Accuracy of the Tibial Component Alignment by Extramedullary System Using Simple Radiographic References in Total Knee Arthroplasty
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
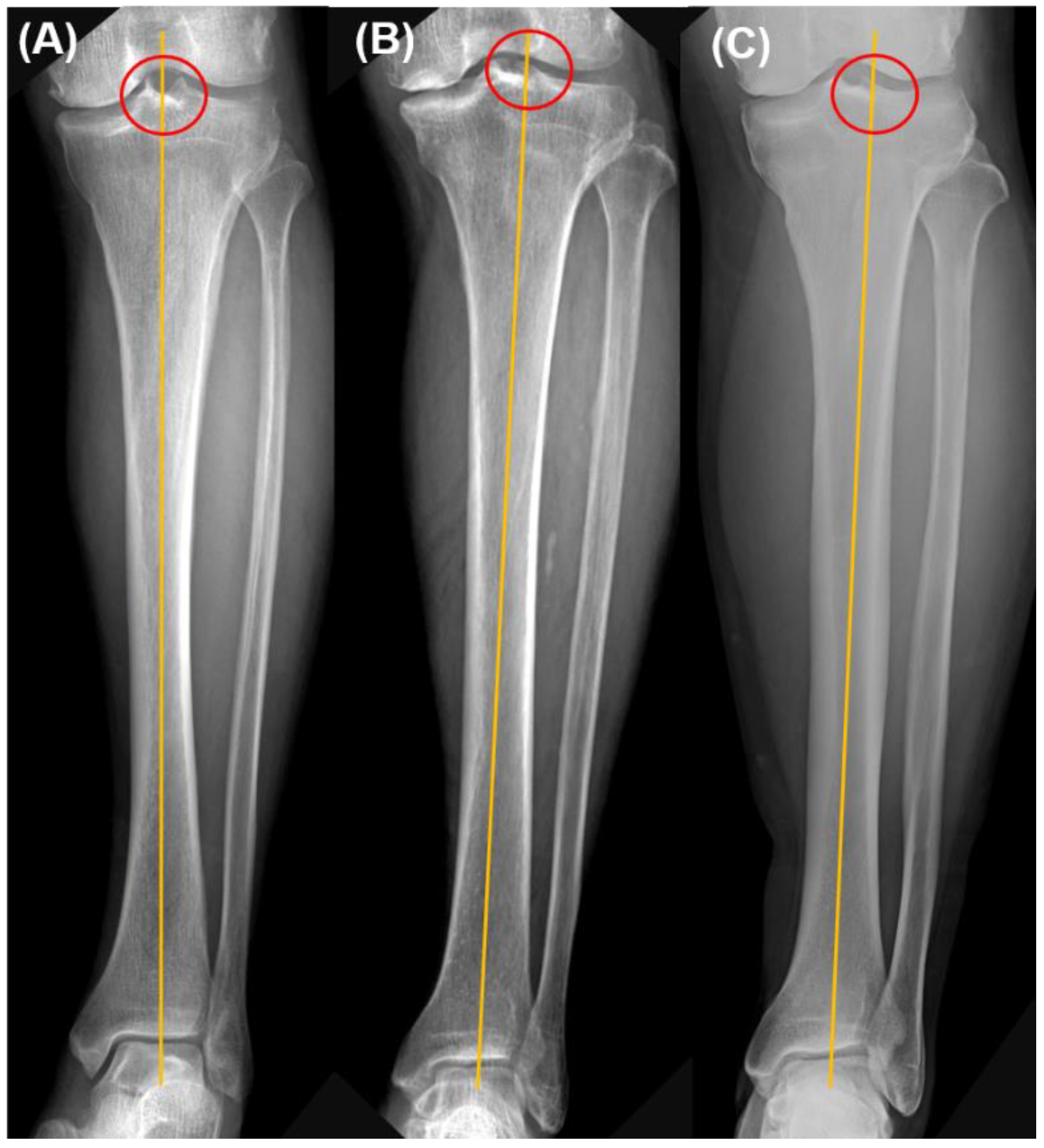
2.2. Radiographic and Clinical Assessment
2.3. Pre-Operative Planning
2.4. Intraoperative Planning
2.5. Operative Procedure
2.6. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lee, Y.S.; Howell, S.M.; Won, Y.Y.; Lee, O.S.; Lee, S.H.; Vahedi, H.; Teo, S.H. Kinematic alignment is a possible alternative to mechanical alignment in total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 3467–3479. [Google Scholar] [CrossRef] [PubMed]
- Yoon, J.R.; Han, S.B.; Jee, M.K.; Shin, Y.S. Comparison of kinematic and mechanical alignment techniques in primary total knee arthroplasty: A meta-analysis. Medicine 2017, 96, e8157. [Google Scholar] [CrossRef] [PubMed]
- Young, S.W.; Walker, M.L.; Bayan, A.; Briant-Evans, T.; Pavlou, P.; Farrington, B. The Chitranjan, S. Ranawat Award: No Difference in 2-year Functional Outcomes Using Kinematic versus Mechanical Alignment in TKA: A Randomized Controlled Clinical Trial. Clin. Orthop. Relat. Res. 2017, 475, 9–20. [Google Scholar] [CrossRef] [PubMed]
- Vanlommel, L.; Vanlommel, J.; Claes, S.; Bellemans, J. Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 2325–2330. [Google Scholar] [CrossRef] [PubMed]
- Ritter, M.A.; Davis, K.E.; Meding, J.B.; Pierson, J.L.; Berend, M.E.; Malinzak, R.A. The effect of alignment and BMI on failure of total knee replacement. J. Bone Joint Surg. Am. 2011, 93, 1588–1596. [Google Scholar] [CrossRef]
- Liu, H.X.; Shang, P.; Ying, X.Z.; Zhang, Y. Shorter survival rate in varus-aligned knees after total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 2663–2671. [Google Scholar] [CrossRef]
- Li, Z.; Esposito, C.I.; Koch, C.N.; Lee, Y.Y.; Padgett, D.E.; Wright, T.M. Polyethylene Damage Increases with Varus Implant Alignment in Posterior-stabilized and Constrained Condylar Knee Arthroplasty. Clin. Orthop. Relat. Res. 2017, 475, 2981–2991. [Google Scholar] [CrossRef]
- Cheng, T.; Zhao, S.; Peng, X.; Zhang, X. Does computer-assisted surgery improve postoperative leg alignment and implant positioning following total knee arthroplasty? A meta-analysis of randomized controlled trials? Knee Surg. Sports Traumatol. Arthrosc. 2012, 20, 1307–1322. [Google Scholar] [CrossRef]
- Schotanus, M.G.M.; Thijs, E.; Heijmans, M.; Vos, R.; Kort, N.P. Favourable alignment outcomes with MRI-based patient-specific instruments in total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 2659–2668. [Google Scholar] [CrossRef]
- Kim, K.; Kim, J.; Lee, D.; Lim, S.; Eom, J. The Accuracy of Alignment Determined by Patient-Specific Instrumentation System in Total Knee Arthroplasty. Knee Surg. Relat. Res. 2019, 31, 19–24. [Google Scholar] [CrossRef]
- Akagi, M.; Oh, M.; Nonaka, T.; Tsujimoto, H.; Asano, T.; Hamanishi, C. An anteroposterior axis of the tibia for total knee arthroplasty. Clin. Orthop. Relat. Res. 2004, 420, 213–219. [Google Scholar] [CrossRef] [PubMed]
- Reed, M.R.; Bliss, W.; Sher, J.L.; Emmerson, K.P.; Jones, S.M.; Partington, P.F. Extramedullary or intramedullary tibial alignment guides: A randomised, prospective trial of radiological alignment. J. Bone Joint Surg. Br. 2002, 84, 858–860. [Google Scholar] [CrossRef] [PubMed]
- Cinotti, G.; Sessa, P.; D’Arino, A.; Ripani, F.R.; Giannicola, G. Improving tibial component alignment in total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 3563–3570. [Google Scholar] [CrossRef]
- Thippana, R.K.; Kumar, M.N. Lateralization of Tibial Plateau Reference Point Improves Accuracy of Tibial Resection in Total Knee Arthroplasty in Patients with Proximal Tibia Vara. Clin. Orthop. Surg. 2017, 9, 458–464. [Google Scholar] [CrossRef] [PubMed]
- Puliero, B.; Favreau, H.; Eichler, D.; Adam, P.; Bonnomet, F.; Ehlinger, M. Total knee arthroplasty in patients with varus deformities greater than ten degrees: Survival analysis at a mean ten year follow-up. Int. Orthop. 2019, 43, 333–341. [Google Scholar] [CrossRef]
- Rahm, S.; Camenzind, R.S.; Hingsammer, A.; Lenz, C.; Bauer, D.E.; Farshad, M.; Fucentese, S.F. Postoperative alignment of TKA in patients with severe preoperative varus or valgus deformity: Is there a difference between surgical techniques? BMC Musculoskelet. Disord. 2017, 18, 272. [Google Scholar] [CrossRef]
- Thienpont, E.; Parvizi, J. A New Classification for the Varus Knee. J. Arthroplast. 2016, 31, 2156–2160. [Google Scholar] [CrossRef]
- Kang, B.Y.; Lee, D.K.; Kim, H.S.; Wang, J.H. How to achieve an optimal alignment in medial opening wedge high tibial osteotomy? Knee Surg. Relat. Res. 2022, 34, 3. [Google Scholar] [CrossRef]
- Lee, S.S.; Kwon, K.B.; Lee, Y.I.; Moon, Y.W. Navigation-Assisted Total Knee Arthroplasty for a Valgus Knee Improves Limb and Femoral Component Alignment. Orthopedics 2019, 42, e253–e259. [Google Scholar] [CrossRef]
- Piovan, G.; Farinelli, L.; Screpis, D.; Iacono, V.; Povegliano, L.; Bonomo, M.; Auregli, L.; Zorzi, C. Distal femoral osteotomy versus lateral unicompartmental arthroplasty for isolated lateral tibiofemoral osteoarthritis with intra-articular and extra-articular deformity: A propensity score-matched analysis. Knee Surg. Relat. Res. 2022, 34, 34. [Google Scholar] [CrossRef]
- Makiev, K.G.; Vasios, I.S.; Georgoulas, P.; Tilkeridis, K.; Drosos, G.; Ververidis, A. Clinical significance and management of meniscal extrusion in different knee pathologies: A comprehensive review of the literature and treatment algorithm. Knee Surg. Relat. Res. 2022, 34, 35. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.W.; Park, C.H.; Bae, D.K.; Song, S.J. How much preoperative flexion contracture is a predictor for residual flexion contracture after total knee arthroplasty in hemophilic arthropathy and rheumatoid arthritis? Knee Surg. Relat. Res. 2022, 34, 20. [Google Scholar] [CrossRef]
- Lee, J.M.; Ha, C.; Jung, K.; Choi, W. Clinical Results after Design Modification of Lospa Total Knee Arthroplasty System: Comparison between Posterior-Stabilized (PS) and PS Plus Types. Clin. Orthop. Surg. 2022, 14, 236–243. [Google Scholar] [CrossRef]
- Insall, J.N.; Ranawat, C.S.; Aglietti, P.; Shine, J. A comparison of four models of total knee-replacement prostheses. J. Bone Joint Surg. Am. 1976, 58, 754–765. [Google Scholar] [CrossRef] [PubMed]
- Stucki, G.; Meier, D.; Stucki, S.; Michel, B.A.; Tyndall, A.G.; Dick, W.; Theiler, R. Evaluation of a German version of WOMAC (Western Ontario and McMaster Universities) Arthrosis Index. Z Rheumatol. 1996, 55, 40–49. [Google Scholar]
- Maniar, R.N.; Bhatnagar, N.; Bidwai, R.; Dhiman, A.; Chanda, D.; Sanghavi, N. Comparison of Patellofemoral Outcomes between Attune and PFC Sigma Designs: A Prospective Matched-Pair Analysis. Clin. Orthop. Surg. 2022, 14, 96–104. [Google Scholar] [CrossRef]
- Seo, J.G.; Moon, Y.W.; Park, S.H.; Kang, H.M.; Kim, S.M. How precise is the identification of the center of the femoral head during total knee arthroplasty? Acta Orthop. 2012, 83, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Dennis, D.A.; Channer, M.; Susman, M.H.; Stringer, E.A. Intramedullary versus extramedullary tibial alignment systems in total knee arthroplasty. J. Arthroplast. 1993, 8, 43–47. [Google Scholar] [CrossRef]
- Teter, K.E.; Bregman, D.; Colwell, C.W., Jr. Accuracy of intramedullary versus extramedullary tibial alignment cutting systems in total knee arthroplasty. Clin. Orthop. Relat. Res. 1995, 321, 106–110. [Google Scholar] [CrossRef]
- Ko, P.S.; Tio, M.K.; Ban, C.M.; Mak, Y.K.; Ip, F.K.; Lam, J.J. Radiologic analysis of the tibial intramedullary canal in Chinese varus knees: Implications in total knee arthroplasty. J. Arthroplast. 2001, 16, 212–215. [Google Scholar] [CrossRef]
- Nishikawa, K.; Mizu-uchi, H.; Okazaki, K.; Matsuda, S.; Tashiro, Y.; Iwamoto, Y. Accuracy of Proximal Tibial Bone Cut Using Anterior Border of Tibia as Bony Landmark in Total Knee Arthroplasty. J. Arthroplast. 2015, 30, 2121–2124. [Google Scholar] [CrossRef] [PubMed]
- Oh, S.M.; Bin, S.I.; Kim, J.Y.; Lee, B.S.; Kim, J.M. Impact of preoperative varus deformity on postoperative mechanical alignment and long-term results of “mechanical” aligned total knee arthroplasty. Orthop. Traumatol. Surg. Res. 2019, 105, 1061–1066. [Google Scholar] [CrossRef] [PubMed]
- Ahn, J.H.; Back, Y.W. Comparative Study of Two Techniques for Ligament Balancing in Total Knee Arthroplasty for Severe Varus Knee: Medial Soft Tissue Release vs. Bony Resection of Proximal Medial Tibia. Knee Surg. Relat. Res. 2013, 25, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.M.; Kim, K.W.; Cha, S.M.; Han, K.Y. Proximal tibial resection in varus-deformed tibiae during total knee arthroplasty: An in vitro study using sawbone model. Int. Orthop. 2015, 39, 429–434. [Google Scholar] [CrossRef]




| Age, year a | 70.55 ± 7.21 |
| Sex, male:female | 46:174 |
| Direction, right:left | 107:113 |
| Proximal tibial reference point | |
| Center | 157 (71.4%) |
| In-between | 24 (10.9%) |
| Lateral tibial spine | 39 (17.7%) |
| Pre-Operation | Post-Operation | p Value | |
|---|---|---|---|
| HKA alignment, ° | 10.4 ± 6.4 | 1.9 ± 1.7 | <0.001 |
| MPTA, ° | 83.9 ± 3.3 | 90.1 ± 0.9 | <0.001 |
| Tibial slope, ° | 9.3 ± 4.4 | 3.2 ± 2.1 | <0.001 |
| HSS score | 38.7 ± 11.9 | 77.7 ± 9.9 | <0.001 |
| WOMAC index | 68.0 ± 7.1 | 28.2 ± 5.4 | <0.001 |
| Mild Varus Group (<10°) | Severe Varus Group (≥10°) | p Value | |
|---|---|---|---|
| Number of cases | 111 | 109 | |
| Age | 70.2 ± 7.0 | 70.8 ± 7.4 | 0.517 |
| Direction (R:L) | 57:54 | 50:59 | 0.422 |
| Pre-operative HKA alignment (°) | 5.7 ± 2.5 | 15.0 ± 5.8 | <0.001 |
| Post-operative HKA alignment (°) | 1.4 ± 1.7 | 2.4 ± 2.1 | <0.001 |
| HKA alignment outliers, n (%) | 6 (5.4%) | 15 (13.8%) | 0.04 |
| Pre-operative MPTA (°) | 85.1 ± 2.9 | 82.7 ± 3.1 | <0.001 |
| Post-operative MPTA (°) | 90.2 ± 0.8 | 90.1 ± 1.0 | 0.654 |
| MPTA outliers, n (%) | 1 (0.9%) | 2 (1.5%) | 0.62 |
| Pre-operative tibial slope (°) | 8.8 ± 4.5 | 9.9 ± 4.3 | 0.065 |
| Post-operative tibial slope (°) | 3.1 ± 2.0 | 3.4 ± 2.3 | 0.394 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cho, J.-H.; Choi, J.Y.; Lee, S.-S. Accuracy of the Tibial Component Alignment by Extramedullary System Using Simple Radiographic References in Total Knee Arthroplasty. Medicina 2022, 58, 1212. https://doi.org/10.3390/medicina58091212
Cho J-H, Choi JY, Lee S-S. Accuracy of the Tibial Component Alignment by Extramedullary System Using Simple Radiographic References in Total Knee Arthroplasty. Medicina. 2022; 58(9):1212. https://doi.org/10.3390/medicina58091212
Chicago/Turabian StyleCho, Jin-Ho, Jun Young Choi, and Sung-Sahn Lee. 2022. "Accuracy of the Tibial Component Alignment by Extramedullary System Using Simple Radiographic References in Total Knee Arthroplasty" Medicina 58, no. 9: 1212. https://doi.org/10.3390/medicina58091212
APA StyleCho, J.-H., Choi, J. Y., & Lee, S.-S. (2022). Accuracy of the Tibial Component Alignment by Extramedullary System Using Simple Radiographic References in Total Knee Arthroplasty. Medicina, 58(9), 1212. https://doi.org/10.3390/medicina58091212








