Cutaneous Ulcer Caused by Apixaban Treatment Is Resolved after Replacement with Dabigatran
Abstract
1. Introduction
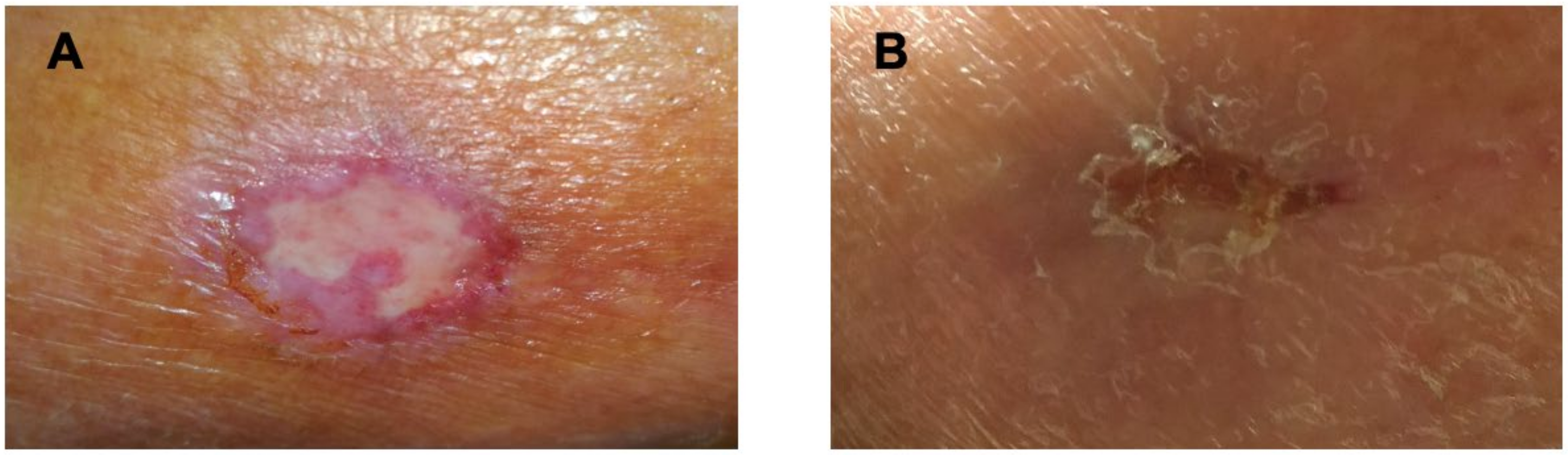
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kovacs, R.J.; Flaker, G.C.; Saxonhouse, S.J.; Doherty, J.U.; Birtcher, K.K.; Cuker, A.; Davidson, B.L.; Giugliano, R.; Granger, C.B.; Jaffer, A.K.; et al. Practical Management of Anticoagulation in Patients With Atrial Fibrillation. J. Am. Coll. Cardiol. 2015, 65, 1340–1360. [Google Scholar] [CrossRef] [PubMed]
- Bacchus, F.; Schulman, S. Clinical Experience With the New Oral Anticoagulants for Treatment of Venous Thromboembolism. Arter. Thromb. Vasc. Biol. 2015, 35, 513–519. [Google Scholar] [CrossRef] [PubMed]
- Yeh, C.H.; Hogg, K.; Weitz, J.I. Overview of the New Oral Anticoagulants: Opportunities and Challenges. Arter. Thromb. Vasc. Biol. 2015, 35, 1056–1065. [Google Scholar] [CrossRef] [PubMed]
- Harrington, A.R.; Armstrong, E.P.; Nolan, P.E.; Malone, D.C. Cost-Effectiveness of Apixaban, Dabigatran, Rivaroxaban, and Warfarin for Stroke Prevention in Atrial Fibrillation. Stroke 2013, 44, 1676–1681. [Google Scholar] [CrossRef] [PubMed]
- Dentali, F.; Riva, N.; Crowther, M.; Turpie, A.G.; Lip, G.Y.; Ageno, W. Efficacy and Safety of the Novel Oral Anticoagulants in Atrial Fibrillation: A Systematic Review and Meta-Analysis of the Literature. Circulation 2012, 126, 2381–2391. [Google Scholar] [CrossRef] [PubMed]
- Miller, C.S.; Grandi, S.M.; Shimony, A.; Filion, K.B.; Eisenberg, M.J. Meta-analysis of efficacy and safety of new oral anticoagulants (dabigatran, rivaroxaban, apixaban) versus warfarin in patients with atrial fibrillation. Am. J. Cardiol. 2012, 110, 453–60. [Google Scholar] [CrossRef]
- You, J.J.; Singer, D.E.; Howard, P.A.; Lane, D.A.; Eckman, M.; Fang, M.C.; Hylek, E.M.; Schulman, S.; Go, A.S.; Hughes, M.; et al. Antithrombotic Therapy for Atrial Fibrillation. Chest 2012, 141, e531S–e575S. [Google Scholar] [CrossRef]
- Schulman, S.; Kearon, C.; Kakkar, A.K.; Mismetti, P.; Schellong, S.; Eriksson, H.; Baanastra, D.; Schnee, J.; Goldhaber, S.Z.; RE-COVER Study Group. Dabigatran versus Warfarin in the Treatment of Acute Venous Thromboembolism. N. Engl. J. Med. 2009, 361, 2342–2352. [Google Scholar] [CrossRef]
- Schulman, S.; Kakkar, A.K.; Goldhaber, S.Z.; Schellong, S.; Eriksson, H.; Mismetti, P.; Christiansesn, A.V.; Friedman, J.; Le Maulf, F.; Peter, N.; et al. Treatment of acute venous thromboembolism with dabigatran or warfarin and pooled analysis. Circulation 2014, 129, 764–72. [Google Scholar] [CrossRef]
- Agnelli, G.; Buller, H.R.; Cohen, A.; Curto, M.; Gallus, A.S.; Johnson, M.; Masiukiewicz, U.; Pak, R.; Thompson, J.; Raskob, G.E.; et al. Oral apixaban for the treatment of acute venous thromboembolism. N. Engl. J. Med. 2013, 368, 799–808. [Google Scholar] [CrossRef]
- Büller, H.; Décousus, H.; Grosso, M.; Mercuri, M.; Middeldorp, S.; Prins, M.; Raskob, G.E.; Schellong, S.M.; Schwocho, L.; Segers, A.; et al. Edoxaban versus warfarin for the treatment of symptomatic venous thromboembolism. N. Engl. J. Med. 2013, 369, 1406–1415. [Google Scholar] [CrossRef] [PubMed]
- Bauersachs, R.; Berkowitz, S.; Brenner, B.; Buller, H.; Decousus, H.; Gallus, A.; Lensing, A.W.; Misselwitz, F.; Prins, M.H.; Raskob, G.E.; et al. Oral Rivaroxaban for Symptomatic Venous Thromboembolism. N. Engl. J. Med. 2010, 363, 2499–510. [Google Scholar] [CrossRef] [PubMed]
- Gulseth, M.P.; Wittkowsky, A.K.; Fanikos, J.; A Spinler, S.; E Dager, W.; A Nutescu, E. Dabigatran Etexilate in Clinical Practice: Confronting Challenges to Improve Safety and Effectiveness. Pharmacotherapy 2011, 31, 1232–1249. [Google Scholar] [CrossRef] [PubMed]
- Abraham, N.S.; Singh, S.; Caleb, A.G.; Heien, H.; Haas, L.R.; Crown, W.; Shah, N.D. Comparative risk of gastrointestinal bleeding with dabigatran, rivaroxaban, and warfarin: Population based cohort study. BMJ 2015, 350, 1857. [Google Scholar] [CrossRef]
- Raschi, E.; Bianchin, M.; Ageno, W.; De Ponti, R.; De Ponti, F. Risk–Benefit Profile of Direct-Acting Oral Anticoagulants in Established Therapeutic Indications: An Overview of Systematic Reviews and Observational Studies. Drug Saf. 2016, 39, 1175–1187. [Google Scholar] [CrossRef] [PubMed]
- Monaco, L.; Biagi, C.; Conti, V.; Melis, M.; Donati, M.; Venegoni, M.; Vaccheri, A.; Motola, D. Safety profile of the direct oral anticoagulants: An analysis of the WHO database of adverse drug reactions. Br. J. Clin. Pharmacol. 2017, 83, 1532–1543. [Google Scholar] [CrossRef]
- Raschi, E.; Bianchin, M.; Ageno, W.; De Ponti, R.; De Ponti, F. Adverse events associated with the use of direct-acting oral anticoagulants in clinical practice: Beyond bleeding complications. Pol. Arch. Intern. Med. 2016, 126, 552–561. [Google Scholar] [CrossRef]
- Kupó, P.; Szakács, Z.; Solymár, M.; Habon, T.; Czopf, L.; Hategan, L.; Csányi, B.; Borbás, J.; Tringer, A.; Varga, G.; et al. Direct Anticoagulants and Risk of Myocardial Infarction, a Multiple Treatment Network Meta-Analysis. Angiology 2020, 71, 27–37. [Google Scholar] [CrossRef]
- Aslan, A.N.; Sari, C.; Baştuğ, S.; Sari, S.; Akçay, M.; Durmaz, T.; Bozkurt, E. Severe jaundice due to intrahepatic cholestasis after initiating anticoagulation with rivaroxaban. Blood Coagul. Fibrinolysis 2016, 27, 226–227. [Google Scholar] [CrossRef]
- Ryan, M.; Ware, K.; Qamri, Z.; Satoskar, A.; Wu, H.; Nadasdy, G.; Rovin, B.; Hebert, L.; Nadasdy, T.; Brodsky, S.V. Warfarin-related nephropathy is the tip of the iceberg: Direct thrombin inhibitor dabigatran induces glomerular hemorrhage with acute kidney injury in rats. Nephrol. Dial. Transplant. 2014, 29, 2228–2234. [Google Scholar] [CrossRef]
- Josyln, J.A.; Khattak, F.H.; Geraci, S.A. A Case of a Reversible Neurologic Adverse Reaction to Apixaban Confirmed by Re-Challenge. J. Clin. Med. Res. 2018, 10, 523–526. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Galgani, A.; Palleria, C.; Iannone, L.F.; De Sarro, G.; Giorgi, F.S.; Maschio, M.; Russo, E. Pharmacokinetic Interactions of Clinical Interest Between Direct Oral Anticoagulants and Antiepileptic Drugs. Front. Neurol. 2018, 9, 1067. [Google Scholar] [CrossRef] [PubMed]
- Holm, J.; Mannheimer, B.; E Malmström, R.; Eliasson, E.; Lindh, J.D. Bleeding and thromboembolism due to drug-drug interactions with non-vitamin K antagonist oral anticoagulants—A Swedish, register-based cohort study in atrial fibrillation outpatients. Eur. J. Clin. Pharmacol. 2021, 77, 409–419. [Google Scholar] [CrossRef] [PubMed]
- Pham, P.; Schmidt, S.; Lesko, L.; Lip, G.Y.H.; Brown, J.D. Association of Oral Anticoagulants and Verapamil or Diltiazem With Adverse Bleeding Events in Patients With Nonvalvular Atrial Fibrillation and Normal Kidney Function. JAMA Netw. Open 2020, 3, e203593. [Google Scholar] [CrossRef] [PubMed]
- Hanigan, S.; Das, J.; Pogue, K.; Barnes, G.D.; Dorsch, M.P. The real world use of combined P-glycoprotein and moderate CYP3A4 inhibitors with rivaroxaban or apixaban increases bleeding. J. Thromb. Thrombolysis 2020, 49, 636–643. [Google Scholar] [CrossRef] [PubMed]
- Spada, G.; Vighi, G.; Pagani, S.; Venegoni, M.; Ruocco, M. What are the Characteristics of Patients Experiencing Adverse Drug Reactions to Oral Anticogulants and How Can Such Reactions be Prevented? Curr. Drug Saf. 2019, 15, 38–44. [Google Scholar] [CrossRef]
- Jiménez-Serranía, M.-I.; Martínez-García, R.; Corzo-Delibes, F.; Arias, L.H.M.; Treceño-Lobato, C. New Anticoagulant Agents: Incidence of Adverse Drug Reactions and New Signals Thereof. Semin. Thromb. Hemost. 2018, 45, 196–204. [Google Scholar] [CrossRef]
- Sasson, E.; James, M.; Russell, M.; Todorov, D.; Cohen, H. Probable Rivaroxaban-Induced Full Body Rash: A Case Report. J. Pharm. Pract. 2018, 31, 503–506. [Google Scholar] [CrossRef]
- Villines, T.C.; Peacock, W.F. Safety of Direct Oral Anticoagulants: Insights from Postmarketing Studies. Am. J. Med. 2016, 129, S41–S46. [Google Scholar] [CrossRef][Green Version]
- Di Minno, A.; Frigerio, B.; Spadarella, G.; Ravani, A.; Sansaro, D.; Amato, M.; Kitzmiller, J.P.; Pepi, M.; Tremoli, E.; Baldassarre, D. Old and new oral anticoagulants: Food, herbal medicines and drug interactions. Blood Rev. 2017, 31, 193–203. [Google Scholar] [CrossRef]
- To, K.; Reynolds, C.; Spinler, S.A. Rash Associated with Dabigatran Etexilate. Pharmacother. J. Hum. Pharmacol. Drug Ther. 2013, 33, e23–e27. [Google Scholar] [CrossRef] [PubMed]
- Heidbuchel, H.; Verhamme, P.; Alings, M.; Antz, M.; Diener, H.-C.; Hacke, W.; Oldgren, J.; Sinnaeve, P.; Camm, A.J.; Kirchhof, P. Updated European Heart Rhythm Association practical guide on the use of non-vitamin-K antagonist anticoagulants in patients with non-valvular atrial fibrillation: Executive summary. Eur. Heart J. 2016, 38, ehw058. [Google Scholar] [CrossRef] [PubMed]
- Sartori, M.T.; Danesin, C.; Saggiorato, G.; Tormene, D.; Simioni, P.; Spiezia, L.; Patrassi, G.M.; Girolami, A. The PAI-I gene 4G/5G Polymorphism and Deep Vein Thrombosis in Patients with Inherited Thrombophilia. Clin. Appl. Thromb. Hemost. 2003, 9, 299–307. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Silva, D.; Malone, M.V.; Seetharaman, K. MTHFR A1298C and C677T Polymorphisms Are Associated with Increased Risk of Venous Thromboembolism: A Retrospective Chart Review Study. Acta Haematol. 2017, 138, 208–215. [Google Scholar] [CrossRef]
- FDAble: Search FDA MedWatch FAERS AERS Database n.d. Available online: http://www.fdable.com/advanced_aers_query/1445e394afeb6dabbb44e5d2f2e98635 (accessed on 4 April 2022).
- Veliyev, V.; Özmen, İ.; Yaşar, S.; Gürsoy, E.; Köklü, M.; Çelik, M. A rare side effect seen due to the use of apixaban: Palmoplantar psoriasiform drug eruption. Anatol. J. Cardiol. 2016, 16, 213–215. [Google Scholar] [CrossRef]
- Naranjo, C.A.; Busto, U.; Sellers, E.M.; Sandor, P.; Ruiz, I.; Roberts, E.A.; Janecek, E.; Domecq, C.; Greenblatt, D.J. A method for estimating the probability of adverse drug reactions. Clin. Pharmacol. Ther. 1981, 30, 239–245. [Google Scholar] [CrossRef]
- The Use of the WHO-UMC System for Standardised Case Causality Assessment; World Health Organization (WHO)–Uppsala Monitoring Centre: Uppsala, Sweden, 2013.
- Gao, Y.; Jin, H. Livedoid vasculopathy and its association with genetic variants: A systematic review. Int. Wound J. 2021, 18, 616–625. [Google Scholar] [CrossRef]
- Byon, W.; Garonzik, S.; Boyd, R.A.; Frost, C.E. Apixaban: A Clinical Pharmacokinetic and Pharmacodynamic Review. Clin. Pharmacokinet. 2019, 58, 1265–1279. [Google Scholar] [CrossRef]
- Shnayder, N.; Petrova, M.; Shesternya, P.; Savinova, A.; Bochanova, E.; Zimnitskaya, O.; Pozhilenkova, E.; Nasyrova, R. Using Pharmacogenetics of Direct Oral Anticoagulants to Predict Changes in Their Pharmacokinetics and the Risk of Adverse Drug Reactions. Biomedicines 2021, 9, 451. [Google Scholar] [CrossRef]
- Wauthier, V.; Verbeeck, R.K.; Calderon, P.B. The effect of ageing on cytochrome p450 enzymes: Consequences for drug biotransformation in the elderly. Curr. Med. Chem. 2007, 14, 745–757. [Google Scholar] [CrossRef]
- Blech, S.; Ebner, T.; Ludwig-Schwellinger, E.; Stangier, J.; Roth, W. The Metabolism and Disposition of the Oral Direct Thrombin Inhibitor, Dabigatran, in Humans. Drug Metab. Dispos. 2008, 36, 386–399. [Google Scholar] [CrossRef] [PubMed]
- Horikiri, Y.; Suzuki, T.; Mizobe, M. Pharmacokinetics and Metabolism of Bisoprolol Enantiomers in Humans. J. Pharm. Sci. 1998, 87, 289–294. [Google Scholar] [CrossRef] [PubMed]
- Naritomi, Y.; Terashita, S.; Kagayama, A. Identification and relative contributions of human cytochrome P450 isoforms involved in the metabolism of glibenclamide and lansoprazole: Evaluation of an approach based on thein vitrosubstrate disappearance rate. Xenobiotica 2004, 34, 415–427. [Google Scholar] [CrossRef]
- Yang, K.H.; Choi, Y.H.; Lee, U.; Lee, M.G. Effects of cytochrome P450 inducers and inhibitors on the pharmacokinetics of intravenous furosemide in rats: Involvement of CYP2C11, 2E1, 3A1 and 3A2 in furosemide metabolism. J. Pharm. Pharmacol. 2008, 61, 47–54. [Google Scholar] [CrossRef]
- Tahara, K.; Kagawa, Y.; Takaai, M.; Taguchi, M.; Hashimoto, Y. Directional Transcellular Transport of Bisoprolol in P-glycoprotein-expressed LLC-GA5-COL150 Cells but not in Renal Epithelial LLC-PK1 Cells. Drug Metab. Pharmacokinet. 2008, 23, 340–346. [Google Scholar] [CrossRef] [PubMed]
- Nehaj, F.; Sokol, J.; Ivankova, J.; Mokan, M.; Mokan, M. Effect of Bisoprolol on the Level of Dabigatran. Am. J. Ther. 2020, 27, e159–e164. [Google Scholar] [CrossRef] [PubMed]
- Darvari, R.; Boroujerdi, M. Concentration dependency of modulatory effect of amlodipine on P-glycoprotein efflux activity of doxorubicin—A comparison with tamoxifen. J. Pharm. Pharmacol. 2010, 56, 985–991. [Google Scholar] [CrossRef] [PubMed]
- Katoh, M.; Nakajima, M.; Yamazaki, H.; Yokoi, T. Inhibitory potencies of 1,4-dihydropyridine calcium antagonists to P-glycoprotein-mediated transport: Comparison with the effects on CYP3A4. Pharm. Res. 2000, 17, 1189–1197. [Google Scholar] [CrossRef]
- Sychev, D.; Shikh, N.; Morozova, T.; Grishina, E.; Ryzhikova, K.; Malova, E. Effects of ABCB1 rs1045642 polymorphisms on the efficacy and safety of amlodipine therapy in Caucasian patients with stage I–II hypertension. Pharm. Pers. Med. 2018, 11, 157–165. [Google Scholar] [CrossRef]
- Hill, K.; Sucha, E.; Rhodes, E.; Bota, S.; Hundemer, G.L.; Clark, E.G.; Canney, M.; Harel, Z.; Wang, T.-F.; Carrier, M.; et al. Amiodarone, Verapamil, or Diltiazem Use With Direct Oral Anticoagulants and the Risk of Hemorrhage in Older Adults. CJC Open 2021, 4, 315–323. [Google Scholar] [CrossRef]
| Assessment Questions | Yes | No | Don’t Know |
|---|---|---|---|
| 1. Are there previous conclusive reports on the ADR? | +1 | 0 | 0 |
| 2. Did ADR appear after the suspected drug was given? | +2 | −1 | 0 |
| 3. Did the ADR improve when the drug was discontinued, or a specific antagonist was given? | +1 | 0 | 0 |
| 4. Did the ADR appear when the drug was re-administered? | +2 | -1 | 0 |
| 5. Are there alternative causes that could have caused the ADR? | −1 | +2 | 0 |
| 6. Did the reaction reappear when a placebo was given? | −1 | +1 | 0 |
| 7. Was the drug detected in any body fluid in toxic concentrations? | +1 | 0 | 0 |
| 8. Was the reaction more severe when the dose was increased, or less severe when the dose was decreased? | +1 | 0 | 0 |
| 9. Did the patient have a similar reaction to the same or similar drugs in any previous exposure? | +1 | 0 | 0 |
| 10. Was the ADR confirmed by any objective evidence? | +1 | 0 | 0 |
| Total Score | 6 = Probable | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Medoro, A.; Passarella, D.; Mignogna, D.; Porcile, C.; Foderà, E.; Intrieri, M.; Raimo, G.; La Floresta, P.; Russo, C.; Martucci, G. Cutaneous Ulcer Caused by Apixaban Treatment Is Resolved after Replacement with Dabigatran. Medicina 2022, 58, 691. https://doi.org/10.3390/medicina58050691
Medoro A, Passarella D, Mignogna D, Porcile C, Foderà E, Intrieri M, Raimo G, La Floresta P, Russo C, Martucci G. Cutaneous Ulcer Caused by Apixaban Treatment Is Resolved after Replacement with Dabigatran. Medicina. 2022; 58(5):691. https://doi.org/10.3390/medicina58050691
Chicago/Turabian StyleMedoro, Alessandro, Daniela Passarella, Donatella Mignogna, Carola Porcile, Emanuele Foderà, Mariano Intrieri, Gennaro Raimo, Pancrazio La Floresta, Claudio Russo, and Gennaro Martucci. 2022. "Cutaneous Ulcer Caused by Apixaban Treatment Is Resolved after Replacement with Dabigatran" Medicina 58, no. 5: 691. https://doi.org/10.3390/medicina58050691
APA StyleMedoro, A., Passarella, D., Mignogna, D., Porcile, C., Foderà, E., Intrieri, M., Raimo, G., La Floresta, P., Russo, C., & Martucci, G. (2022). Cutaneous Ulcer Caused by Apixaban Treatment Is Resolved after Replacement with Dabigatran. Medicina, 58(5), 691. https://doi.org/10.3390/medicina58050691







