrossRef]
- Hammer, W. Functional Soft-Tissue Examination and Treatment by Manual Methods, 3rd ed.; Jones and Bartlett Publishers: Boston, MA, USA, 2006. [Google Scholar]
- Chou, L.S.; Kaufman, K.R.; Brey, R.H.; Draganich, L.F. Motion of the whole body’s center of mass when stepping over obstacles of different heights. Gait Posture 2001, 13, 17–26. [Google Scholar] [CrossRef]
- Chou, L.S.; Kaufman, K.R.; Hahn, M.E.; Brey, R.H. Medio-lateral motion of the center of mass during obstacle crossing distinguishes elderly individuals with imbalance. Gait Posture 2003, 18, 125–133. [Google Scholar] [CrossRef]
- Lee, H.J.; Chou, L.S. Detection of gait instability using the center of mass and center of pressure inclination angles. Arch. Phys. Med. Rehabil. 2006, 87, 569–575. [Google Scholar] [CrossRef]
- Kurz, E.; Faude, O.; Roth, R.; Zahner, L.; Donath, L. Ankle muscle activity modulation during single-leg stance differs between children, young adults and seniors. Eur. J. Appl. Physiol. 2018, 118, 239–247. [Google Scholar] [CrossRef]
- Kim, B.J.; Lee, J.H.; Kim, C.T.; Lee, S.M. Effects of ankle balance taping with kinesiology tape for a patient with chronic ankle instability. J. Phys. Ther. Sci. 2015, 27, 2405–2406. [Google Scholar] [CrossRef] [Green Version]
- Hadadi, M.; Haghighat, F.; Mohammadpour, N.; Sobhani, S. Effects of Kinesiotape vs Soft and Semirigid Ankle Orthoses on Balance in Patients with Chronic Ankle Instability: A Randomized Controlled Trial. Foot Ankle Int. 2020, 41, 793–802. [Google Scholar] [CrossRef] [PubMed]
- Briem, K.; Eythörsdöttir, H.; Magnúsdóttir, R.G.; Pálmarsson, R.; Rúnarsdöttir, T.; Sveinsson, T. Effects of Kinesio tape compared with nonelastic sports tape and the untaped ankle during a sudden inversion perturbation in male athletes. J. Orthop. Sports Phys. Ther. 2011, 41, 328–335. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fayson, S.D.; Needle, A.R.; Kaminski, T.W. The effects of ankle Kinesio taping on ankle stiffness and dynamic balance. Res. Sports Med. 2013, 21, 204–216. [Google Scholar] [CrossRef] [PubMed]
- Gross, T.S.; Nelson, R.C. The shock attenuation role of the ankle during landing from a vertical jump. Med. Sci. Sports Exerc. 1988, 20, 506–514. [Google Scholar] [CrossRef]
- Zhang, S.N.; Bates, B.T.; Dufek, J.S. Contributions of lower extremity joints to energy dissipation during landings. Med. Sci. Sports Exerc. 2000, 32, 812–819. [Google Scholar] [CrossRef]
- Riemann, B.L.; Schmitz, R.J.; Gale, M.; McCaw, S.T. Effect of ankle taping and bracing on vertical ground reaction forces during drop landings before and after treadmill jogging. J. Orthop. Sports Phys. Ther. 2002, 32, 628–635. [Google Scholar] [CrossRef] [Green Version]
- Mason-Mackay, A.R.; Whatman, C.; Reid, D. The effect of reduced ankle dorsiflexion on lower extremity mechanics during landing: A systematic review. J. Sci. Med. Sport 2017, 20, 451–458. [Google Scholar] [CrossRef]
- Jackson, K.; Simon, J.E.; Docherty, C.L. Extended use of kinesiology tape and balance in participants with chronic ankle instability. J. Athl. Train. 2016, 51, 16–21. [Google Scholar] [CrossRef] [Green Version]
- Delahunt, E.; McGrath, A.; Doran, N.; Coughlan, G.F. Effect of taping on actual and perceived dynamic postural stability in persons with chronic ankle instability. Arch. Phys. Med. Rehabil. 2010, 91, 1383–1389. [Google Scholar] [CrossRef]
- Hunt, E.; Short, S. Collegiate Athletes’ Perceptions of Adhesive Ankle Taping: A Qualitative Analysis. J. Sport Rehabil. 2006, 15, 280–298. [Google Scholar] [CrossRef] [Green Version]
- Sawkins, K.; Refshauge, K.; Kilbreath, S.; Raymond, J. The placebo effect of ankle taping in ankle instability. Med. Sci. Sports Exerc. 2007, 39, 781–787. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Author (Publication Year) | Type of Study | Level of Evidence | n (m/f) | Age (Years *) | Sport |
|---|---|---|---|---|---|
| Kim et al. (2017) [48] | Cross-Over Randomised Design | I | 22 (m) | 17.72 ± 0.76 | Football |
| Sarvestan et al. (2018) [49] | Cross-Sectional Randomised Design | II | 26 (13 m/13 f) | 23.9 ± 1.6 | University Athletes |
| Souza et al. (2018) [50] | Cross-Sectional Randomised Trial | II | 13 (9 m/4 f) | 23.2 ± 3.2 | Basketball |
| Gehrke et al. (2018) [51] | Cross-Sectional Randomised Trial | II | 21 (14 m/7 f) | 23.7 ± 3.2 | Basketball |
| Sarvestan et al. (2019) [52] | Cross-Sectional Randomised Design | II | 25 (13 m/12 f) | 23.8 ± 1.62 | College Athletes |
| Alawna et al. (2020) [53] | Randomised Controlled Trial | I | 100 (56 m/44 f) | 22.25 ± 2.96 | Volleyball |
| Lin et al. (2020) [54] | Randomised Controlled Trial | I | 33 (25 m/8 f) | 22.0 ± 2.8 | Basketball, volleyball, baseball and badminton |
| Sarvestan et al. (2020) [55] | Case-Control Study | III | 30 (19 m/11 f) | 23.91 ± 2.58 | College Athletes |
| TOTAL | 270 (171 m/99 f) |
| Author (Publication Year) | n (m/f) | Outcome Measurements | Test |
|---|---|---|---|
| Kim et al. (2017) [48] | 22 (m) | Gait Functions | GAITRite PORTABLE WALKAWAY SYSTEMc (cm) |
| Sarvestan et al. (2018) [49] | 26 (13 m/13 f) | Agility | Illinois, 5-0-5, 10-m Shuttle, Hexagon, Compass Drill, T-Agility Test (*s) |
| Souza et al. (2018) [50] | 13 (9 m/4 f) | Dynamic Balance | SEBT (*cm) |
| Gehrke et al. (2018) [51] | 21 (14 m/7 f) | Dynamic Balance Agility | SEBT (cm) Figure-of-8 (s) |
| Sarvestan et al. (2019) [52] | 25 (13 m/12 f) | ROM during Agility tests | Illinois, 5-0-5, 10-m Shuttle, Hexagon, Compass Drill, T-Agility Test (s) |
| Alawna et al. (2020) [53] | 100 (56 m/44 f) | Dynamic Balance *ROM Vertical Jump | Y Balance Test (inches) ROM (degrees) Vertical Jump (inches) |
| Lin et al. (2020) [54] | 33 (25 m/8 f) | Lateral landing performance in single-leg drop | KISTLER FORCE PLATE PEAK *vGRF (%BW), Loading Rate (N/ms), Loading Time (ms), Difference of *CoP-range, Difference of CoP-velocity |
| Sarvestan et al. (2020) [55] | 30 (19 m/11 f) | Postural sway parameters ROM Muscle Activation | KISTLER FORCE PLATE PEAK (cm) ROM (degrees) EMG (% peak) |
| TOTAL | 270 (171 m/99 f) |
| ITEM | Kim et al. (2017) [48] | Sarvestan et al. (2018) [49] | Souza et al. (2018) [50] | Gehrke et al. (2018) [51] | Sarvestan et al. (2019) [52] | Alawna et a.l (2020) [53] | Lin et al. (2020) [54] | Sarvestan et al. (2020) [55] |
|---|---|---|---|---|---|---|---|---|
| 1. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 2. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 3. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 4. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 5. | 2 | 1 | 2 | 2 | 0 | 2 | 2 | 0 |
| 6. | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 |
| 7. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 8. | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 |
| 9. | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 10. | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 1 |
| 11. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 12. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 13. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 14. | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 0 |
| 15. | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 0 |
| 16. | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 17. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 18. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 19. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 20. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 21. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 22. | U/D | U/D | U/D | U/D | U/D | U/D | U/D | U/D |
| 23. | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 0 |
| 24. | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 0 |
| 25. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 |
| 26. | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 27. | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 |
| TOTAL | 21/28 | 17/28 | 22/28 | 21/28 | 16/28 | 21/28 | 20/28 | 16/28 |
| Parameter | Effect Size or ES (SMD) | Standard Error | 95% CI | p-Value | I2 |
|---|---|---|---|---|---|
| Dynamic Balance | |||||
| SEBT | 0.197 | 0.237 | −0.268 to 0.662 | 0.406 | 0.00% |
| SEBT-A | 0.0979 | 0.237 | −0.375 to 0.571 | 0.681 | 0.00% |
| SEBT-AM | 0.269 | 0.238 | −0.206 to 0.744 | 0.263 | 0.00% |
| SEBT-M | 0.199 | 0.237 | −0.275 to 0.673 | 0.405 | 0.00% |
| SEBT-PM | 0.211 | 0.237 | −0.263 to 0.685 | 0.377 | 0.00% |
| SEBT-P | 0.187 | 0.237 | −0.286 to 0.661 | 0.433 | 0.00% |
| SEBT-PL | 0.250 | 0.238 | −0.224 to 0.725 | 0.296 | 0.00% |
| SEBT-L | 0.286 | 0.238 | −0.189 to 0.761 | 0.234 | 0.00% |
| SEBT-AL | 0.0753 | 0.237 | −0.398 to 0.548 | 0.752 | 0.00% |
| Lateral Landing | |||||
| Kistler force plate peak vGRF—ground reaction forces | 0.09 (overall ES sensu Morris) 0.134 (overall ES sensu Klauer) | ||||
| 0.588 (pre) | 0.246 | 0.095 to 1.081 | 0.017 | 0.00% | |
| 0.455 (post) | 0.249 | −0.034 to 0.943 | 0.068 | 0.00% | |
| Loading Rate | 0.243 (overall ES sensu Morris) 0.233 (overall ES sensu Klauer) | ||||
| 0.127 (pre) | 0.246 | −0.356 to 0.61 | 0.606 | 0.00% | |
| 0.360 (post) | 0.248 | −0.126 to 0.846 | 0.147 | 0.00% | |
| Loading Time | 0.760 (overall ES sensu Morris) 0.836 (overall ES sensu Klauer) | ||||
| 0.119 (pre) | 0.246 | −0.364 to 0.602 | 0.629 | 0.00% | |
| 0.717 (post) | 0.366 | −0.22 to 1.215 | 0.050 | 0.00% | |
| Gait Functions | |||||
| Velocity | 1.978 | 0.368 | 1.257 to 2.699 | 0.000 | 0.00% |
| Step | 2.271 | 0.387 | 1.513 to 3.029 | 0.000 | 0.00% |
| Stride | 2.277 | 0.387 | 1.519 to 3.036 | 0.000 | 0.00% |
| H-H Base support | 1.920 | 0.365 | 1.205 to 2.634 | 0.000 | 0.00% |
| Agility | |||||
| Illinois | Male: 0.213 (overall ES sensu Morris) | 0.410 | −0.59 to 1.02 | 0.603 | 0.00% |
| 0.254 (overall sensu Klauer); | 0.410 | −0.55 to 1.06 | 0.536 | 0.00% | |
| Female: −0.136 (overall ES sensu Morris) | 0.409 | −0.94 to 0.67 | 0.739 | 0.00% | |
| −0.186 (overall sensu Klauer) | 0.409 | −0.99 to 0.62 | 0.649 | 0.00% | |
| 5-0-5 | Male: −0.329 (overall ES sensu Morris) | 0.411 | −1.14 to 0.48 | 0.424 | 0.00% |
| −0.425 (overall sensu Klauer); | 0.413 | −1.23 to 0.38 | 0.304 | 0.00% | |
| Female: −0.412 (overall ES sensu Morris) | 0.413 | −1.22 to 0.40 | 0.318 | 0.00% | |
| −0.481 (overall sensu Klauer) | 0.415 | −1.29 to 0.33 | 0.246 | 0.00% | |
| 10-m Shuttle | Male: −0.351 (overall ES sensu Morris) | 0.412 | −1.16 to 0.46 | 0.394 | 0.00% |
| −0.525 (overall sensu Klauer); | 0.416 | −1.34 to 0.29 | 0.207 | 0.00% | |
| Female: −0.56 (overall ES sensu Morris) | 0.417 | −1.38 to 0.26 | 0.179 | 0.00% | |
| −0.456 (overall sensu Klauer) | 0.414 | −1.27 to 0.36 | 0.271 | 0.00% | |
| Hexagon | Male: 0.127 (overall ES sensu Morris) | 0.409 | −0.67 to 0.93 | 0.756 | 0.00% |
| 0.253 (overall sensu Klauer); | 0.410 | −0.55 to 1.06 | 0.537 | 0.00% | |
| Female: 0.312 (overall ES sensu Morris) | 0.411 | −0.49 to 1.12 | 0.448 | 0.00% | |
| 0.252 (overall sensu Klauer) | 0.410 | −0.55 to 1.06 | 0.539 | 0.00% | |
| Compass Drill | Male: −0.055 (overall ES sensu Morris) | 0.408 | −0.86 to 0.75 | 0.893 | 0.00% |
| −0.061 (overall sensu Klauer); | 0.408 | −0.86 to 0.74 | 0.881 | 0.00% | |
| Female: −0.067 (overall ES sensu Morris) | 0.408 | −0.87 to 0.73 | 0.870 | 0.00% | |
| −0.092 (overall sensu Klauer) | 0.408 | −0.89 to 0.71 | 0.822 | 0.00% | |
| T-Agility Test | Male: 0.339 (overall ES sensu Morris) | 0.411 | −0.47 to 1.15 | 0.410 | 0.00% |
| 0.341 (overall sensu Klauer); | 0.411 | −0.47 to 1.15 | 0.407 | 0.00% | |
| Female: −0.402 (overall ES sensu Morris) | 0.413 | −1.21 to 0.41 | 0.330 | 0.00% | |
| −0.415 (overall sensu Klauer) | 0.413 | −1.22 to 0.39 | 0.315 | 0.00% | |
| Figure of 8 | 0.302 | 0.310 | −0.307 to 0.910 | 0.331 | 0.00% |
| ROM | |||||
| Ankle angle peak Dorsi–-Plantar flexion | 0.03 | 0.258 | −0.48 to 0.54 | 0.908 | 0.00% |
| Ankle angle Inversion–Eversion | 0.52 | 0.263 | 0.00 to 1.04 | 0.048 | 0.00% |
| Knee angle peak Flexion–Extension | 0.01 | 0.258 | −0.50 to 0.52 | 0.978 | 0.00% |
| Hip angle Peak Flexion–Extension | 0.05 | 0.258 | −0.46 to 0.56 | 0.831 | 0.00% |
| Hip angle Peak Abduction–Adduction | 0.12 | 0.258 | −0.39 to 0.63 | 0.794 | 0.00% |
| Sway parameters | |||||
| Sway length | 0.14 | 0.259 | −0.37 to 0.65 | 0.436 | 0.00% |
| Sway area | 0.37 | 0.261 | −0.14 to 0.88 | 0.499 | 0.00% |
| Sway displacement anterior–posterior | 0.15 | 0.259 | −0.36 to 0.66 | 0.433 | 0.00% |
| Sway displacement medial–lateral | 0.46 | 0.262 | −0.05 to 0.97 | 0.162 | 0.00% |
| Total velocity | 0.16 | 0.259 | −0.35 to 0.67 | 0.436 | 0.00% |
| Sway velocity anterior–posterior | 0.17 | 0.259 | −0.34 to 0.68 | 0.433 | 0.00% |
| Sway velocity medial–lateral | 1.25 | 0.284 | 0.69 to 1.81 | 0.029 | 0.00% |
| Average muscle activity (% Peak) | |||||
| Lateral Gastrocnemius | 0.01 | 0.258 | −0.50 to 0.52 | 0.963 | 0.00% |
| Medial Gastrocnemius | 0.01 | 0.258 | −0.50 to 0.52 | 0.901 | 0.00% |
| Tibialis Anterior | 0.06 | 0.258 | −0.45 to 0.57 | 0.674 | 0.00% |
| Peroneus Longus | 0.55 | 0.263 | 0.03 to 1.07 | 0.042 | 0.00% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Biz, C.; Nicoletti, P.; Tomasin, M.; Bragazzi, N.L.; Di Rubbo, G.; Ruggieri, P. Is Kinesio Taping Effective for Sport Performance and Ankle Function of Athletes with Chronic Ankle Instability (CAI)? A Systematic Review and Meta-Analysis. Medicina 2022, 58, 620. https://doi.org/10.3390/medicina58050620
Biz C, Nicoletti P, Tomasin M, Bragazzi NL, Di Rubbo G, Ruggieri P. Is Kinesio Taping Effective for Sport Performance and Ankle Function of Athletes with Chronic Ankle Instability (CAI)? A Systematic Review and Meta-Analysis. Medicina. 2022; 58(5):620. https://doi.org/10.3390/medicina58050620
Chicago/Turabian StyleBiz, Carlo, Pietro Nicoletti, Matteo Tomasin, Nicola Luigi Bragazzi, Giuseppe Di Rubbo, and Pietro Ruggieri. 2022. "Is Kinesio Taping Effective for Sport Performance and Ankle Function of Athletes with Chronic Ankle Instability (CAI)? A Systematic Review and Meta-Analysis" Medicina 58, no. 5: 620. https://doi.org/10.3390/medicina58050620
APA StyleBiz, C., Nicoletti, P., Tomasin, M., Bragazzi, N. L., Di Rubbo, G., & Ruggieri, P. (2022). Is Kinesio Taping Effective for Sport Performance and Ankle Function of Athletes with Chronic Ankle Instability (CAI)? A Systematic Review and Meta-Analysis. Medicina, 58(5), 620. https://doi.org/10.3390/medicina58050620









