Retro-Malleolar Z-Plasty of Flexor Hallucis Longus Tendon in Post-Traumatic Checkrein Deformity: A Case Series and Literature Review
Abstract
:1. Introduction
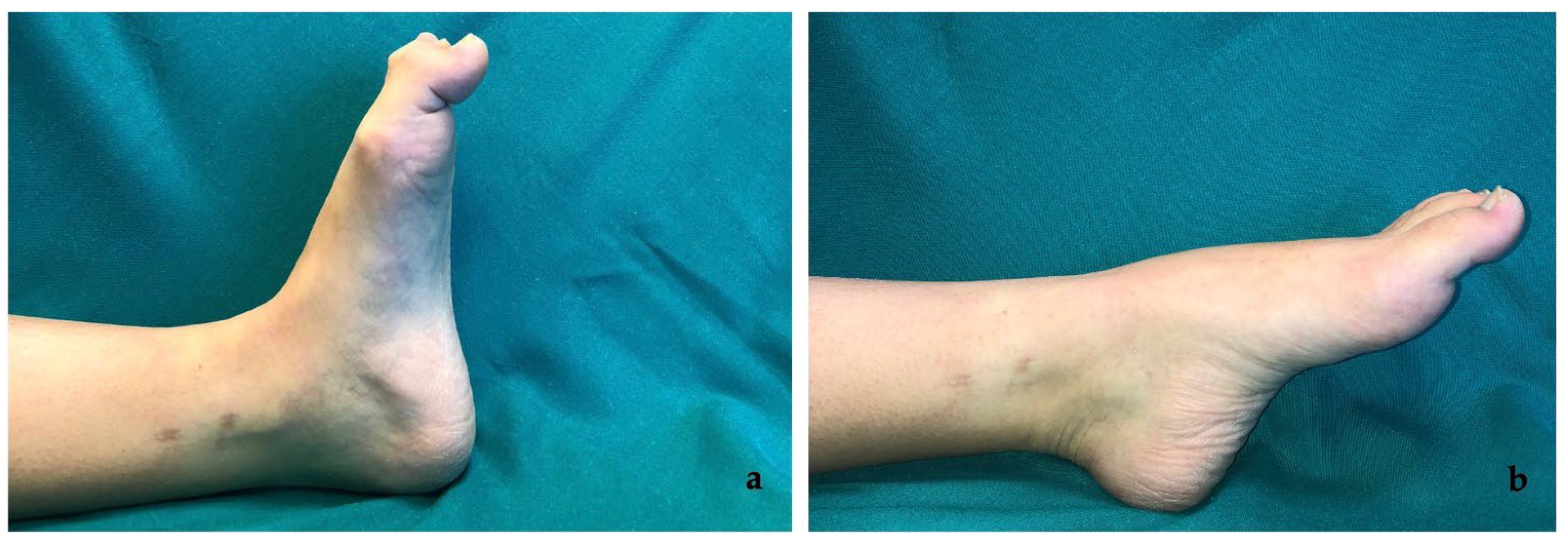
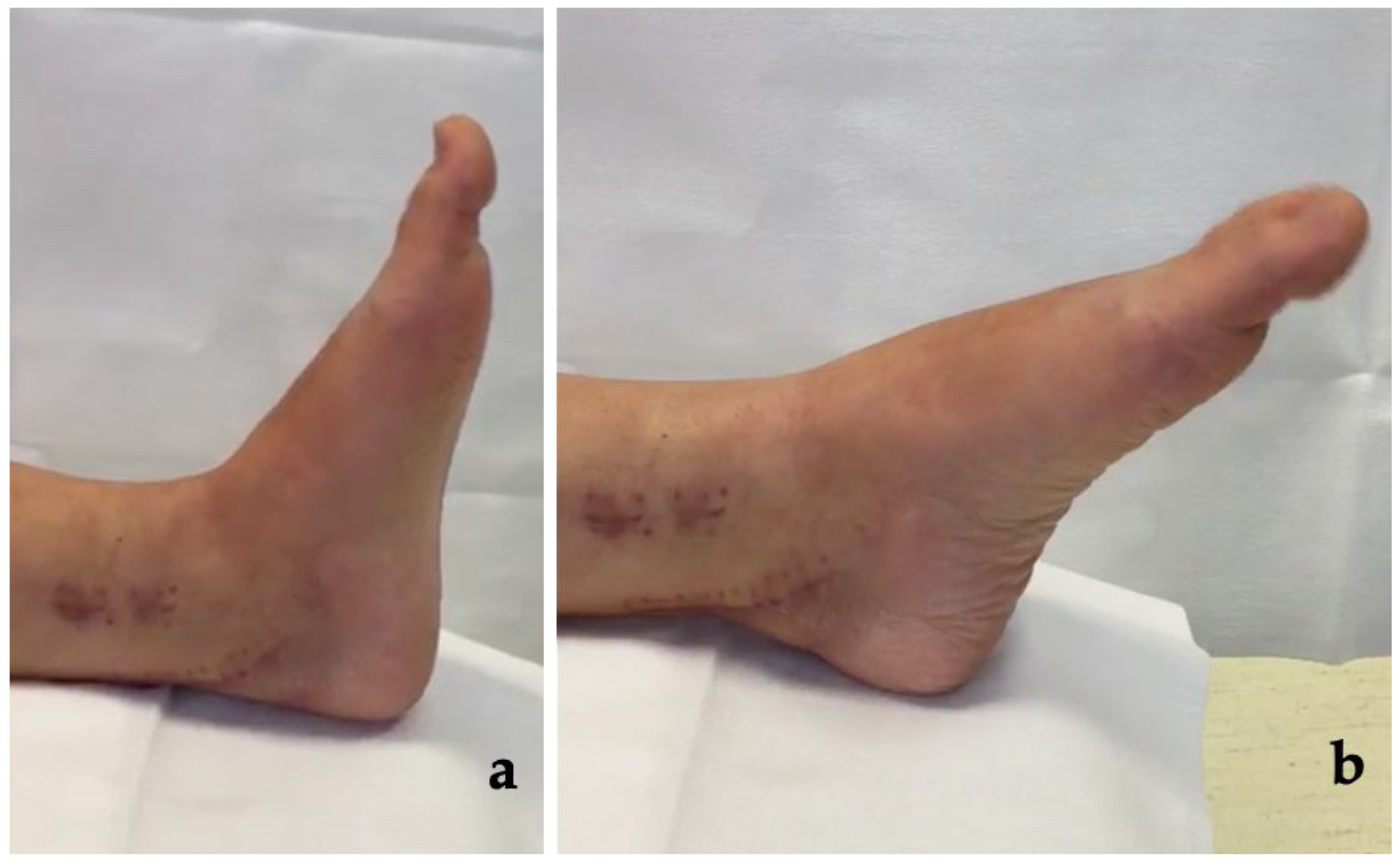
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
Appendix B
References
- Lee, J.H.; Kim, Y.J.; Baek, J.H.; Kim, D.H. Z-Plasty of the Flexor Hallucis Longus Tendon at Tarsal Tunnel for Checkrein Deformity. J. Orthop. Surg. 2016, 24, 354–357. [Google Scholar] [CrossRef] [Green Version]
- Holcomb, T.M.; Temple, E.W.; Barp, E.A.; Smith, H.L. Surgical Correction of Checkrein Deformity after Malunited Distal Tibia Fracture: A Case Report. J. Foot Ankle Surg. 2014, 53, 631–634. [Google Scholar] [CrossRef] [PubMed]
- Greco, T.; Cianni, L.; Polichetti, C.; Inverso, M.; Maccauro, G.; Perisano, C. Uncoated vs. Antibiotic-Coated Tibia Nail in Open Diaphyseal Tibial Fracture (42 According to AO Classification): A Single Center Experience. BioMed Res. Int. 2021, 2021, 7421582. [Google Scholar] [CrossRef] [PubMed]
- Perisano, C.; Greco, T.; Polichetti, C.; Inverso, M.; Maccauro, G. Antibiotic-Coated Nail in Open Tibial Fracture: A Retrospective Case Series. J. Funct. Morphol. Kinesiol. 2021, 6, 97. [Google Scholar] [CrossRef] [PubMed]
- Feeney, M.S.; Williams, R.L.; Stephens, M.M. Selective Lengthening of the Proximal Flexor Tendon in the Management of Acquired Claw Toes. J. Bone Jt. Surg. Br. 2001, 83, 335–338. [Google Scholar] [CrossRef]
- Yuen, C.P.; Lui, T.H. Adhesion of Flexor Hallucis Longus at the Site of a Tibial-Shaft Fracture—A Cause of a Checkrein Deformity. Foot Ankle Surg. 2015, 21, e23–e26. [Google Scholar] [CrossRef] [PubMed]
- Sinnett, T.; Rudge, B.; Clark, C. A Case of Check-Rein Deformities of the Great and Lesser Toes Treated through Exploration at the Midfoot. Foot Ankle Surg. 2015, 21, e6–e8. [Google Scholar] [CrossRef]
- Lee, H.S.; Kim, J.S. Treatment of Checkrein Deformity of the Hallux. J. Bone Jt. Surg. 2008, 90, 4. [Google Scholar] [CrossRef] [Green Version]
- Gadhavi, M.V.; Majmundar, D.D.; Solanki, R.A. Checkrein Deformity of the Great Toe Managed by Midfoot Flexor Hallucis Longus Z-Plasty: A Case Report. J Orthop Case Rep. 2019, 9, 18. [Google Scholar]
- Sanhudo, J.A.V.; Lompa, P.A. Checkrein Deformity–Flexor Hallucis Tethering: Two Case Reports. Foot Ankle Int. 2002, 23, 799–800. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, G.A.; Sferra, J.J. Checkrein Deformity—An Unusual Complication Associated with a Closed Salter-Harris Type II Ankle Fracture: A Case Report. Foot Ankle Int. 1999, 20, 591–594. [Google Scholar] [CrossRef] [PubMed]
- Leitschuh, P.H.; Zimmerman, J.P.; Uhorchak, J.M.; Arciero, R.A.; Bowser, L. Hallux Flexion Deformity Secondary to Entrapment of the Flexor Hallucis Longus Tendon after Fibular Fracture. Foot Ankle Int. 1995, 16, 232–235. [Google Scholar] [CrossRef] [PubMed]
- Bai, L.; You, T.; Zhang, W. Checkrein Deformity of the Hallux Caused by Misplaced Suture-Button Syndesmosis Fixation: A Case Report. J. Foot Ankle Surg. 2020, 59, 598–602. [Google Scholar] [CrossRef] [PubMed]
- Carr, J.B. Complications of Calcaneus Fractures Entrapment of the Flexor Hallucis Longus: Report of Two Cases. J. Orthop. Trauma 1990, 4, 166–168. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Lee, K.T.; Smith, R.W.; Park, Y.-U. Checkrein Deformity Secondary to Entrapment of FHL after Talus Fracture: A Case Report. Foot Ankle Int. 2010, 31, 336–338. [Google Scholar] [CrossRef]
- Abolfotouh, S.M.; Mahmoud, K.M.; Mekhaimar, M.M.; Said, N.; Al Dosari, M.A. Checkrein Deformity Associated with Intra-Articular Talar Fracture: A Report of Three Cases. JBJS Case Connect. 2015, 5, e21. [Google Scholar] [CrossRef]
- Feng, X.-J.; Jiang, Y.; Wu, J.-X.; Zhou, Y. Efficacy of Comprehensive Rehabilitation Therapy for Checkrein Deformity: A Case Report. World J. Clin. Cases 2020, 8, 444–450. [Google Scholar] [CrossRef]
- Sallent, A.; Soza, D.; Duarri, G.; Busquets, R. Checkrein Deformity: A Case Report of Two Patients with Hallux Deformity and Pain Following Mandibular Reconstruction in Oral Cancer Treatment. Oral Maxillofac. Surg. 2020, 24, 359–362. [Google Scholar] [CrossRef]
- Tanwar, Y.S.; Singh, S.; Arya, R.K.; Aujla, N.; Mathur, A.; Kharbanda, Y. A Closed Lateral Subtalar Dislocation with Checkrein Deformity of Great Toe due to Entrapment of Flexor Hallucis Longus: A Case Report. Foot Ankle Spec. 2016, 9, 461–464. [Google Scholar] [CrossRef]
- Rodriguez-Collell, J.R.; Mifsut-Miedes, D. Checkrein Deformity of the Hallux and Second Toe after Soft-Tissue Injury. Case Rep. Orthop. 2021, 2021, 8459586. [Google Scholar] [CrossRef]
- Greco, T.; Cianni, L.; De Mauro, D.; Dughiero, G.; Bocchi, M.B.; Cazzato, G.; Ragonesi, G.; Liuzza, F.; Maccauro, G.; Perisano, C. Foot Metastasis: Current Knowledge. Orthop. Rev. 2020, 12, 8671. [Google Scholar] [CrossRef] [PubMed]
- Greco, T.; Fulchignoni, C.; Cianni, L.; Maccauro, G.; Perisano, C. Surgical Management of Tibial Metastases: A Systematic Review. Acta Biomed. Atenei Parm. 2022, 92, e2021552. [Google Scholar] [CrossRef]
- Perisano, C.; Greco, T.; Vitiello, R.; Maccauro, G.; Liuzza, F.; Tamburelli, F.C.; Forconi, F. Mueller-Weiss Disease: Review of the Literature. J. Biol. Regul. Homeost. Agents 2018, 32, 157–162. [Google Scholar]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paul-Dauphin, A.; Guillemin, F.; Virion, J.M.; Briançon, S. Bias and Precision in Visual Analogue Scales: A Randomized Controlled Trial. Am. J. Epidemiol. 1999, 150, 1117–1127. [Google Scholar] [CrossRef] [Green Version]
- Leigheb, M.; Janicka, P.; Andorno, S.; Marcuzzi, A.; Magnani, C.; Grassi, F. Italian Translation, Cultural Adaptation and Validation of the “American Orthopaedic Foot and Ankle Society’s (AOFAS) Ankle-Hindfoot Scale”. Acta Biomed. 2016, 87, 38–45. [Google Scholar]
- Park, J.Y.; Wang, C.; Kim, H.D.; Kim, H.N. Tendon Split Lengthening Technique for Flexor Hallucis Longus Tendon Rupture. J. Orthop. Surg. Res. 2017, 12, 165. [Google Scholar] [CrossRef] [Green Version]
- Greco, T.; Vitiello, R.; Cazzato, G.; Cianni, L.; Malerba, G.; Maccauro, G.; Perisano, C. Intramedullary Antibiotic Coated Nail in Tibial Fracture: A Systematic Review. J. Biol. Regul. Homeost. Agents 2020, 34, 63–69. [Google Scholar]
- Bocchi, M.B.; Cianni, L.; Perna, A.; Raffaele, V.; Greco, T.; Maccauro, G.; Perisano, C. A Rare Case of Bacillus Megaterium Soft Tissues Infection. Acta Biomed. Atenei Parm. 2020, 91, e2020013. [Google Scholar] [CrossRef]

| Number of Patients | 14 | |
| Sex | 8M, 6F (57.1%; 42.9%) | |
| Age * | 37.4 ± 14.6 (range 19–63) | |
| Onset of Deformity * (months after trauma) | 7.0 ± 3.2 (range 1–12) | |
| Affected Toes 1 1, 2 1, 2, 3 | 10 2 2 | |
| VAS Pre * Post * | 8.0 ± 0.7 1.1 ± 0.8 | p < 0.05 |
| Hallux MTP Flexion Pre * Post * | 12.1 ± 4.6 36.0 ± 4.0 | p < 0.05 |
| Hallux IP Flexion Pre * Post * | 64.0 ± 7.2 11.4 ± 4.1 | p < 0.05 |
| AOFAS Score Pre * Post * | 39.7 ± 9.4 84.2 ± 8.5 | p < 0.05 |
| Follow-Up * (months) | 32.0 ± 10.6 (range 18–48) | |
| No. | Sex | Age | Etiology | First Treatment | Onset of Deformity (Months after Trauma) | Affected Toes | Follow-up (Months) |
|---|---|---|---|---|---|---|---|
| 1 | M | 50 | Tibial and fibular shaft fracture | IMN | 10 | 1 | 36 |
| 2 | F | 25 | Open distal tibial and fibular fracture # | EF + Plate and screws | 8 | 1, 2 | 20 |
| 3 | F | 32 | Bimalleolar ankle fracture | Plate and screws | 10 | 1 | 42 |
| 4 | M | 63 | Tibial and fibular shaft fracture | IMN | 7 | 1 | 24 |
| 5 | M | 21 | Tri-malleolar ankle fracture | Plate and screws | 9 | 1 | 48 |
| 6 | M | 19 | Tibial and fibular shaft fracture | IMN | 2 | 1 | 24 |
| 7 | F | 53 | Tibial plafond fracture # | Plate and screws | 1 | 1, 2, 3 | 36 |
| 8 | M | 28 | Tri-malleolar ankle fracture | Plate and screws | 5 | 1 | 36 |
| 9 | M | 39 | Tibial and fibular shaft fracture | IMN | 8 | 1 | 20 |
| 10 | F | 47 | Distal tibial and fibular fracture # | EF + Plate and screws | 10 | 1, 2 | 48 |
| 11 | M | 33 | Distal tibial and fibular fracture | Plate and screws | 6 | 1 | 18 |
| 12 | F | 20 | Open tibial shaft fracture | EF + IMN | 8 | 1, 2, 3 | 42 |
| 13 | F | 36 | Tibial plafond fracture # | Plate and screws | 12 | 1 | 32 |
| 14 | M | 58 | Bimalleolar ankle fracture | Plate and screws | 3 | 1 | 22 |
| No. | VAS | Hallux MTP Flexion (°) | Hallux IP Flexion (°) | AOFAS Score | ||||
|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | Pre | Post | Pre | Post | |
| 1 | 9 | 2 | 10 | 35 | 70 | 10 | 47 | 90 |
| 2 | 8 | 1 | 15 | 40 | 66 | 15 | 24 | 72 |
| 3 | 7 | 2 | 15 | 35 | 65 | 10 | 37 | 82 |
| 4 | 9 | 0 | 10 | 40 | 75 | 5 | 42 | 92 |
| 5 | 7 | 1 | 5 | 30 | 60 | 10 | 32 | 97 |
| 6 | 8 | 2 | 20 | 35 | 70 | 15 | 47 | 67 |
| 7 | 9 | 0 | 10 | 40 | 65 | 15 | 52 | 77 |
| 8 | 8 | 1 | 15 | 35 | 60 | 10 | 34 | 79 |
| 9 | 8 | 0 | 10 | 30 | 45 | 10 | 38 | 85 |
| 10 | 8 | 2 | 10 | 40 | 63 | 5 | 47 | 90 |
| 11 | 9 | 2 | 20 | 40 | 60 | 10 | 32 | 88 |
| 12 | 8 | 2 | 5 | 30 | 72 | 20 | 57 | 79 |
| 13 | 8 | 1 | 15 | 35 | 60 | 15 | 40 | 90 |
| 14 | 7 | 0 | 10 | 40 | 65 | 10 | 28 | 91 |
| Authors, Year | Number of Cases | Sex | Age | Etiology | Fingers Involved | Time Trauma to Deformity (Months) | Treatment | Follow-Up (Months) |
|---|---|---|---|---|---|---|---|---|
| Carr [14] 1990 | 2 | F | 21 35 | Calcaneus Fracture | 1 | Within 5 days | Tendon dislocation reduction | 30 24 |
| Leitschuh et al. [12], 1995 | 1 | M | 61 | Weber C ankle fracture | 1 | 18 | Release + medial tenodesis | NS |
| Rosenberg and Sferra [11], 1999 | 1 | M | 14 | Salter-Harris II distal tibia fracture and distal fibular shaft fracture | 1, 2 | 1,5 | Release + retro-malleolar tenodesis of tibialis posterior to FDL+ great toe IP and second toe PIP capsulotomies | NS |
| Feeney et al. [5], 2001 | 10 | 8M-2F | 27 * | 8 tibial shaft fracture; 1 post-traumatic compartment syndrome; 1 prolonged lithotomy positions with ankle strips | (1) 2–5 (2) 1 (2) 1–3 (2) 1–4 (3) 1–5 | 6 | FHL/FDL tendon lengthening with Z plasty | 12 |
| Sanhudo and Lompa [10], 2002 | 2 | 1M-1F | 45 31 | Distal fibular graft for hip surgery; Weber C ankle fracture | 1 | 2 1.5 | (I) release + retro-malleolar tendon lengthening (II) FHL and FDL lengthening at midfoot | NS |
| Lee and Kim [8], 2008 | 11 | 6M-5F | 36 * | Bimalleolar, tri-malleolar, pilon, biosseous leg fracture, soft tissue injury without fracture | (5) 1 (5) 1–2–3 (1) 1–2 | 3.5 * | (6) midfoot lengthening of FHL by Z plasty(+2 weeks with short removable splint) (5) release and musculotendinous Z-plasty lengthening | 20.4 * |
| Kim et al. [15], 2010 | 1 | M | 44 | Ankle sprain with talar fracture | 1 | 2 | fracture reduction+ tendon release with posteromedial approach | 2 |
| Holcomb et al. [2], 2014 | 1 | M | 19 | Distal tibia fracture | 1–2–3 | 60 | FHL tenotomy over the IP joint + hallux IP joint arthrodesis | 12 |
| Sinnet et al. [7], 2015 | 1 | M | 22 | Distal tibia and fibula fracture | 1 | 48 | Midfoot FHL tendon Z-plasty | 3 |
| Abolfotouh et al. [16], 2015 | 3 | M | 40 36 30 | Intra-articular talar fracture | 1 | 0 | Fracture reduction + tendon release | 24 24 18 |
| Yuen and Lui [6], 2015 | 1 | M | 36 | Tibial and fibular shaft fracture | 1–2–3 | 6 | Rehabilitation therapy first, FHL tendon Z-plasty with posteromedial approach to the distal tibia | 17 |
| Tanwar et al. [19], 2016 | 1 | M | 26 | Peri-talar dislocation | 1 | 0 | Dislocation reduction + stabilization with 2 Kirschner wires across subtalar joint and 1 across talonavicular joint | NS |
| Lee et al. [1], 2016 | 8 | 6M-2F | 39,5 * | Tibiofibular, distal fibular fracture and crush injury around the ankle | 1–2 | 8.4 * | Retro-malleolar FHL tendon Z-plasty | 3.4 * |
| Park et al. [27], 2017 | 5 | M | 34,8 * | 2) laceration on great toe 3) IP joint dislocation | 1 | 1.5 * | Midfoot FHL tendon Z-plasty | 44 |
| Gadhavi et al. [9], 2019 | 1 | M | 25 | Distal tibia fracture | 1 | 24 | Midfoot FHL tendon Z-plasty | 3 |
| Bai et al. [13], 2020 | 1 | M | 32 | Ankle fracture-dislocation combined with syndesmosis injury | 1 | 2 | Removal of the suture-button device + midfoot FHL tendon tenotomy and suture of distal part of the FHL to the FDL | 24 |
| Feng at al. [17], 2020 | 1 | F | 28 | Fibular grafting for mandibular ameloblastoma | 1–2–3 | 20 days | Physical rehabilitation therapy | 6 |
| Sallent et al. [18], 2020 | 2 | M | 27 36 | Fibular free flap for mandibular mesenchymal chondrosarcoma/squamous carcinoma | 1–2 | NS 6 | Hallux arthrodesis + midfoot FHL tendon Z-plasty and FDL tendon tenotomy | NS 5 |
| Rodriguez-Collell and Mifsut-Miedes [20],2021 | 1 | M | 37 | Soft tissue trauma (compartment Syndrome) | 1–2 | 12 | Retro-malleolar FHL tendon Z-plasty and application of a pulvertaft suture to the flexor hallucis longus | NS |
| Greco et al. [3], 2021 | 1 | M | 63 | Open tibia and fibula fracture | 1 | 7 | Retro-malleolar FHL tendon Z-plasty | 24 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Polichetti, C.; Greco, T.; Inverso, M.; Maccauro, G.; Forconi, F.; Perisano, C. Retro-Malleolar Z-Plasty of Flexor Hallucis Longus Tendon in Post-Traumatic Checkrein Deformity: A Case Series and Literature Review. Medicina 2022, 58, 1072. https://doi.org/10.3390/medicina58081072
Polichetti C, Greco T, Inverso M, Maccauro G, Forconi F, Perisano C. Retro-Malleolar Z-Plasty of Flexor Hallucis Longus Tendon in Post-Traumatic Checkrein Deformity: A Case Series and Literature Review. Medicina. 2022; 58(8):1072. https://doi.org/10.3390/medicina58081072
Chicago/Turabian StylePolichetti, Chiara, Tommaso Greco, Michele Inverso, Giulio Maccauro, Fabrizio Forconi, and Carlo Perisano. 2022. "Retro-Malleolar Z-Plasty of Flexor Hallucis Longus Tendon in Post-Traumatic Checkrein Deformity: A Case Series and Literature Review" Medicina 58, no. 8: 1072. https://doi.org/10.3390/medicina58081072
APA StylePolichetti, C., Greco, T., Inverso, M., Maccauro, G., Forconi, F., & Perisano, C. (2022). Retro-Malleolar Z-Plasty of Flexor Hallucis Longus Tendon in Post-Traumatic Checkrein Deformity: A Case Series and Literature Review. Medicina, 58(8), 1072. https://doi.org/10.3390/medicina58081072








