Postoperative Rehabilitation Protocol Following Arthroscopic Rotator Cuff Repair: A Prospective Single-Arm Pragmatic Interventional Study
Abstract
:1. Introduction
2. Materials and Methods
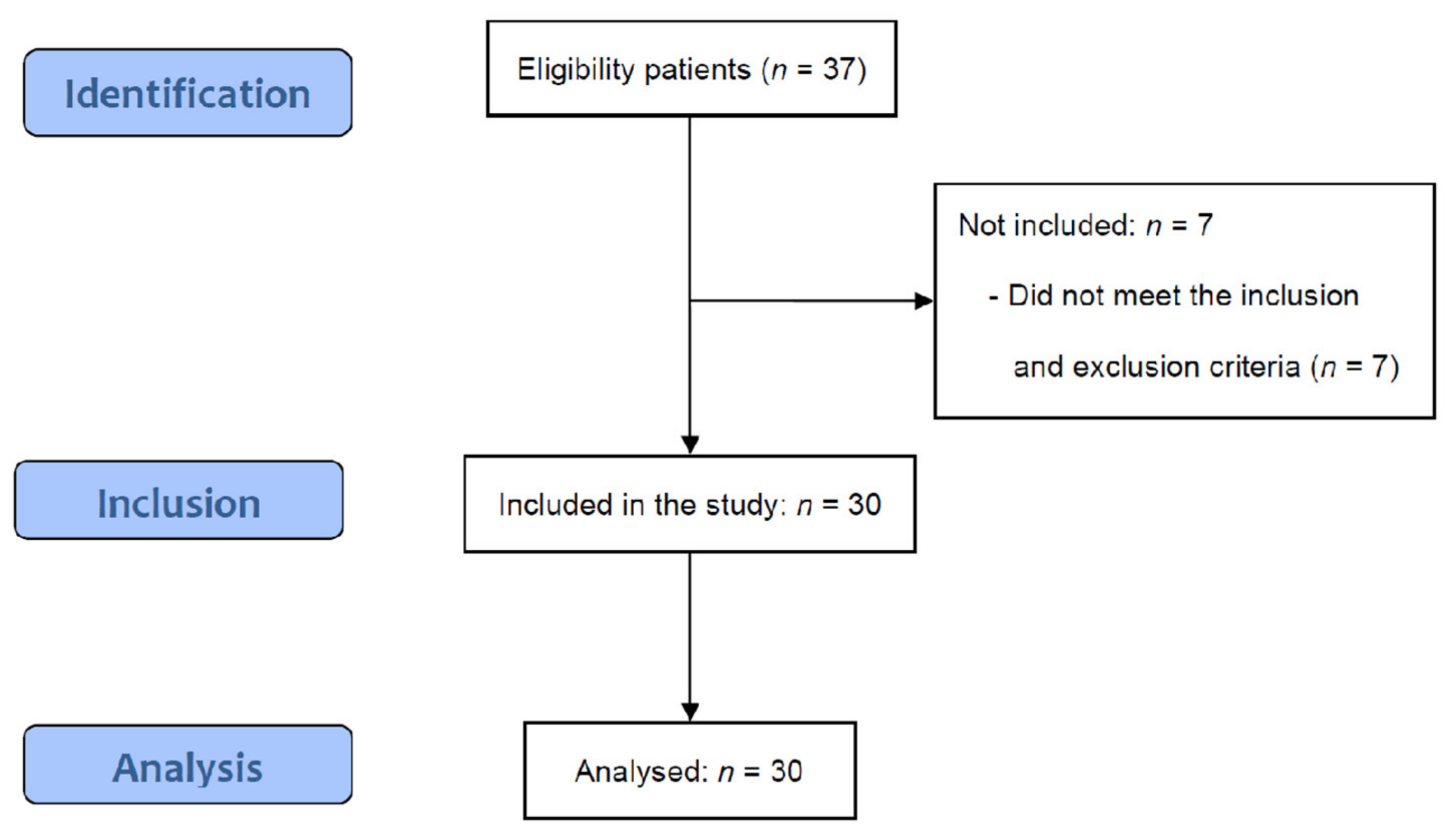
2.1. Study Design
2.2. Participants and Ethics
2.3. Sample Size
2.4. Postoperative Operative Rehabilitation Protocol
2.4.1. Physical Agents
2.4.2. Manual Therapy
2.4.3. Exercise
2.5. Outcomes
2.5.1. Primary Outcome Measures
2.5.2. Secondary Outcome Measures
2.6. Data Analysis
3. Results
3.1. Characteristics of the Enrolled Participants
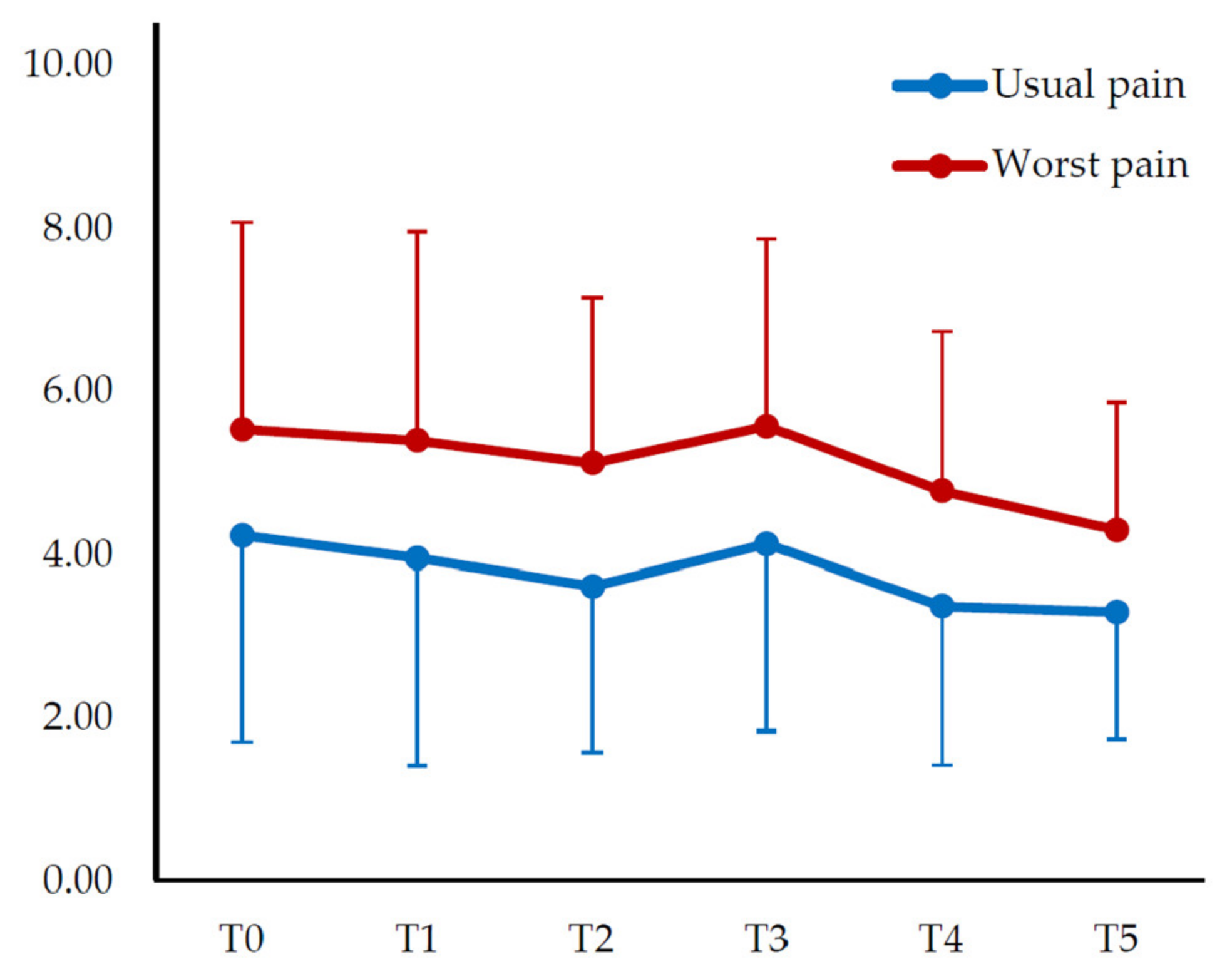
3.2. Change in Pain Intensity
3.3. Change in Range of Motion
3.4. Change in Shoulder Function
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed consent statement
Data Availability Statement
Conflicts of Interest
References
- Sheps, D.M.; Silveira, A.; Beaupre, L.; Styles-Tripp, F.; Balyk, R.; Lalani, A.; Glasgow, R.; Bergman, J.; Bouliane, M. Early active motion versus sling immobilization after arthroscopic rotator cuff repair: A randomized controlled trial. Arthroscopy 2019, 35, 749–760. [Google Scholar] [CrossRef]
- Largacha, M.; Parsons, I., IV.; Campbell, B.; Titelman, R.M.; Smith, K.L.; Matsen, F., III. Deficits in shoulder function and general health associated with sixteen common shoulder diagnoses: A study of 2674 patients. J. Shoulder Elbow Surg. 2006, 15, 30–39. [Google Scholar] [CrossRef]
- Weber, S.; Chahal, J. Management of rotator cuff injuries. J. Am. Acad. Orthop. Surg. 2020, 28, e193–e201. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.-V.; Hung, C.-Y.; Han, D.-S.; Chen, W.-S.; Wang, T.-G.; Chien, K.-L. Early versus delayed passive range of motion exercise for arthroscopic rotator cuff repair: A meta-analysis of randomized controlled trials. Am. J. Sports Med. 2015, 43, 1265–1273. [Google Scholar] [CrossRef] [PubMed]
- Kawano, Y.; Matsumura, N.; Murai, A.; Tada, M.; Matsumoto, M.; Nakamura, M.; Nagura, T. Evaluation of the translation distance of the glenohumeral joint and the function of the rotator cuff on its translation: A cadaveric study. Arthroscopy 2018, 34, 1776–1784. [Google Scholar] [CrossRef] [PubMed]
- Longo, U.G.; Ambrogioni, L.R.; Berton, A.; Candela, V.; Carnevale, A.; Schena, E.; Gugliemelli, E.; Denaro, V. Physical therapy and precision rehabilitation in shoulder rotator cuff disease. Int. Orthop. 2020, 44, 893–903. [Google Scholar] [CrossRef] [PubMed]
- Glazier, R.H.; Dalby, D.M.; Badley, E.M.; Hawker, G.A.; Bell, M.J.; Buchbinder, R.; Lineker, S.C. Management of common musculoskeletal problems: Survey of Ontario primary care physicians. CMAJ 1998, 158, 1037–1040. [Google Scholar]
- Dickens, V.A.; Williams, J.L.; Bhamra, M.S. Role of physiotherapy in the treatment of subacromial impingement syndrome: A prospective study. Physiotherapy 2005, 91, 159–164. [Google Scholar] [CrossRef]
- Green, S.; Buchbinder, R.; Hetrick, S.E. Physiotherapy interventions for shoulder pain. Cochrane Database Syst. Rev. 2003, CD004258. [Google Scholar] [CrossRef]
- Haahr, J.; Østergaard, S.; Dalsgaard, J.; Norup, K.; Frost, P.; Lausen, S.; Holm, E.; Andersen, J. Exercises versus arthroscopic decompression in patients with subacromial impingement: A randomised, controlled study in 90 cases with a one year follow up. Ann. Rheum. Dis. 2005, 64, 760–764. [Google Scholar] [CrossRef] [Green Version]
- Berton, A.; De Salvatore, S.; Candela, V.; Cortina, G.; Lo Presti, D.; Massaroni, C.; Petrillo, S.; Denaro, V. Delayed Rehabilitation Protocol after Rotator Cuff Repair. Osteology 2021, 1, 29–38. [Google Scholar] [CrossRef]
- Lee, B.G.; Cho, N.S.; Rhee, Y.G. Effect of two rehabilitation protocols on range of motion and healing rates after arthroscopic rotator cuff repair: Aggressive versus limited early passive exercises. Arthroscopy 2012, 28, 34–42. [Google Scholar] [CrossRef]
- Kane, L.T.; Thakar, O.; Jamgochian, G.; Lazarus, M.D.; Abboud, J.A.; Namdari, S.; Horneff, J.G. The role of telehealth as a platform for postoperative visits following rotator cuff repair: A prospective, randomized controlled trial. J. Shoulder Elbow Surg. 2020, 29, 775–783. [Google Scholar] [CrossRef]
- Conti, M.; Garofalo, R.; Delle Rose, G.; Massazza, G.; Vinci, E.; Randelli, M.; Castagna, A. Post-operative rehabilitation after surgical repair of the rotator cuff. Musculoskelet. Surg. 2009, 93, 55–63. [Google Scholar] [CrossRef]
- Van Der Meijden, O.A.; Westgard, P.; Chandler, Z.; Gaskill, T.R.; Kokmeyer, D.; Millett, P.J. Rehabilitation after arthroscopic rotator cuff repair: Current concepts review and evidence-based guidelines. Int. J. Sports Phys. Ther. 2012, 7, 197. [Google Scholar]
- Jung, C.; Tepohl, L.; Tholen, R.; Beitzel, K.; Buchmann, S.; Gottfried, T.; Grim, C.; Mauch, B.; Krischak, G.; Ortmann, H.; et al. Rehabilitation following rotator cuff repair. Obere Extrem. 2018, 13, 45–61. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.-J.; Lee, S. Physical Therapy Following Arthroscopic Rotator Cuff Repair with Graft Augmentation: A Case Report with Magnetic Resonance Imaging. Phys. Ther. Rehabil. Sci. 2021, 10, 463–469. [Google Scholar] [CrossRef]
- Bellew, J.W.; Michlovitz, S.L.; Nolan, T.P., Jr. Michlovitz’s Modalities for Therapeutic Intervention; FA Davis: Philadelphia, PA, USA, 2016. [Google Scholar]
- Wang, G.; Xu, Y.-M.; Ye, D.-M.; Fu, T.-F.; Zou, Y.-Z.; Feng, X.-X.; Bai, Y.-H. Effects of different doses of microwave therapy on adjacent tissue of titanium alloy implants after fracture surgery. Chin. J. Tissue Eng. Res. 2018, 22, 1072. [Google Scholar]
- Johnson, M. Transcutaneous electrical nerve stimulation: Mechanisms, clinical application and evidence. Rev. Pain 2007, 1, 7–11. [Google Scholar] [CrossRef]
- Senbursa, G.; Baltacı, G.; Atay, A. Comparison of conservative treatment with and without manual physical therapy for patients with shoulder impingement syndrome: A prospective, randomized clinical trial. Knee Surg. Sports Traumatol. Arthrosc. 2007, 15, 915–921. [Google Scholar] [CrossRef]
- Desjardins-Charbonneau, A.; Roy, J.-S.; Dionne, C.E.; Frémont, P.; MacDermid, J.C.; Desmeules, F. The efficacy of manual therapy for rotator cuff tendinopathy: A systematic review and meta-analysis. J. Orthop. Sports Phys. Ther. 2015, 45, 330–350. [Google Scholar] [CrossRef]
- Rodriguez-Santiago, B.; Castillo, B.; Baerga-Varela, L.; Micheo, W.F. Rehabilitation management of rotator cuff injuries in the master athlete. Curr. Sports Med. Rep. 2019, 18, 330–337. [Google Scholar] [CrossRef]
- Almasoodi, M.C.I.; Mahdavinejad, R.; Ghasmi, G. The Effect of 8 Weeks National Academy of Sports Medicine Exercises Training on Posture, Shoulder Pain, and Functional Disability in Male with Upper Cross Syndrome. Syst. Rev. Pharm. 2020, 11, 1826–1833. [Google Scholar]
- De Mey, K.; Danneels, L.; Cagnie, B.; Huyghe, L.; Seyns, E.; Cools, A.M. Conscious correction of scapular orientation in overhead athletes performing selected shoulder rehabilitation exercises: The effect on trapezius muscle activation measured by surface electromyography. J. Orthop. Sports Phys. Ther. 2013, 43, 3–10. [Google Scholar] [CrossRef] [Green Version]
- Hotta, G.H.; Santos, A.L.; McQuade, K.J.; de Oliveira, A.S. Scapular-focused exercise treatment protocol for shoulder impingement symptoms: Three-dimensional scapular kinematics analysis. Clin. Biomech. 2018, 51, 76–81. [Google Scholar] [CrossRef]
- Michener, L.A.; Snyder, A.R.; Leggin, B.G. Responsiveness of the numeric pain rating scale in patients with shoulder pain and the effect of surgical status. J. Sport Rehabil. 2011, 20, 115–128. [Google Scholar] [CrossRef]
- Mintken, P.E.; Glynn, P.; Cleland, J.A. Psychometric properties of the shortened disabilities of the Arm, Shoulder, and Hand Questionnaire (QuickDASH) and Numeric Pain Rating Scale in patients with shoulder pain. J. Shoulder Elbow Surg. 2009, 18, 920–926. [Google Scholar] [CrossRef]
- Mullaney, M.J.; McHugh, M.P.; Johnson, C.P.; Tyler, T.F. Reliability of shoulder range of motion comparing a goniometer to a digital level. Physiother. Theory Pract. 2010, 26, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Dabija, D.I.; Jain, N.B. Minimal clinically important difference of shoulder outcome measures and diagnoses: A systematic review. Am. J. Phys. Med. Rehabil. 2019, 98, 671. [Google Scholar] [CrossRef]
- Schmitt, J.S.; Di Fabio, R.P. Reliable change and minimum important difference (MID) proportions facilitated group responsiveness comparisons using individual threshold criteria. J. Clin. Epidemiol. 2004, 57, 1008–1018. [Google Scholar] [CrossRef]
- Tashjian, R.Z.; Deloach, J.; Green, A.; Porucznik, C.A.; Powell, A.P. Minimal clinically important differences in ASES and simple shoulder test scores after nonoperative treatment of rotator cuff disease. J. Bone Joint Surg. Am. 2010, 92, 296–303. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge: Abingdon, UK, 1988. [Google Scholar]
- Cohen, J. Quantitative methods in psychology: A power primer. Psychol. Bull. 1992, 112, 153–159. [Google Scholar] [CrossRef]
- Kim, K.C.; Shin, H.D.; Lee, W.-Y.; Yeon, K.-W.; Han, S.-C. Clinical outcomes and repair integrity of arthroscopic rotator cuff repair using suture-bridge technique with or without medial tying: Prospective comparative study. J. Orthop. Surg. Res. 2018, 13, 212. [Google Scholar] [CrossRef] [Green Version]
- Millett, P.J.; Mazzocca, A.; Guanche, C.A. Mattress double anchor footprint repair: A novel, arthroscopic rotator cuff repair technique. Arthroscopy 2004, 20, 875–879. [Google Scholar] [CrossRef]
- Duzgun, I.; Baltaci, G.; Atay, O. Comparison of slow and accelerated rehabilitation protocol after arthroscopic rotator cuff repair: Pain and functional activity. Acta Orthop. Traumatol. Turc. 2011, 45, 23–33. [Google Scholar] [CrossRef]
- Ha, J.-W.; Kim, H.; Kim, S.H. Effects of steroid injection during rehabilitation after arthroscopic rotator cuff repair. Clin. Shoulder Elb. 2021, 24, 166. [Google Scholar] [CrossRef]
- Sgroi, T.A.; Cilenti, M. Rotator cuff repair: Post-operative rehabilitation concepts. Curr. Rev. Musculoskelet. Med. 2018, 11, 86–91. [Google Scholar] [CrossRef] [Green Version]
- Milano, G.; Grasso, A.; Salvatore, M.; Zarelli, D.; Deriu, L.; Fabbriciani, C. Arthroscopic rotator cuff repair with and without subacromial decompression: A prospective randomized study. Arthroscopy 2007, 23, 81–88. [Google Scholar] [CrossRef]

| Types | Component | Description | Dosage |
|---|---|---|---|
| Physical agents | Superficial heat therapy | In side-lying position, using infrared radiation | 15 min per session 5 sessions per week |
| Microwave therapy | In side-lying position, using biowave, at a distance of 20 cm | 5 min per session 5 sessions per week | |
| TENS | In side-lying position, automatic modulation intense TENS of 100–300 Hz | 15 min per session 5 sessions per week | |
| Manual therapy | Soft tissue mobilization | Upper extremity and periscapular regions, in supine and side-lying positions, respectively | 20 min per session 5 sessions per week |
| Joint mobilization | Glenohumeral joint, scapular, and thoracic spine, in supine and side-lying positions, respectively | 10 min per session 5 sessions per week | |
| Exercises | Maximal protection phase; Wearing shoulder abduction sling (POD 2-week to 4-week) | ||
| ROM exercise | CPM: In a sitting position, the instrument was set to a scaption of 180° flexion to 20° of extension Active assisted ROM exercise: ROM exercise with correct movement under supervision | 30 min per session 5 sessions per week | |
| Therapeutic exercise | Active exercise of the elbow and wrist, scapular conscious exercise, scapular setting exercise | 20 min per session 5 sessions per week | |
| Minimal protection active phase (POD 4-week to 8-week) | |||
| ROM exercise | CPM: In a sitting position, the instrument was set to a scaption of 180° flexion to 20° of extension Active ROM exercise: ROM exercise with correct movement under supervision | 30 min per session 5 sessions per week | |
| Therapeutic exercise | Scapular stabilization exercise, pectoralis and periscapular muscle stretching exercise (mild to moderate) | 20 min per session 5 sessions per week | |
| Variables (n = 30) | Mean ± SD |
|---|---|
| Sex (male, %) | 11 (36.67) |
| Affected side (left,%) | 9 (30.00) |
| Age (years) | 51.86 ± 4.76 |
| Height (cm) | 161.47 ± 6.06 |
| Weight (kg) | 63.20 ± 8.74 |
| Body mass index (kg/m2) | 23.78 ± 2.12 |
| Arthroscopic rotator cuff repair | |
| Supraspinatus repair (n) | 14 |
| Subscapularis repair (n) | 20 |
| Capsular release (n) | 14 |
| Biceps tenodesis (n) | 24 |
| Subacromial decompression (n) | 30 |
| Variables (n = 30) | T0 POD 2-Week | T1 POD 4-Week | T2 POD 6-Week | T3 POD 8-Week | T4 POD 10-Week | T5 POD 12-Week | Time F (p) (a) | Effect Size (b) |
|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | |||
| Pain intensity | ||||||||
| Usual pain | 4.24 ± 1.55 | 3.97 ± 1.59 | 3.62 ± 1.86 | 4.14 ± 1.90 | 3.38 ± 1.88 | 3.31 ± 1.73 | 3.731 (0.013) | 0.114 |
| Worst pain | 5.55 ± 2.53 | 5.41 ± 2.54 | 5.14 ± 2.03 | 5.59 ± 2.29 | 4.79 ± 1.95 | 4.31 ± 1.56 | 3.572 (0.011) | 0.110 |
| Shoulder function | ||||||||
| DASH | 77.82 ± 19.51 | 72.18 ± 17.78 | 61.15 ± 16.33 *** | 61.12 ± 17.90 *** | 56.98 ± 16.58 *** | 55.37 ± 17.69 *** | 26.636 (0.000) | 0.479 |
| SPAD-pain | 68.69 ± 22.94 | 60.69 ± 27.20 | 54.14 ± 23.46 ** | 52.76 ± 24.37 ** | 45.38 ± 23.71 *** | 39.93 ± 23.49 *** | 22.166 (0.000) | 0.433 |
| SPADI-disability | 63.02 ± 23.09 | 54.87 ± 28.16 | 43.41 ± 23.26 *** | 41.16 ± 25.34 *** | 34.83 ± 22.83 *** | 34.79 ± 25.39 *** | 20.770 (0.000) | 0.417 |
| SPADI-total | 65.10 ± 22.65 | 57.11 ± 27.53 | 47.53 ± 22.01 *** | 45.62 ± 24.22 *** | 38.89 ± 22.77 *** | 36.81 ± 23.77 *** | 24.900 (0.000) | 0.462 |
| SST | 9.72 ± 2.96 | 8.55 ± 1.99 | 6.90 ± 1.68 *** | 7.34 ± 3.05 * | 5.48 ± 2.44 *** | 5.17 ± 2.28 *** | 23.801 (0.000) | 0.451 |
| Variables (n = 30) | T1 | T3 | Z | p(a) | Effect Size (b) |
|---|---|---|---|---|---|
| Median | Median | ||||
| Flexion | 162.50 | 180.00 | −4.061 | 0.000 | 1.167 |
| Scaption flexion | 130.00 | 180.00 | −4.013 | 0.000 | 1.355 |
| Abduction | 120.00 | 180.00 | −3.449 | 0.001 | 0.907 |
| Horizontala | 110.00 | 130.00 | −3.432 | 0.001 | 0.766 |
| External rotation | 60.00 | 80.00 | −4.183 | 0.000 | 1.005 |
| Internal rotation | 50.00 | 50.00 | −3.204 | 0.001 | 0.506 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.; Lee, S. Postoperative Rehabilitation Protocol Following Arthroscopic Rotator Cuff Repair: A Prospective Single-Arm Pragmatic Interventional Study. Medicina 2022, 58, 729. https://doi.org/10.3390/medicina58060729
Kim H, Lee S. Postoperative Rehabilitation Protocol Following Arthroscopic Rotator Cuff Repair: A Prospective Single-Arm Pragmatic Interventional Study. Medicina. 2022; 58(6):729. https://doi.org/10.3390/medicina58060729
Chicago/Turabian StyleKim, Hyunjoong, and Seungwon Lee. 2022. "Postoperative Rehabilitation Protocol Following Arthroscopic Rotator Cuff Repair: A Prospective Single-Arm Pragmatic Interventional Study" Medicina 58, no. 6: 729. https://doi.org/10.3390/medicina58060729
APA StyleKim, H., & Lee, S. (2022). Postoperative Rehabilitation Protocol Following Arthroscopic Rotator Cuff Repair: A Prospective Single-Arm Pragmatic Interventional Study. Medicina, 58(6), 729. https://doi.org/10.3390/medicina58060729







