The Characteristics of Benzodiazepine Prescribing in the Republic of Srpska, Bosnia and Herzegovina
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Collection and Analyses
2.2. Statistical Analyses
3. Results
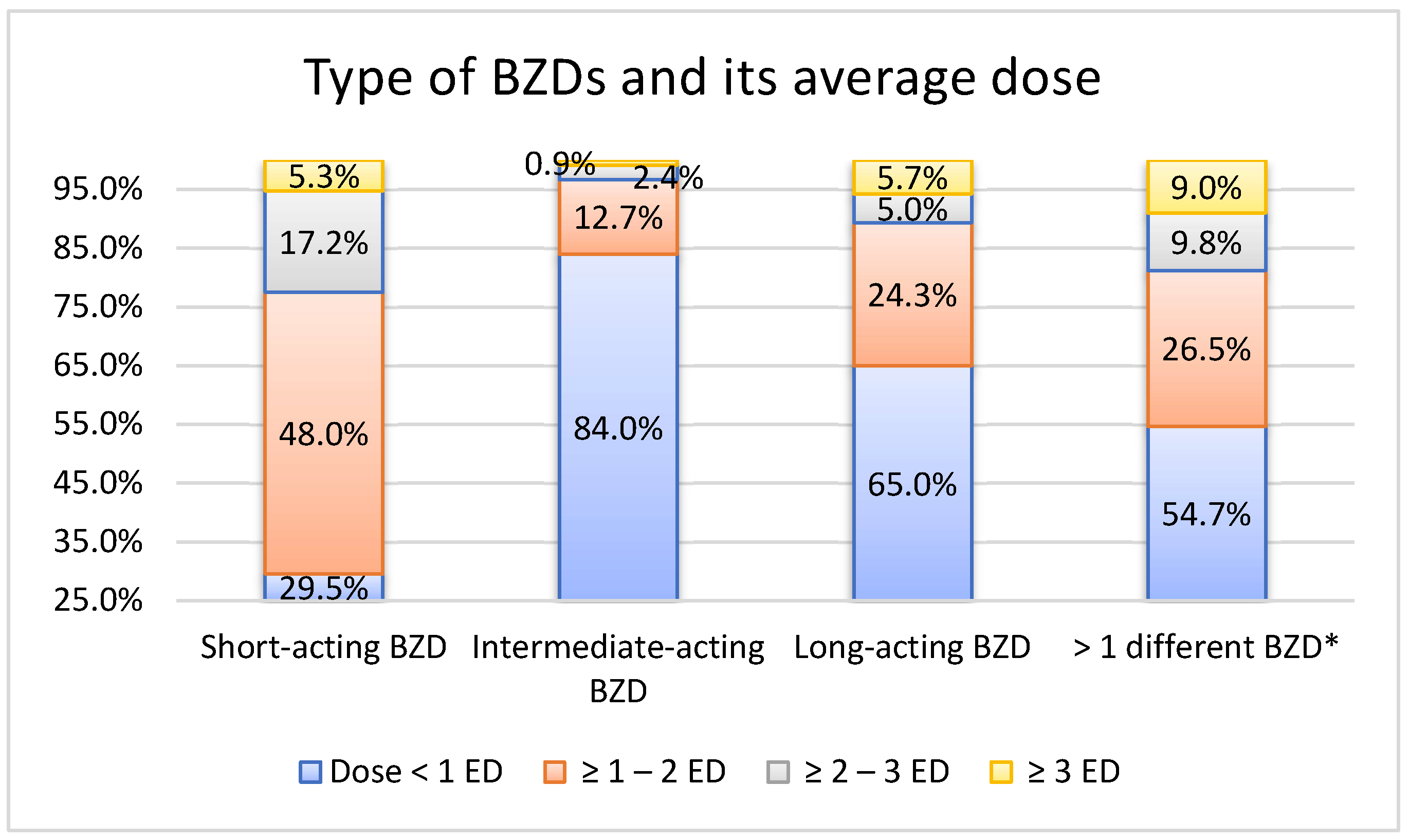
3.1. Type of BZDs Prescribed
3.2. Dose of BZDs Prescribed
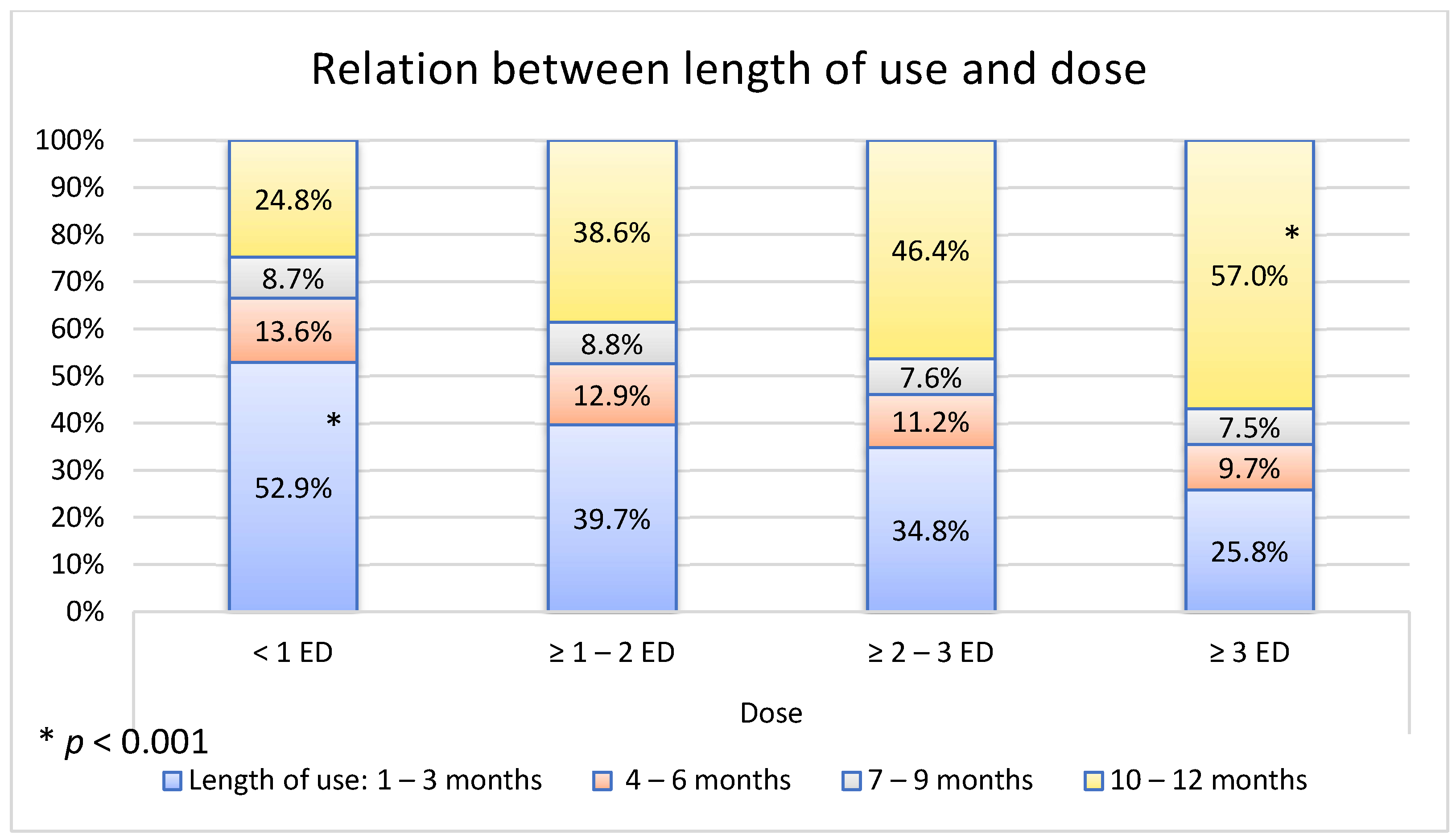
3.3. Length of Use of BZDs
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brett, J.; Murnion, B. Management of benzodiazepine misuse and dependence. Aust. Prescr. 2015, 38, 152–155. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guina, J.; Merrill, B. Benzodiazepines I: Upping the care on downers: The evidence of risks, benefits and alternatives. J. Clin. Med. 2018, 7, 17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lader, M. Benzodiazepines revisited—Will we ever learn? Addiction 2011, 106, 2086–2109. [Google Scholar] [CrossRef]
- Jacob, L.; Rapp, M.A.; Kostev, K. Long-term use of benzodiazepines in older patients in Germany: A retrospective analysis. Ther. Adv. Psychopharmacol. 2017, 7, 191–200. [Google Scholar] [CrossRef]
- Maksimović, Ž.; Stajić, M.; Lončar-Stojiljković, D. Analysis of the benzodiazepine prescribing patterns in the primary healthcare of the Republic of Srpska. Scr. Med. 2019, 50, 89–97. [Google Scholar] [CrossRef]
- Maric, N.P.; Latas, M.; Andric Petrovic, S.; Soldatovic, I.; Arsova, S.; Crnkovic, D.; Gugleta, D.; Ivezic, A.; Janjic, V.; Karlovic, D.; et al. Prescribing practices in Southeastern Europe—Focus on benzodiazepine prescription at discharge from nine university psychiatric hospitals. Psychiatry Res. 2017, 258, 59–65. [Google Scholar] [CrossRef]
- Airagnes, G.; Pelissolo, A.; Lavallée, M.; Flament, M.; Limosin, F. Benzodiazepine misuse in the elderly: Risk factors, consequences, and management. Curr. Psychiatry Rep. 2016, 18, 89. [Google Scholar] [CrossRef] [PubMed]
- Pariente, A.; Dartigues, J.F.; Benichou, J.; Letenneur, L.; Moore, N.; Fourrier-Réglat, A. Benzodiazepines and injurious falls in community dwelling elders. Drugs Aging 2008, 25, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Palmaro, A.; Dupouy, J.; Lapeyre-Mestre, M. Benzodiazepines and risk of death: Results from two large cohort studies in France and UK. Eur. Neuropsychopharmacol. 2015, 25, 1566–1577. [Google Scholar] [CrossRef]
- Kurko, T.A.; Saastamoinen, L.K.; Tähkäpää, S.; Tuulio-Henriksson, A.; Taiminen, T.; Tiihonen, J.; Airaksinen, M.S.; Hietala, J. Long-term use of benzodiazepines: Definitions, prevalence and usage patterns—A systematic review of register-based studies. Eur. Psychiatry 2015, 30, 1037–1047. [Google Scholar] [CrossRef]
- Airagnes, G.; Lemogne, C.; Renuy, A.; Goldberg, M.; Hoertel, N.; Roquelaure, Y.; Limosin, F.; Zins, M. Prevalence of prescribed benzodiazepine long-term use in the French general population according to sociodemographic and clinical factors: Findings from the CONSTANCES cohort. BMC Public Health 2019, 19, 566. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mokh, I.F.; Bjorner, T.; Skomedal, T. Risk factors for excessive benzodiazepine use in a working age population: A nationwide 5-year survey in Norway. Scand. J. Prim. Helath Care 2015, 33, 252–259. [Google Scholar]
- WHO Collaborating Centre for Drug Statistics Methodology. ATC/DDD System. Available online: https://www.whocc.no/atc_ddd_index/ (accessed on 26 November 2021).
- Republic of Srpska Government. Ministry of Health and Social Welfare. Legislation in the Field of Pharmacy Activities in the Republic of Srpska. Ministry of Health and Social Welfare of the Republic of Srpska. Serbian. 2010. Available online: https://www.vladars.net/sr-SP-Cyrl/Vlada/Ministarstva/MZSZ/Documents/Zakonska%20regulativa%20u%20oblasti%20apotekarske%20djelatnosti%20u%20Republici%20Srpskoj.pdf/ (accessed on 26 November 2021).
- Benzo.org.uk. The Resource Site for Involuntary Benzodiazepine Tranquiliser Addiction, Withdrawal & Recovery. Benzodiazepine Equivalence Table. 2016. Available online: http://www.benzo.org.uk/bzequiv.htm (accessed on 26 November 2021).
- Medscape. Benzodiazepine Equivalency Table. 2018. Available online: http://emedicine.medscape.com/article/2172250-overview/ (accessed on 26 November 2021).
- Sonnenberg, C.M.; Bierman, E.; Deeg, D.; Comijs, H.; Tilburg, W.; Beekman, A. Ten-year trends in benzodiazepine use in the Dutch population. Soc. Psychiatry Psychiatr. Epidemiol. 2012, 47, 293–301. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alvarenga, J.M.; Loyola Filho, A.I.; Firmo, J.O.A.; Lima-Costa, M.F.; Uchoa, E. Prevalence and sociodemographic characteristics associated with benzodiazepines use among community dwelling older adults: The Bambuí Health and Aging Study (BHAS). Rev. Bras. Psiquiatr. 2008, 30, 7–11. [Google Scholar] [CrossRef] [Green Version]
- Nordfjærn, T.; Bjerkeset, O.; Bratberg, G.; Moylan, S.; Berk, M.; Gråwe, R. Socio-demographic, lifestyle and psychological predictors of benzodiazepine and z-hypnotic use patterns. Nord. J. Psychiatry 2014, 68, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Taipale, H.; Särkilä, H.; Tanskanen, A.; Kurko, T.; Taiminen, T.; Tiihonen, J.; Sund, R.; Tuulio-Henriksson, A.; Saastamoinen, L.; Hietala, J. Incidence of and characteristics associated with long-term benzodiazepine use in Finland. JAMA Netw. Open 2020, 3, e2019029. [Google Scholar] [CrossRef]
- Maust, D.T.; Lin, L.A.; Blow, F.C. Benzodiazepine use and misuse among adults in the United States. Psychiatr. Serv. 2019, 70, 97–106. [Google Scholar] [CrossRef]
- Sundseth, A.C.; Gjelstad, S.; Straand, J.; Rosvold, E.O. General practitioners’ prescriptions of benzodiazepines, Z-hypnotics and opioid analgesics for elderly patients during direct and indirect contacts. A cross-sectional, observational study. Scand. J. Prim. Health Care 2018, 36, 115–122. [Google Scholar] [CrossRef]
- Zandstra, S.M.; van Rijswijk, E.; Rijnders, C.A.T.; van de Lisdonk, E.H.; Bor, J.H.J.; van Weel, C.; Zitman, F.G. Long-term benzodiazepine users in family practice: Differences from short-term users in mental health, coping behaviour and psychological characteristics. Fam. Pract. 2004, 21, 266–269. [Google Scholar] [CrossRef] [Green Version]
- Romans, S.; Cohen, M.; Forte, T. Rates of depression and anxiety in urban and rural Canada. Soc. Psychiatry Psychiatr. Epidemiol. 2011, 46, 567–575. [Google Scholar] [CrossRef]
- Tahiri, Z.; Kellici, S.; Mone, I.; Shabani, D.; Qazimi, M.; Burazeri, G. Prevalence and correlates of inappropriate use of benzodiazepines in Kosovo. Int. J. Clin. Pharm. 2017, 39, 669–673. [Google Scholar] [CrossRef] [PubMed]
- Janhsen, K.; Roser, P.; Hoffmann, K. The problems of long-term treatment with benzodiazepines and related substances. Dtsch. Arztebl. Int. 2015, 112, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sirdifield, C.; Anthierens, S.; Creupelandt, H.; Chipchase, S.Y.; Christiaens, T.; Siriwardena, A.N. General practitioners’ experiences and perceptions of benzodiazepine prescribing: Systematic review and meta-synthesis. BMC Fam. Pract. 2013, 14, 191. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mokhar, A.; Kuhn, S.; Topp, J.; Dirmaier, J.; Härter, M.; Verthein, U. Long-term use of benzodiazepines and Z drugs: A qualitative study of patients’ and healthcare professionals’ perceptions and possible levers for change. BJGP Open 2019, 3, bjgpopen18X101626. [Google Scholar] [CrossRef]
- Offidani, E.; Guidi, J.; Tomba, E.; Fava, G.A. Efficacy and tolerability of benzodiazepines versus antidepressants in anxiety disorders: A systematic review and meta-analysis. Psychother. Psychosom. 2013, 82, 355–362. [Google Scholar] [CrossRef]
- Rickels, K.; Moeller, H.J. Benzodiazepines in anxiety disorders: Reassessment of usefulness and safety. World J. Biol. Psychiatry 2019, 20, 514–518. [Google Scholar] [CrossRef]
- Takeshima, N.; Ogawa, Y.; Hayasaka, Y.; Furukawa, T.A. Continuation and discontinuation of benzodiazepine prescriptions: A cohort study based on a large claims database in Japan. Psychiatry Res. 2016, 237, 201–207. [Google Scholar] [CrossRef] [Green Version]
- Hata, T.; Kanazawa, T.; Hamada, T.; Nishihara, M.; Bush, A.I.; Yoneda, H.; Nakajima, M.; Katsumata, T. What can predict and prevent the long-term use of benzodiazepines? J. Psychiatr. Res. 2018, 97, 94–100. [Google Scholar] [CrossRef]
- Creupelandt, H.; Anthierens, S.; Habraken, H.; Declercq, T.; Sirdifield, C.; Siriwardena, A.N.; Christiaens, T. Teaching young GPs to cope with psychosocial consultations without prescribing: A durable impact of an e-module on determinants of benzodiazepines prescribing. BMC Med. Educ. 2017, 17, 259. [Google Scholar] [CrossRef] [Green Version]
- Kurko, T.; Saastamoinen, L.K.; Tuulio-Henriksson, A.; Taiminen, T.; Tiihonen, J.; Airaksinen, M.; Hietala, J. Trends in the long-term use of benzodiazepine anxiolytics and hypnotics: A national register study for 2006 to 2014. Pharmacoepidemiol. Drug Saf. 2018, 27, 674–682. [Google Scholar] [CrossRef]
- Marković-Peković, V.; Stoisavljević-Satara, S.; Skrbić, R. Outpatient utilization of drugs acting on nervous system: A study from the Republic of Srpska, Bosnia & Herzegovina. Eur. J. Clin. Pharmacol. 2010, 66, 177–186. [Google Scholar] [PubMed]
- Ait-Daoud, N.; Hamby, A.S.; Sharma, S.; Blevins, D. A review of alprazolam use, misuse, and withdrawal. J. Addict. Med. 2018, 12, 4–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Duration of BZD Action | INN | ATC Code | ED |
|---|---|---|---|
| Alprazolam | N05BA12 | 0.5 mg | |
| Short-acting | Brotizolam | N05CD09 | 0.25 mg |
| (t1/2 < 12 h) | Midazolam | N05CD08 | 5 mg |
| Oxazepam | N05BA04 | 20 mg | |
| Intermediate-acting (t1/2 = 12–24 h) | Bromazepam | N05BA08 | 5 mg |
| Lorazepam | N05BA06 | 1 mg | |
| Nitrazepam | N05CD02 | 10 mg | |
| Diazepam | N05BA01 | 10 mg | |
| Clorazepate | N05BA05 | 15 mg | |
| Long-acting | Flurazepam | N05CD01 | 20 mg |
| (t1/2 > 24 h) | Clobazam | N05BA09 | 20 mg |
| Clonazepam | N03AE01 | 0.5 mg | |
| Medazepam | N05BA03 | 10 mg | |
| Prazepam | N05BA11 | 10 mg |
| Variable | N | % | ED | Length of Use |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||
| Gender | ||||
| Male | 52,254 | 34.56 | 0.98 ± 0.96 | 5.39 ± 4.51 |
| Female | 98,950 | 65.44 | 0.83 ± 0.79 | 5.72 ± 4.50 |
| Age | ||||
| 18–40 years | 16,782 | 11.10 | 0.96 ± 1.03 | 3.68 ± 3.92 |
| 41–65 years | 74,731 | 49.42 | 0.91 ± 0.89 | 5.47 ± 4.49 |
| ≥66 years | 59,691 | 39.48 | 0.83 ± 0.75 | 6.27 ± 4.53 |
| Marital status | ||||
| Married | 59,781 | 39.54 | 0.86 ± 0.82 | 5.65 ± 4.51 |
| Single | 91,423 | 60.46 | 0.89 ± 0.88 | 5.54 ± 4.51 |
| Place of residence | ||||
| Urban areas | 105,365 | 69.68 | 0.87 ± 0.84 | 6.35 ± 4.53 |
| Rural areas | 45,839 | 30.32 | 0.92 ± 0.90 | 5.26 ± 4.46 |
| Total | 151,204 | 100.00 | 0.88 ± 0.86 | 5.59 ± 4.51 |
| Variable | N | % |
|---|---|---|
| Length of use (mean ± SD: 5.59 ± 4.51) | ||
| 1–3 months | 73,061 | 48.32 |
| 4–6 months | 19,980 | 13.21 |
| 7–9 months | 12,988 | 8.59 |
| 10–12 months | 45,175 | 29.88 |
| Dose (mean ± SD: 0.88 ± 0.86) | ||
| <1 ED | 107,040 | 70.79 |
| 1–2 ED | 30,928 | 20.45 |
| 2–3 ED | 8147 | 5.39 |
| >4 ED | 5089 | 3.37 |
| Type of BZD | ||
| Short-acting BZD | 15,435 | 10.21 |
| Intermediate-acting BZD | 85,030 | 56.24 |
| Long-acting BZD | 25,742 | 17.02 |
| >1 different BZD | 24,997 | 16.53 |
| Total | 151,204 | 100.00 |
| Factors | MRA for Dose | ||
|---|---|---|---|
| β | t | p | |
| Length of use | 0.235 | 65.55 | 0.001 |
| Age | −0.094 | 25.90 | 0.001 |
| Gender (male) | 0.086 | 24.20 | 0.001 |
| Marital status (married) | −0.024 | 6.89 | 0.001 |
| Factors | MRA for Length of Use | ||
|---|---|---|---|
| β | t | p | |
| Dose | 0.229 | 65.55 | 0.001 |
| Age | 0.187 | 53.15 | 0.001 |
| Gender (male) | −0.045 | 12.78 | 0.001 |
| Marital status (married) | 0.018 | 5.19 | 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maksimović, Ž.M.; Stajić, M.; Stojiljković, M.P.; Stoisavljević Šatara, S.; Stojaković, N.; Škrbić, R. The Characteristics of Benzodiazepine Prescribing in the Republic of Srpska, Bosnia and Herzegovina. Medicina 2022, 58, 980. https://doi.org/10.3390/medicina58080980
Maksimović ŽM, Stajić M, Stojiljković MP, Stoisavljević Šatara S, Stojaković N, Škrbić R. The Characteristics of Benzodiazepine Prescribing in the Republic of Srpska, Bosnia and Herzegovina. Medicina. 2022; 58(8):980. https://doi.org/10.3390/medicina58080980
Chicago/Turabian StyleMaksimović, Žana M., Mladen Stajić, Miloš P. Stojiljković, Svjetlana Stoisavljević Šatara, Nataša Stojaković, and Ranko Škrbić. 2022. "The Characteristics of Benzodiazepine Prescribing in the Republic of Srpska, Bosnia and Herzegovina" Medicina 58, no. 8: 980. https://doi.org/10.3390/medicina58080980
APA StyleMaksimović, Ž. M., Stajić, M., Stojiljković, M. P., Stoisavljević Šatara, S., Stojaković, N., & Škrbić, R. (2022). The Characteristics of Benzodiazepine Prescribing in the Republic of Srpska, Bosnia and Herzegovina. Medicina, 58(8), 980. https://doi.org/10.3390/medicina58080980






