A Life-Threatening Infection after Endobronchial Ultrasound Transbronchial Lung Biopsy with Guide Sheath: A Case Report
Abstract
:1. Introduction
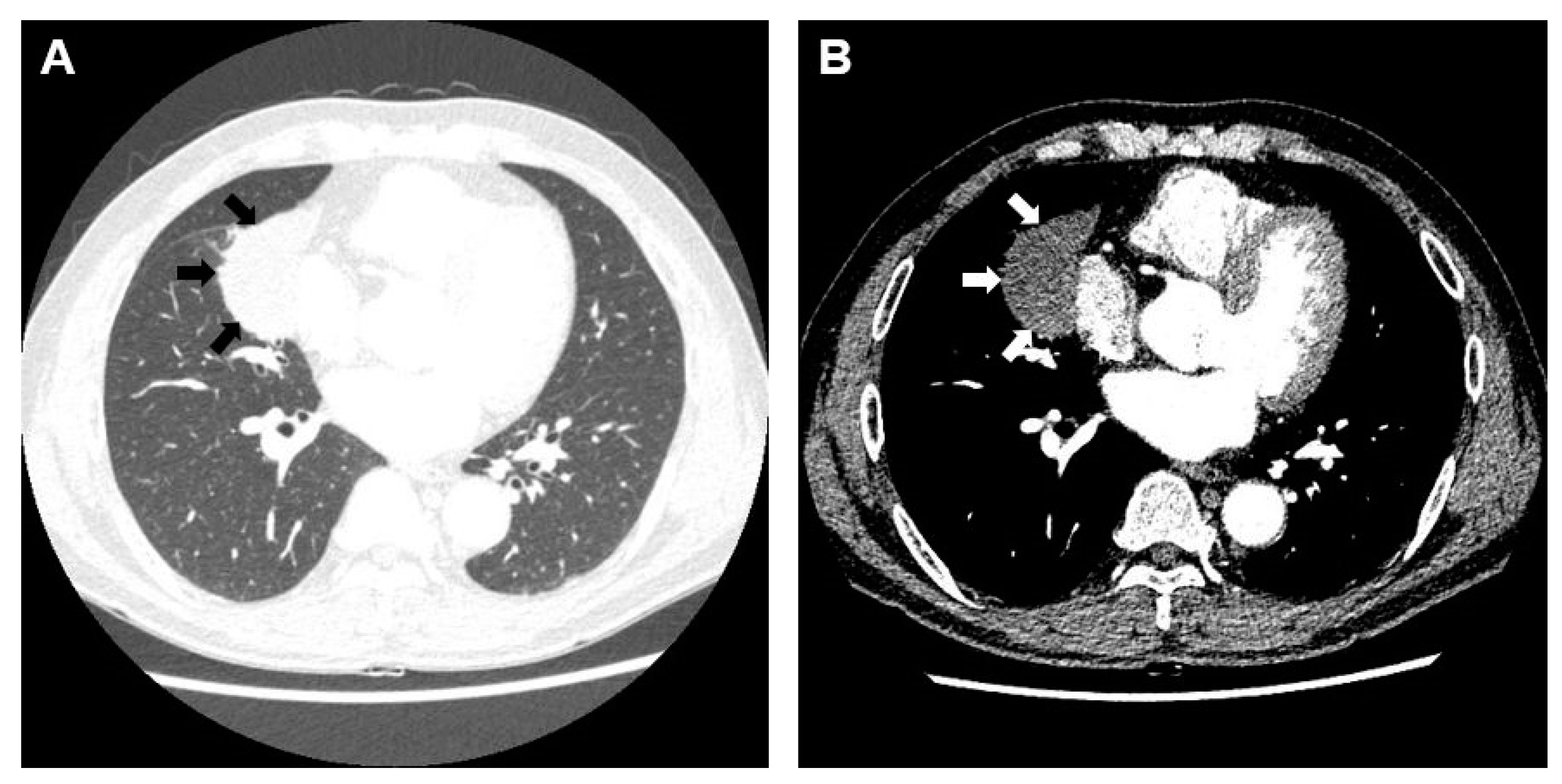
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Aberle, D.R.; Adams, A.M.; Berg, C.D.; Black, W.C.; Clapp, J.D.; Fagerstrom, R.M.; Gareen, I.F.; Gatsonis, C.; Marcus, P.M.; Sicks, J.D. Reduced lung-cancer mortality with low-dose computed tomographic screening. N. Engl. J. Med. 2011, 365, 395–409. [Google Scholar] [CrossRef] [PubMed]
- Steinfort, D.P.; Khor, Y.H.; Manser, R.L.; Irving, L.B. Radial probe endobronchial ultrasound for the diagnosis of peripheral lung cancer: Systematic review and meta-analysis. Eur. Respir. J. 2011, 37, 902–910. [Google Scholar] [CrossRef] [PubMed]
- Wang Memoli, J.S.; Nietert, P.J.; Silvestri, G.A. Meta-analysis of guided bronchoscopy for the evaluation of the pulmonary nodule. Chest 2012, 142, 385–393. [Google Scholar] [CrossRef] [PubMed]
- Hayama, M.; Izumo, T.; Matsumoto, Y.; Chavez, C.; Tsuchida, T.; Sasada, S. Complications with Endobronchial Ultrasound with a Guide Sheath for the Diagnosis of Peripheral Pulmonary Lesions. Respiration 2015, 90, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Kurimoto, N.; Miyazawa, T.; Okimasa, S.; Maeda, A.; Oiwa, H.; Miyazu, Y.; Murayama, M. Endobronchial ultrasonography using a guide sheath increases the ability to diagnose peripheral pulmonary lesions endoscopically. Chest 2004, 126, 959–965. [Google Scholar] [CrossRef] [PubMed]
- Du Rand, I.A.; Blaikley, J.; Booton, R.; Chaudhuri, N.; Gupta, V.; Khalid, S.; Mandal, S.; Martin, J.; Mills, J.; Navani, N.; et al. British Thoracic Society guideline for diagnostic flexible bronchoscopy in adults: Accredited by NICE. Thorax 2013, 68, i1–i44. [Google Scholar] [CrossRef] [PubMed]
- Souma, T.; Minezawa, T.; Yatsuya, H.; Okamura, T.; Yamatsuta, K.; Morikawa, S.; Horiguchi, T.; Maeda, S.; Goto, Y.; Hayashi, M.; et al. Risk Factors of Infectious Complications After Endobronchial Ultrasound-Guided Transbronchial Biopsy. Chest 2020, 158, 797–807. [Google Scholar] [CrossRef] [PubMed]
- Shimoda, M.; Yamana, K.; Yano, R.; Saitou, M.; Fujiwara, K.; Furuuchi, K.; Osawa, T.; Uesugi, F.; Arakawa, K.; Morimoto, K.; et al. Analysis of risk factors for the development of a post-bronchoscopy respiratory infection in lung cancer patients. J. Infect. Chemother. 2021, 27, 237–242. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, I.; Oh, Y.; Lee, M.K.; Eom, J.S. A Life-Threatening Infection after Endobronchial Ultrasound Transbronchial Lung Biopsy with Guide Sheath: A Case Report. Medicina 2022, 58, 1275. https://doi.org/10.3390/medicina58091275
Kim I, Oh Y, Lee MK, Eom JS. A Life-Threatening Infection after Endobronchial Ultrasound Transbronchial Lung Biopsy with Guide Sheath: A Case Report. Medicina. 2022; 58(9):1275. https://doi.org/10.3390/medicina58091275
Chicago/Turabian StyleKim, Insu, Yeseul Oh, Min Ki Lee, and Jung Seop Eom. 2022. "A Life-Threatening Infection after Endobronchial Ultrasound Transbronchial Lung Biopsy with Guide Sheath: A Case Report" Medicina 58, no. 9: 1275. https://doi.org/10.3390/medicina58091275




