Impact of Short Sleep Duration on the Incidence of Obesity and Overweight among Children and Adolescents
Abstract
:1. Introduction
2. Materials and Methods
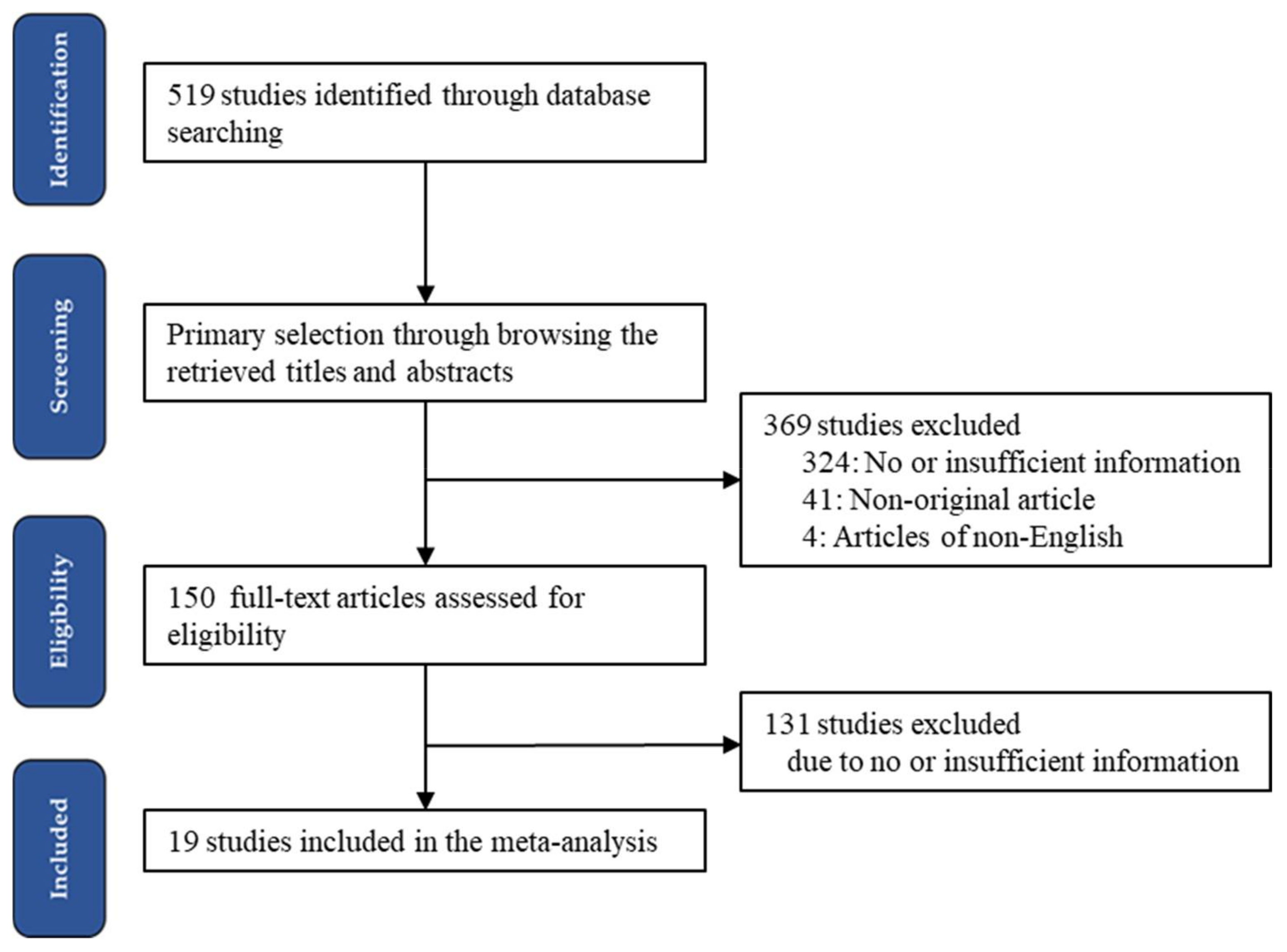
2.1. Literature Search and Study Selection Criteria
2.2. Data Extraction
2.3. Statistical Analyses
3. Results
3.1. Selection and Characteristics of the Included Studies
3.2. Estimated Risks for Obesity and Overweight According to Short Sleep Duration
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- World Health Organization. Facts and Figures on Childhood Obesity. Available online: http://www.who.int/end-childhood-obesity/facts/en/ (accessed on 12 November 2021).
- Wang, G.; Dietz, W.H. Economic Burden of Obesity in Youths Aged 6 to 17 Years: 1979–1999. Pediatrics 2002, 109, e81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, Z.; Han, S.; Chu, J.; Xu, Z.; Zhu, C.; Guo, X. Trends in Overweight and Obesity among Children and Adolescents in China from 1981 to 2010: A Meta-Analysis. PLoS ONE 2012, 7, e51949. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Umer, A.; Kelley, G.A.; Cottrell, L.E.; Giacobbi, P., Jr.; Innes, K.E.; Lilly, C.L. Childhood obesity and adult cardiovascular disease risk factors: A systematic review with meta-analysis. BMC Public Health 2017, 17, 683. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paruthi, S.; Brooks, L.J.; D’Ambrosio, C.; Hall, W.; Kotagal, S.; Lloyd, R.M.; Malow, B.A.; Maski, K.; Nichols, C.; Quan, S.F.; et al. Consensus Statement of the American Academy of Sleep Medicine on the Recommended Amount of Sleep for Healthy Children: Methodology and Discussion. J. Clin. Sleep Med. 2016, 12, 1549–1561. [Google Scholar] [CrossRef]
- Wheaton, A.G.; Jones, S.E.; Cooper, A.C.; Croft, J.B. Short Sleep Duration Among Middle School and High School Students—United States, 2015. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 85–90. [Google Scholar] [CrossRef] [Green Version]
- Song, Y.; Zhang, B.; Hu, P.; Ma, J. Current situation of sleeping duration in Chinese Han students in 2010. Zhonghua Yu Fang Yi Xue Za Zhi [Chin. J. Prev. Med.] 2014, 48, 596–601. [Google Scholar]
- Owens, J.; Adolescent Sleep Working Group; Committee on Adolescence. Insufficient sleep in adolescents and young adults: An update on causes and consequences. Pediatrics 2014, 134, e921–e932. [Google Scholar] [CrossRef] [Green Version]
- Lowry, R.; Eaton, D.K.; Foti, K.; McKnight-Eily, L.; Perry, G.; Galuska, D.A. Association of Sleep Duration with Obesity among US High School Students. J. Obes. 2012, 2012, 476914. [Google Scholar] [CrossRef]
- Fitzgerald, C.T.; Messias, E.; Buysse, D.J. Teen Sleep and Suicidality: Results from the Youth Risk Behavior Surveys of 2007 and 2009. J. Clin. Sleep Med. 2011, 7, 351–356. [Google Scholar] [CrossRef]
- Ford, E.S.; Li, C.; Wheaton, A.G.; Chapman, D.P.; Perry, G.S.; Croft, J.B. Sleep duration and body mass index and waist circumference among U.S. adults. Obesity 2014, 22, 598–607. [Google Scholar] [CrossRef] [Green Version]
- Cho, K.-H.; Cho, E.-H.; Hur, J.; Shin, D. Association of Sleep Duration and Obesity According to Gender and Age in Korean Adults: Results from the Korea National Health and Nutrition Examination Survey 2007–2015. J. Korean Med. Sci. 2018, 33, e345. [Google Scholar] [CrossRef]
- Garaulet, M.; Ortega, F.B.; Ruiz, J.R.; Rey-López, J.P.; Béghin, L.; Manios, Y.; Cuenca-García, M.; Plada, M.; Diethelm, K.; Kafatos, A.; et al. Short sleep duration is associated with increased obesity markers in European adolescents: Effect of physical activity and dietary habits. The HELENA study. Int. J. Obes. 2011, 35, 1308–1317. [Google Scholar] [CrossRef] [Green Version]
- Ames, M.E.; Holfeld, B.; Leadbeater, B.J. Sex and age group differences in the associations between sleep duration and BMI from adolescence to young adulthood. Psychol. Health 2016, 31, 976–992. [Google Scholar] [CrossRef]
- Gong, Q.-H.; Li, S.-X.; Wang, S.-J.; Wu, Y.-H.; Han, L.-Y.; Li, H. Sleep duration and overweight in Chinese adolescents: A prospective longitudinal study with 2-year follow-up. Sleep Breath. 2020, 24, 321–328. [Google Scholar] [CrossRef]
- Mercado-Gonzales, S.I.; Carpio-Rodríguez, A.N.; Carrillo-Larco, R.M.; Bernabé-Ortiz, A. Sleep Duration and Risk of Obesity by Sex: Nine-Year Follow-Up of the Young Lives Study in Peru. Child. Obes. 2019, 15, 237–243. [Google Scholar] [CrossRef] [Green Version]
- Anujuo, K.O.; Vrijkotte, T.G.; Stronks, K.; Jean-Louis, G.; Agyemang, C.O. Ethnic differences in sleep duration at 5 years, and its relationship with overweight and blood pressure. Eur. J. Public Health 2016, 26, 1001–1006. [Google Scholar] [CrossRef] [Green Version]
- Azadbakht, L.; Kelishadi, R.; Khodarahmi, M.; Qorbani, M.; Heshmat, R.; Motlagh, M.E.; Taslimi, M.; Ardalan, G. The association of sleep duration and cardiometabolic risk factors in a national sample of children and adolescents: The CASPIAN III Study. Nutrition 2013, 29, 1133–1141. [Google Scholar] [CrossRef]
- Breitenstein, R.S.; Doane, L.D.; Lemery-Chalfant, K. Early life socioeconomic status moderates associations between objective sleep and weight-related indicators in middle childhood. Sleep Health 2019, 5, 470–478. [Google Scholar] [CrossRef]
- Calamaro, C.J.; Park, S.; Mason, T.B.A.; Marcus, C.L.; Weaver, T.E.; Pack, A.; Ratcliffe, S.J. Shortened sleep duration does not predict obesity in adolescents. J. Sleep Res. 2010, 19, 559–566. [Google Scholar] [CrossRef] [Green Version]
- Cao, M.; Zhu, Y.; Li, X.; Chen, Y.; Ma, J.; Jing, J. Gender-dependent association between sleep duration and overweight incidence in CHINESE school children: A national follow-up study. BMC Public Health 2018, 18, 615. [Google Scholar] [CrossRef] [Green Version]
- Carrillo-Larco, R.M.; Bernabé-Ortiz, A.; Miranda, J.J. Short Sleep Duration and Childhood Obesity: Cross-Sectional Analysis in Peru and Patterns in Four Developing Countries. PLoS ONE 2014, 9, e112433. [Google Scholar] [CrossRef] [Green Version]
- Chaput, J.-P.; Brunet, M.; Tremblay, A. Relationship between short sleeping hours and childhood overweight/obesity: Results from the ‘Québec en Forme’ Project. Int. J. Obes. 2006, 30, 1080–1085. [Google Scholar] [CrossRef] [Green Version]
- Chaput, J.-P.; Lambert, M.; Gray-Donald, K.; McGrath, J.; Tremblay, M.S.; O’Loughlin, J.; Tremblay, A. Short Sleep Duration Is Independently Associated with Overweight and Obesity in Quebec Children. Can. J. Public Health 2011, 102, 369–374. [Google Scholar] [CrossRef]
- Ievers-Landis, C.E.; Storfer-Isser, A.; Rosen, C.; Johnson, N.L.; Redline, S. Relationship of Sleep Parameters, Child Psychological Functioning, and Parenting Stress to Obesity Status Among Preadolescent Children. J. Dev. Behav. Pediatr. 2008, 29, 243–252. [Google Scholar] [CrossRef]
- Malihi, Z.; Portch, R.; Hashemi, L.; Schlichting, D.; Wake, M.; Morton, S.; Fa’Alili-Fidow, J.; Mensah, F.; Olds, T.; Carr, P.A.; et al. Modifiable Early Childhood Risk Factors for Obesity at Age Four Years. Child. Obes. 2021, 17, 196–208. [Google Scholar] [CrossRef]
- Suglia, S.F.; Duarte, C.S.; Chambers, E.C.; Boynton-Jarrett, R. Social and Behavioral Risk Factors for Obesity in Early Childhood. J. Dev. Behav. Pediatr. 2013, 34, 549–556. [Google Scholar] [CrossRef] [Green Version]
- Suglia, S.F.; Kara, S.; Robinson, W.R. Sleep Duration and Obesity among Adolescents Transitioning to Adulthood: Do Results Differ by Sex? J. Pediatr. 2014, 165, 750–754. [Google Scholar] [CrossRef] [Green Version]
- Sun, Y.; Sekine, M.; Kagamimori, S. Lifestyle and Overweight Among Japanese Adolescents: The Toyama Birth Cohort Study. J. Epidemiol. 2009, 19, 303–310. [Google Scholar] [CrossRef] [Green Version]
- Touchette, E.; Petit, D.; Tremblay, R.E.; Boivin, M.; Falissard, B.; Genolini, C.; Montplaisir, J.Y. Associations Between Sleep Duration Patterns and Overweight/Obesity at Age 6. Sleep 2008, 31, 1507–1514. [Google Scholar] [CrossRef] [Green Version]
- Wang, F.; Liu, H.; Wan, Y.; Li, J.; Chen, Y.; Zheng, J.; Huang, T.; Li, D. Sleep Duration and Overweight/Obesity in Preschool-Aged Children: A Prospective Study of up to 48,922 Children of the Jiaxing Birth Cohort. Sleep 2016, 39, 2013–2019. [Google Scholar] [CrossRef] [Green Version]
- Wang, J.; Li, A.M.; Lam, H.S.; Leung, G.M.; Schooling, C.M. Sleep Duration and Adiposity in Children and Adults: Observational and Mendelian Randomization Studies. Obesity 2019, 27, 1013–1022. [Google Scholar] [CrossRef] [PubMed]
- Wing, Y.K.; Li, S.X.; Li, A.M.; Zhang, J.; Kong, A.P.S. The Effect of Weekend and Holiday Sleep Compensation on Childhood Overweight and Obesity. Pediatrics 2009, 124, e994–e1000. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Miller, M.A.; Cappuccio, F.P. Short duration of sleep and incidence of overweight or obesity in Chinese children and adolescents: A systematic review and meta-analysis of prospective studies. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 363–371. [Google Scholar] [CrossRef] [PubMed]
- Eisenmann, J.C.; Ekkekakis, P.; Holmes, M. Sleep duration and overweight among Australian children and adolescents. Acta Paediatr. 2006, 95, 956–963. [Google Scholar] [CrossRef]
- Cao, M.; Zhu, Y.; He, B.; Yang, W.; Chen, Y.; Ma, J.; Jing, J. Association between sleep duration and obesity is age- and gender-dependent in Chinese urban children aged 6–18 years: A cross-sectional study. BMC Public Health 2015, 15, 1029. [Google Scholar] [CrossRef] [Green Version]
- Taheri, S.; Lin, L.; Austin, D.; Young, T.; Mignot, E. Short Sleep Duration Is Associated with Reduced Leptin, Elevated Ghrelin, and Increased Body Mass Index. PLoS Med. 2004, 1, 210–217. [Google Scholar] [CrossRef]
- Chaput, J.-P.; Després, J.-P.; Bouchard, C.; Tremblay, A. Short Sleep Duration is Associated with Reduced Leptin Levels and Increased Adiposity: Results from the Québec Family Study. Obesity 2007, 15, 253–261. [Google Scholar] [CrossRef]
- Chaput, J.-P.; Després, J.-P.; Bouchard, C.; Tremblay, A. The Association Between Sleep Duration and Weight Gain in Adults: A 6-Year Prospective Study from the Quebec Family Study. Sleep 2008, 31, 517–523. [Google Scholar] [CrossRef] [Green Version]
- Santos, R.; Tufik, S.; De Mello, M. Exercise, sleep and cytokines: Is there a relation? Sleep Med. Rev. 2007, 11, 231–239. [Google Scholar] [CrossRef]
- Deng, X.; He, M.; He, D.; Zhu, Y.; Zhang, Z.; Niu, W. Sleep duration and obesity in children and adolescents: Evidence from an updated and dose–response meta-analysis. Sleep Med. 2021, 78, 169–181. [Google Scholar] [CrossRef]

| First Author | Location | No of Patients | Age Group | Parameter | Comparison | Reference |
|---|---|---|---|---|---|---|
| Anujuo 2016 | Various | 2384 | 5 yrs | OS/OW | <10 h | >10 h |
| Azadbakht 2013 | Iran | 5528 | 10–18 yrs | OS, OW | <5 h | 5–8 h |
| 10–14 yrs | <5 h | >8 h | ||||
| Breitenstein 2019 | USA | 382 | 12–13 yrs | OS/OW | 8 h | ND |
| Calamaro 2010 | USA | 13,568 | 15.96 yrs | OS | <6 h | 8–11 h |
| 6–8 h | 8–11 h | |||||
| 8–11 h | 11–14 h | |||||
| Cao 2018 | China | 18,302 | 6–17 yrs | OW | <7 h | >9 h |
| 7–9 h | >9 h | |||||
| Carrillo-Larco 2014 | Various | 1929 | 7.9 yrs | OS, OW | <10 h | 10–11 h |
| Chaput 2006 | Canada | 422 | 5–10 yrs | OS/OW | 8–10 h | 12–13 h |
| 10.5–11.5 h | 12–13 h | |||||
| Chaput 2011 | USA | 550 | 9.6 yrs | OS/OW | <10 h | 11–11.9 h |
| 10–10.9 h | 11–11.9 h | |||||
| 11–11.9 h | >12 h | |||||
| Gong 2020 | China | 3411 | 12–13 yrs | OW | Short | ND |
| Ievers-Landis 2008 | USA | 819 | 9.5 yrs | OS | 1 h reduction | |
| Malihi 2021 | New Zealand | 5734 | 2 yrs | OS | <11.5 h | >11.5 h |
| Mercado-Gonzales 2019 | Various | 1945 | 4–5 yrs | OS | <10 h | 10–13 h |
| Suglia 2013 | USA | 1589 | 5 yrs | OS | <9 h | >9 h |
| Suglia 2014 | USA | 10,076 | 16 yrs | OS | <6 h | >8 h |
| 6–8 h | >8 h | |||||
| Sun 2009 | Japan | 5753 | 12–13 yrs | OW | <7 h | 8–9 h |
| 7–8 h | 8–9 h | |||||
| 8–9 h | >9 h | |||||
| Touchette 2008 | Canada | 2223 | 6 yrs | OS/OW | 10 h | 11 h |
| Wang 2016 | Singapore | 48,922 | 5 yrs | OS, OW | <10 h | 11–12 h |
| 11–12 h | >13 h | |||||
| Wang 2019 | Hong Kong | 3614 | 9–11 yrs | OS/OW | <9 h | >9 h |
| 11–16 yrs | <9 h | >9 h | ||||
| Wing 2009 | China | 5159 | 9.25 yrs | OS/OW | 9–10 h | >10 h |
| 8–9 h | >10 h | |||||
| <8 h | >10 h |
| Number of Subset | Fixed Effect (95% CI) | Heterogeneity Test (p-Value) | Random Effect (95% CI) | Egger’s Test | |
|---|---|---|---|---|---|
| Obesity/overweight | 54 | 1.169 [1.130, 1.210] | <0.001 | 1.171 [1.092, 1.256] | 0.832 |
| Obesity | 17 | 1.225 [1.146, 1.310] | 0.001 | 1.191 [1.055, 1.344] | 0.294 |
| Overweight | 19 | 1.118 [1.068, 1.171] | <0.001 | 1.098 [0.976, 1.234] | 0.669 |
| <6 years | 14 | 1.172 [1.119, 1.227] | <0.001 | 1.226 [1.083, 1.387] | 0.516 |
| 6–10 years | 9 | 1.341 [1.219, 1.474] | 0.093 | 1.341 [1.175, 1.530] | 0.771 |
| >10 years | 26 | 1.055 [0.980, 1.134] | <0.001 | 1.034 [0.904, 1.183] | 0.489 |
| North America | 14 | 1.191 [1.089, 1.302] | <0.001 | 1.161 [0.964, 1.398] | 0.587 |
| Asia | 30 | 1.158 [1.113, 1.206] | <0.001 | 1.161 [1.060, 1.271] | 0.817 |
| Number of Subset | Fixed Effect (95% CI) | Heterogeneity Test (p-Value) | Random Effect (95% CI) | Egger’s Test | |
|---|---|---|---|---|---|
| <10 h | |||||
| Obesity/overweight | 14 | 1.212 [1.156, 1.270] | 0.001 | 1.328 [1.185, 1.489] | 0.094 |
| Obesity | 3 | 1.274 [1.149, 1.413] | 0.040 | 1.304 [1.006, 1.690] | 0.879 |
| Overweight | 3 | 1.169 [1.106, 1.236] | 0.009 | 1.239 [1.042, 1.475] | 0.535 |
| <6 years | 11 | 1.205 [1.147, 1.266] | 0.001 | 1.326 [1.159, 1.518] | 0.221 |
| 6–10 years | 3 | 1.280 [1.095, 1.495] | 0.094 | 1.365 [1.042, 1.789] | 0.035 |
| >10 years | 0 | ||||
| North America | 2 | 1.966 [1.367, 2.826] | 0.591 | 1.966 [1.367, 2.826] | - |
| Asia | 5 | 1.203 [1.144, 1.265] | 0.002 | 1.325 [1.154, 1.520] | 0.038 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, S.-H.; Yee, J.-Y.; Pyo, J.-S. Impact of Short Sleep Duration on the Incidence of Obesity and Overweight among Children and Adolescents. Medicina 2022, 58, 1037. https://doi.org/10.3390/medicina58081037
Han S-H, Yee J-Y, Pyo J-S. Impact of Short Sleep Duration on the Incidence of Obesity and Overweight among Children and Adolescents. Medicina. 2022; 58(8):1037. https://doi.org/10.3390/medicina58081037
Chicago/Turabian StyleHan, Seung-Ho, Jae-Yong Yee, and Jung-Soo Pyo. 2022. "Impact of Short Sleep Duration on the Incidence of Obesity and Overweight among Children and Adolescents" Medicina 58, no. 8: 1037. https://doi.org/10.3390/medicina58081037
APA StyleHan, S.-H., Yee, J.-Y., & Pyo, J.-S. (2022). Impact of Short Sleep Duration on the Incidence of Obesity and Overweight among Children and Adolescents. Medicina, 58(8), 1037. https://doi.org/10.3390/medicina58081037







