Successful Plate Fixation with Long Intramedullary Fibula Bone Graft for Periprosthetic Femur Fracture: A Case Report
Abstract
:1. Introduction
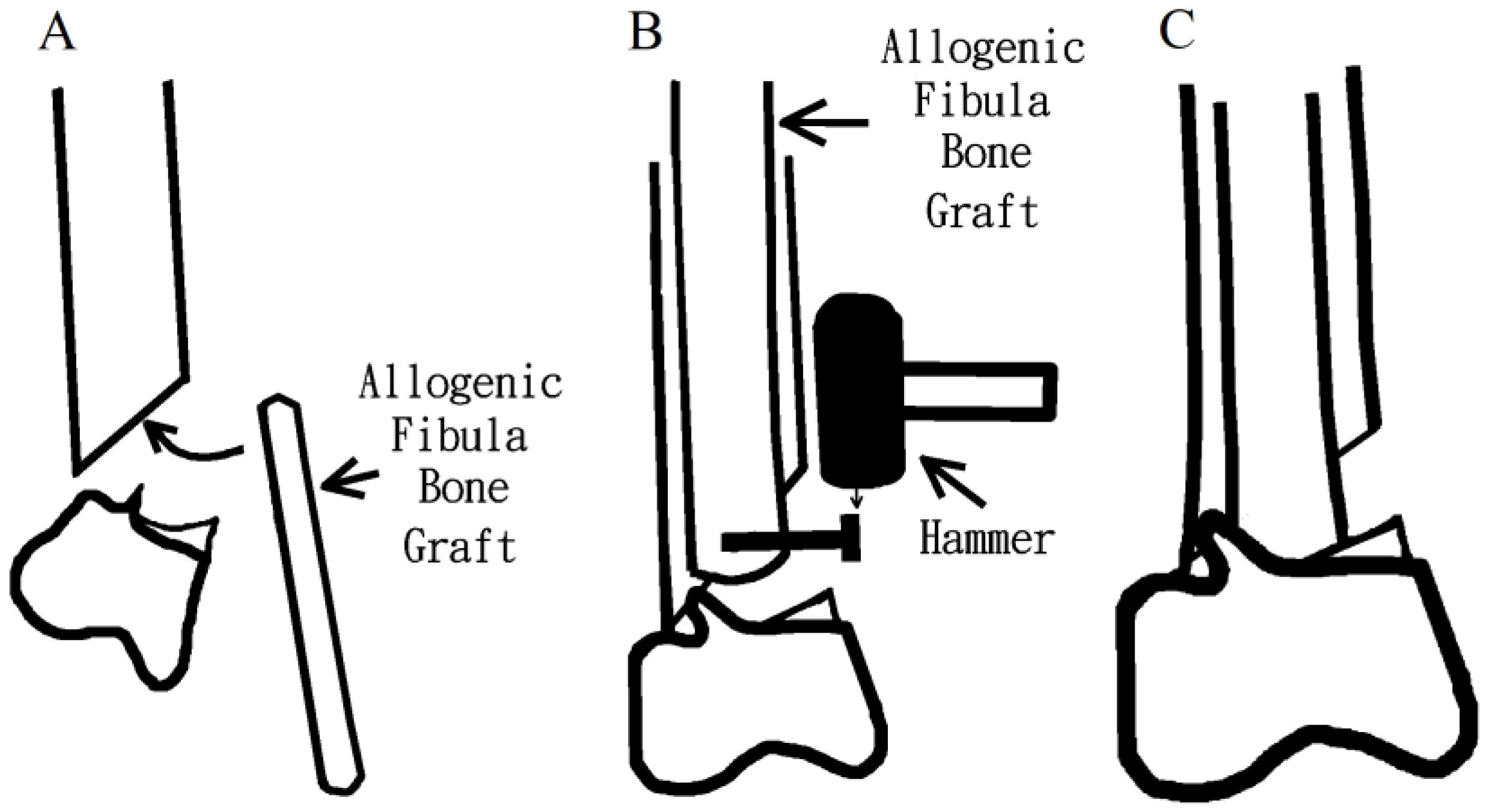
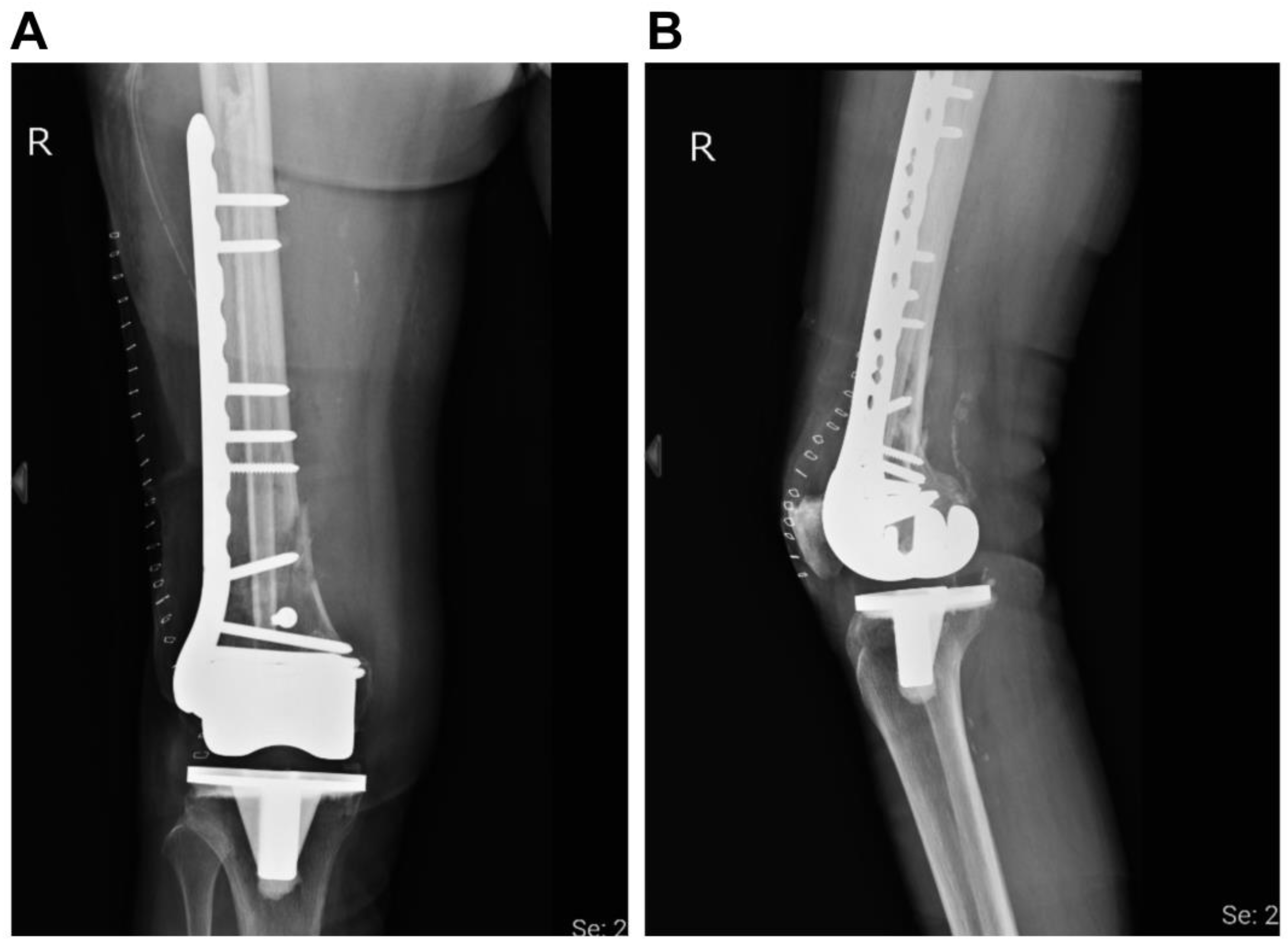
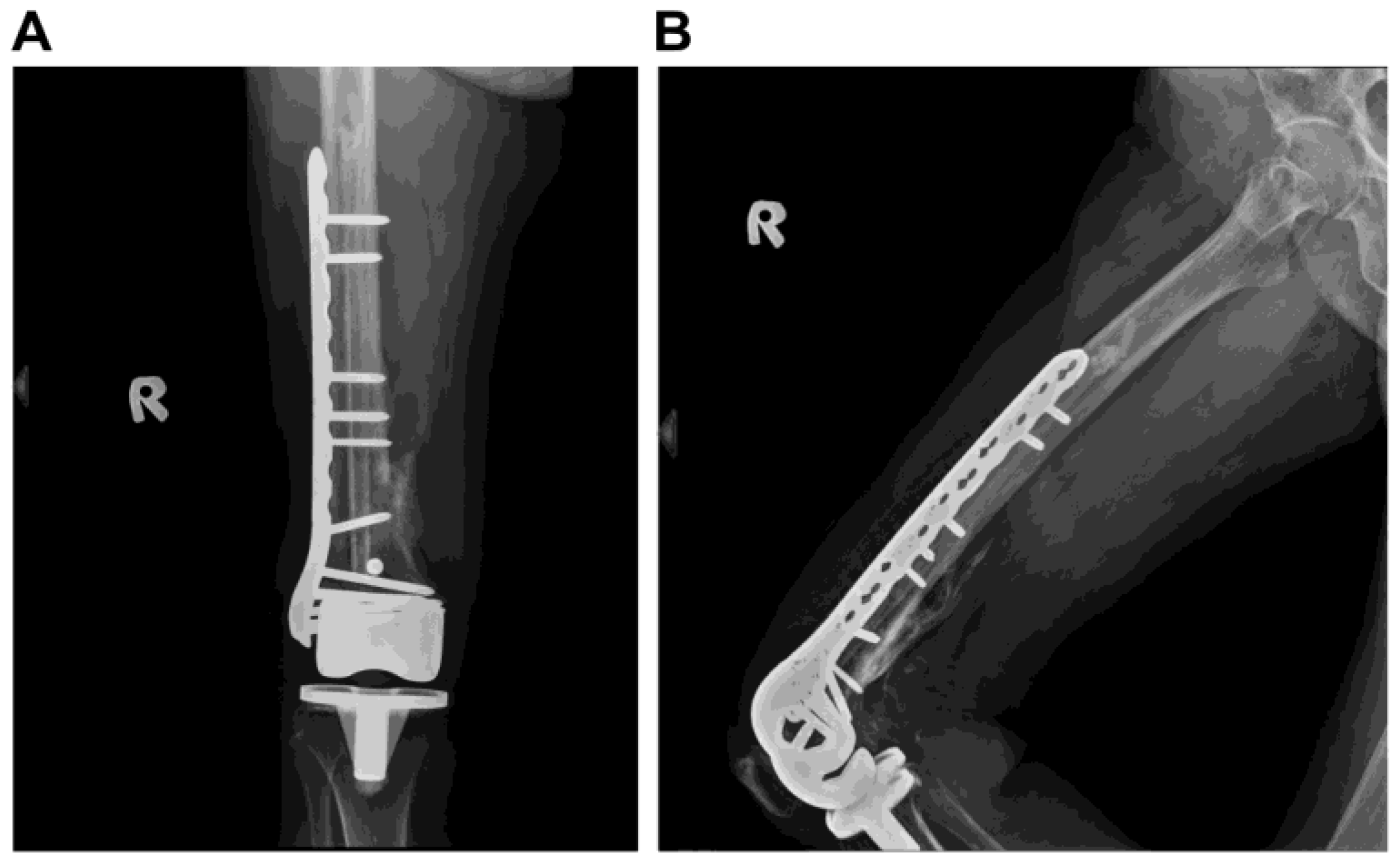
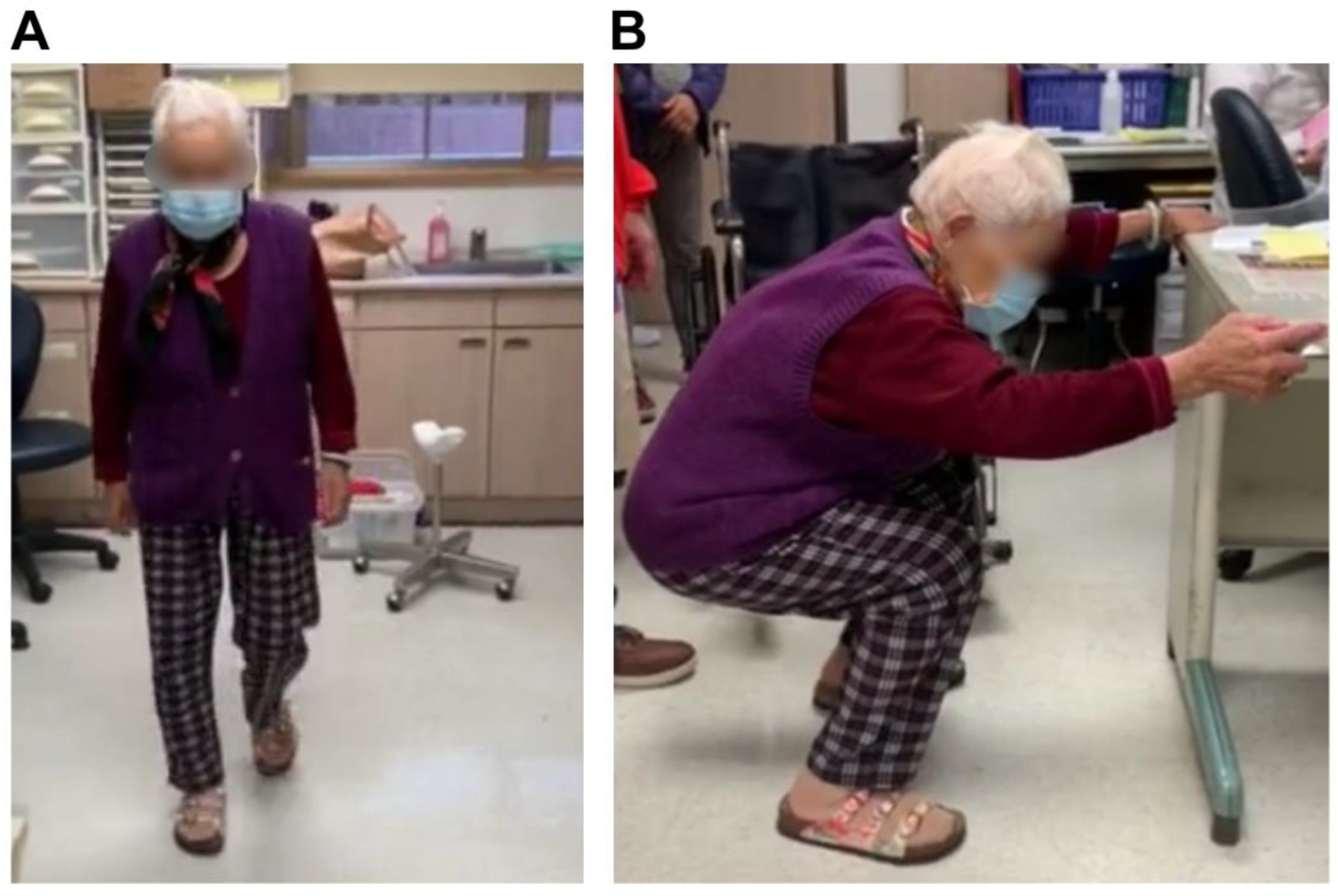
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siddiqi, A.; Smith, T.; McPhilemy, J.J.; Ranawat, A.S.; Sculco, P.K.; Chen, A.F. Soft-Tissue Balancing Technology for Total Knee Arthroplasty. JBJS Rev. 2020, 8, e0050. [Google Scholar] [CrossRef] [PubMed]
- Losina, E.; Walensky, R.P.; Kessler, C.L.; Emrani, P.S.; Reichmann, W.M.; Wright, E.A.; Holt, H.L.; Solomon, D.H.; Yelin, E.; Paltiel, A.D.; et al. Cost-effectiveness of total knee arthroplasty in the United States: Patient risk and hospital volume. Arch. Intern. Med. 2009, 169, 1113–1121, discussion 21–22. [Google Scholar] [CrossRef] [PubMed]
- Hussain, S.M.; Wang, Y.; Giles, G.G.; Graves, S.; Wluka, A.E.; Cicuttini, F.M. Female Reproductive and Hormonal Factors and Incidence of Primary Total Knee Arthroplasty Due to Osteoarthritis. Arthritis Rheumatol. 2018, 70, 1022–1029. [Google Scholar] [CrossRef] [PubMed]
- Rubin, L.E.; Blood, T.D.; Defillo-Draiby, J.C. Total Hip and Knee Arthroplasty in Patients Older than Age 80 Years. J. Am. Acad. Orthop. Surg. 2016, 24, 683–690. [Google Scholar] [CrossRef]
- Yohe, N.; Funk, A.; Ciminero, M.; Erez, O.; Saleh, A. Complications and Readmissions after Total Knee Replacement in Octogenarians and Nonagenarians. Geriatr. Orthop. Surg. Rehabil. 2018, 9, 2151459318804113. [Google Scholar] [CrossRef]
- Yoo, J.D.; Kim, N.K. Periprosthetic fractures following total knee arthroplasty. Knee Surg. Relat. Res. 2015, 27, 1–9. [Google Scholar] [CrossRef]
- Johnson, R.L.; Abdel, M.P.; Frank, R.D.; Chamberlain, A.M.; Habermann, E.B.; Mantilla, C.B. Frailty Index Is Associated with Periprosthetic Fracture and Mortality after Total Knee Arthroplasty. Orthopedics 2019, 42, 335–343. [Google Scholar] [CrossRef]
- Cordeiro, E.N.; Costa, R.C.; Carazzato, J.G.; Silva Jdos, S. Periprosthetic fractures in patients with total knee arthroplasties. Clin. Orthop. Relat. Res. 1990, 252, 182–189. [Google Scholar] [CrossRef]
- Rorabeck, C.H.; Taylor, J.W. Periprosthetic fractures of the femur complicating total knee arthroplasty. Orthop. Clin. N. Am. 1999, 30, 265–277. [Google Scholar] [CrossRef]
- Kumar, A.; Chambers, I.; Maistrelli, G.; Wong, P. Management of periprosthetic fracture above total knee arthroplasty using intramedullary fibular allograft and plate fixation. J. Arthroplast. 2008, 23, 554–558. [Google Scholar] [CrossRef]
- Sun, Z.H.; Liu, Y.J.; Li, H. Femoral stress and strain changes post-hip, -knee and -ipsilateral hip/knee arthroplasties: A finite element analysis. Orthop. Surg. 2014, 6, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Medda, S.; Kessler, R.B.; Halvorson, J.J.; Pilson, H.T.; Babcock, S.; Carroll, E.A. Technical Trick: Dual Plate Fixation of Periprosthetic Distal Femur Fractures. J. Orthop. Trauma. 2021, 35, e148–e152. [Google Scholar] [CrossRef] [PubMed]
- Liporace, F.A.; Yoon, R.S. Nail Plate Combination Technique for Native and Periprosthetic Distal Femur Fractures. J. Orthop. Trauma. 2019, 33, e64–e68. [Google Scholar] [CrossRef] [PubMed]
- Haidukewych, G.J. Role of Distal Femoral Replacement for Periprosthetic Fractures above a Total Knee Arthroplasty: When and How? J. Orthop. Trauma. 2019, 33 (Suppl. S6), S33–S35. [Google Scholar] [CrossRef]
- Hart, G.P.; Kneisl, J.S.; Springer, B.D.; Patt, J.C.; Karunakar, M.A. Open Reduction vs Distal Femoral Replacement Arthroplasty for Comminuted Distal Femur Fractures in the Patients 70 Years and Older. J. Arthroplast. 2017, 32, 202–206. [Google Scholar] [CrossRef]
- Ruder, J.A.; Hart, G.P.; Kneisl, J.S.; Springer, B.D.; Karunakar, M.A. Predictors of Functional Recovery Following Periprosthetic Distal Femur Fractures. J. Arthroplast. 2017, 32, 1571–1575. [Google Scholar] [CrossRef]
- Lombardo, D.J.; Siljander, M.P.; Sobh, A.; Moore, D.D.; Karadsheh, M.S. Periprosthetic fractures about total knee arthroplasty. Musculoskelet. Surg. 2020, 104, 135–143. [Google Scholar] [CrossRef]
- Medda, S.; Snoap, T.; Carroll, E.A. Setting Yourself Up for Success: Retrograde Intramedullary Nailing in Periprosthetic Fractures About Total Knee Arthroplasty. J. Orthop. Trauma. 2019, 33, S29–S32. [Google Scholar] [CrossRef]
- Delport, P.H.; Van Audekercke, R.; Martens, M.; Mulier, J.C. Conservative treatment of ipsilateral supracondylar femoral fracture after total knee arthroplasty. J. Trauma. 1984, 24, 846–849. [Google Scholar] [CrossRef]
- Cain, P.R.; Rubash, H.E.; Wissinger, H.A.; McClain, E.J. Periprosthetic femoral fractures following total knee arthroplasty. Clin. Orthop. Relat. Res. 1986, 208, 205–214. [Google Scholar] [CrossRef]
- Canton, G.; Ratti, C.; Fattori, R.; Hoxhaj, B.; Murena, L. Periprosthetic knee fractures. A review of epidemiology, risk factors, diagnosis, management and outcome. Acta Biomed. 2017, 88, 118–128. [Google Scholar] [PubMed]
- Herrera, D.A.; Kregor, P.J.; Cole, P.A.; Levy, B.A.; Jönsson, A.; Zlowodzki, M. Treatment of acute distal femur fractures above a total knee arthroplasty: Systematic review of 415 cases (1981–2006). Acta Orthop. 2008, 79, 22–27. [Google Scholar] [CrossRef] [PubMed]
- Healy, W.L.; Siliski, J.M.; Incavo, S.J. Operative treatment of distal femoral fractures proximal to total knee replacements. J. Bone Joint Surg. Am. 1993, 75, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Althausen, P.L.; Lee, M.A.; Finkemeier, C.G.; Meehan, J.P.; Rodrigo, J.J. Operative stabilization of supracondylar femur fractures above total knee arthroplasty: A comparison of four treatment methods. J. Arthroplast. 2003, 18, 834–839. [Google Scholar] [CrossRef]
- Saidi, K.; Ben-Lulu, O.; Tsuji, M.; Safir, O.; Gross, A.E.; Backstein, D. Supracondylar periprosthetic fractures of the knee in the elderly patients: A comparison of treatment using allograft-implant composites, standard revision components, distal femoral replacement prosthesis. J. Arthroplast. 2014, 29, 110–114. [Google Scholar] [CrossRef]
- Kolb, W.; Guhlmann, H.; Windisch, C.; Marx, F.; Koller, H.; Kolb, K. Fixation of periprosthetic femur fractures above total knee arthroplasty with the less invasive stabilization system: A midterm follow-up study. J. Trauma. 2010, 69, 670–676. [Google Scholar] [CrossRef]
- Han, H.S.; Oh, K.W.; Kang, S.B. Retrograde intramedullary nailing for periprosthetic supracondylar fractures of the femur after total knee arthroplasty. Clin. Orthop. Surg. 2009, 1, 201–206. [Google Scholar] [CrossRef]
- Ebraheim, N.A.; Kelley, L.H.; Liu, X.; Thomas, I.S.; Steiner, R.B.; Liu, J. Periprosthetic Distal Femur Fracture after Total Knee Arthroplasty: A Systematic Review. Orthop. Surg. 2015, 7, 297–305. [Google Scholar] [CrossRef]
- Liporace, F.A.; Yoon, R.S.; Collinge, C.A. Interprosthetic and Peri-Implant Fractures: Principles of Operative Fixation and Future Directions. J. Orthop. Trauma. 2017, 31, 287–292. [Google Scholar] [CrossRef]
- Yoon, R.S.; Patel, J.N.; Liporace, F.A. Nail and Plate Combination Fixation for Periprosthetic and Interprosthetic Fractures. J. Orthop. Trauma. 2019, 33, S18–S20. [Google Scholar] [CrossRef]
- Giordano, V.; Parilha Coutinho, B.; Miyahira, M.K.; de Souza, F.S.M.; do Amaral, N.P. Use of Nonvascularized Autologous Fibular Strut Graft in the Treatment of Major Bone Defect after Periprosthetic Knee Fracture. Case Rep. Orthop. 2017, 2017, 1650194. [Google Scholar] [CrossRef] [PubMed]
- Lawal, Y.Z.; Garba, E.S.; Ogirima, M.O.; Dahiru, I.L.; Maitama, M.I.; Abubakar, K.; Ejagwulu, F.S. Use of non-vascularized autologous fibula strut graft in the treatment of segmental bone loss. Ann. Afr. Med. 2011, 10, 25–28. [Google Scholar] [CrossRef] [PubMed]
- El Hage, S.; dos Santos, M.J.; de Moraes, E.L.; de Barros e Silva, L.B. Bone Tissue Donation: Tendency and Hurdles. Transplant. Proc. 2018, 50, 394–396. [Google Scholar] [CrossRef]
- Baldwin, P.; Li, D.J.; Auston, D.A.; Mir, H.S.; Yoon, R.S.; Koval, K.J. Autograft, Allograft, and Bone Graft Substitutes: Clinical Evidence and Indications for Use in the Setting of Orthopaedic Trauma Surgery. J. Orthop. Trauma. 2019, 33, 203–213. [Google Scholar] [CrossRef] [PubMed]
- Katz, M.S.; Ooms, M.; Heitzer, M.; Peters, F.; Winnand, P.; Kniha, K.; Möhlhenrich, S.C.; Hölzle, F.; Knobe, M.; Modabber, A. Postoperative Morbidity and Complications in Elderly Patients after Harvesting of Iliac Crest Bone Grafts. Medicina 2021, 57, 759. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yeh, K.-L.; Liaw, C.-K.; Fuh, C.-S.; Chen, C.-S.; Chiang, C.-H.; Shih, K.-S. Successful Plate Fixation with Long Intramedullary Fibula Bone Graft for Periprosthetic Femur Fracture: A Case Report. Medicina 2022, 58, 1148. https://doi.org/10.3390/medicina58091148
Yeh K-L, Liaw C-K, Fuh C-S, Chen C-S, Chiang C-H, Shih K-S. Successful Plate Fixation with Long Intramedullary Fibula Bone Graft for Periprosthetic Femur Fracture: A Case Report. Medicina. 2022; 58(9):1148. https://doi.org/10.3390/medicina58091148
Chicago/Turabian StyleYeh, Kuei-Lin, Chen-Kun Liaw, Chiou-Shann Fuh, Chu-Song Chen, Chen-Hao Chiang, and Kao-Shang Shih. 2022. "Successful Plate Fixation with Long Intramedullary Fibula Bone Graft for Periprosthetic Femur Fracture: A Case Report" Medicina 58, no. 9: 1148. https://doi.org/10.3390/medicina58091148
APA StyleYeh, K.-L., Liaw, C.-K., Fuh, C.-S., Chen, C.-S., Chiang, C.-H., & Shih, K.-S. (2022). Successful Plate Fixation with Long Intramedullary Fibula Bone Graft for Periprosthetic Femur Fracture: A Case Report. Medicina, 58(9), 1148. https://doi.org/10.3390/medicina58091148






