Innovative C-Arm-Free Navigation Technique for Posterior Spinal Fixation for Atlantoaxial Subluxation: A Technical Note
Abstract
:1. Introduction
2. Case Presentation
2.1. Patient History
2.2. Physical Examination
2.3. Preoperative Imaging
2.4. Surgery
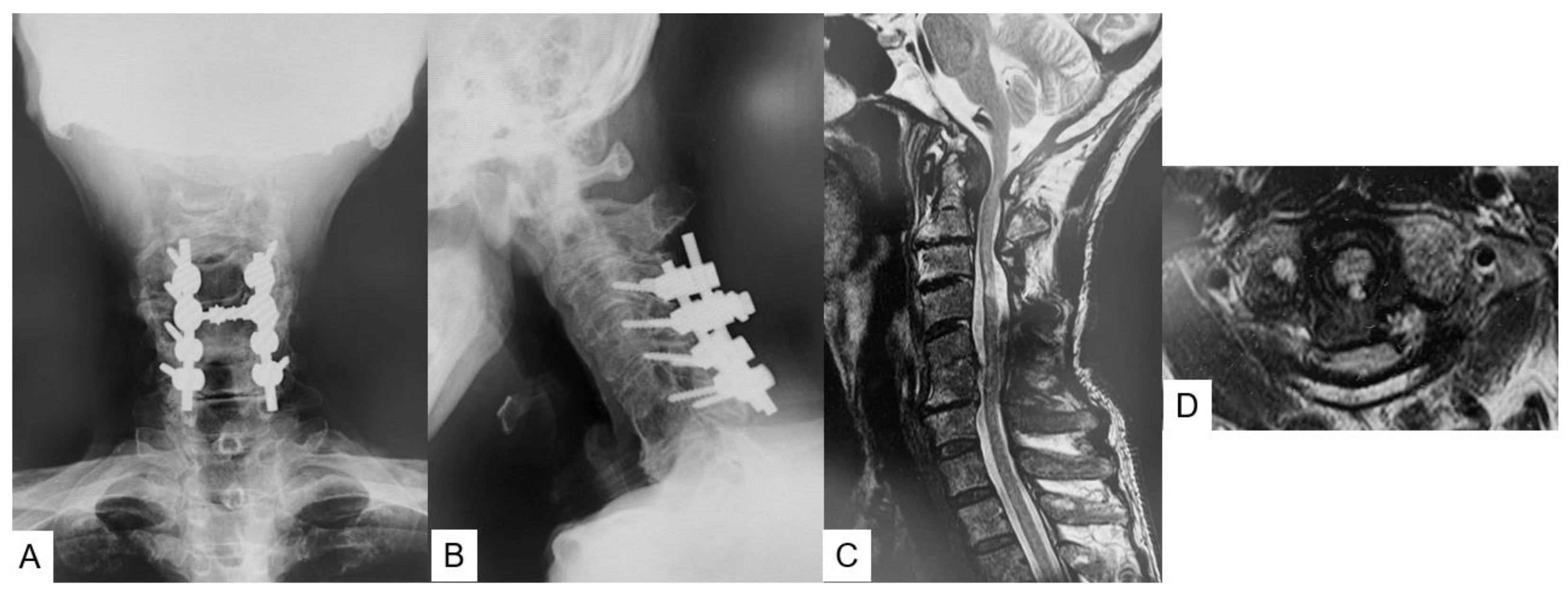
2.5. Postoperative Imaging
2.6. One Year Follow-Up
3. Operative Procedure
3.1. Patient Positioning and Exposure
3.2. C2 Pedicle Screw
3.3. C1 LMS
3.4. Reduction and Bone Graft
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mizutani, J.; Inada, A.; Kato, K.; Kondo, A.; Kainuma, S.; Fujita, K.; Yagi, K.; Shimamura, Y.; Fukuoka, M.; Shibamoto, Y.; et al. Advantages of an on-the-screwhead crosslink connector for atlantoaxial fixation using the Goel/Harms technique. J. Clin. Neurosci. 2018, 50, 183–189. [Google Scholar] [CrossRef] [PubMed]
- Magerl, F.; Seemann, P.S. Stable posterior fusion of the atlas and axis by transarticular screw fixation. In Cervical Spine I; Kehr, P., Weidner, A., Eds.; Springer: New York, NY, USA, 1987; Volume 1, pp. 322–327. [Google Scholar]
- Goel, A.; Laheri, V. Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir. 1994, 129, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Wright, N.M. Posterior C2 fixation using bilateral, crossing C2 laminar screws: Case series and technical note. J. Spinal Disord. Tech. 2004, 17, 158–162. [Google Scholar] [CrossRef] [PubMed]
- Harms, J.; Melcher, R.P. Posterior C1–C2 fusion with polyaxial screw and rod fixation. Spine 2001, 26, 2467–2471. [Google Scholar] [CrossRef] [PubMed]
- Grob, D.; Crisco, J.J., 3rd; Panjabi, M.M.; Wang, P.; Dvorak, J. Biomechanical evaluation of four different posterior atlantoaxial fixation techniques. Spine (Phila Pa 1976) 1992, 17, 480–490. [Google Scholar] [CrossRef]
- Lee, M.J.; Cassinelli, E.; Riew, K.D. The feasibility of inserting atlas lateral mass screws via the posterior arch. Spine 2006, 31, 2798–27801. [Google Scholar] [CrossRef]
- Lee, S.; Hur, J.W.; Lee, J.B.; Park, J.H.; Park, D.; Park, S.J.; Kim, K.T.; Cho, D.C. Radiological evaluation of atlantoaxial fusion using C2 translaminar screws and C2 pedicle screws: Does the screw halo sign imply fusion failure? Medicine 2022, 101, e31496. [Google Scholar] [CrossRef]
- Liu, G.; Buchowski, J.M.; Shen, H.; Yeom, J.S.; Riew, K.D. The feasibility of microscopeassisted “free-hand” C1 lateral mass screw insertion without fluoroscopy. Spine 2008, 33, 1042–1049. [Google Scholar] [CrossRef]
- Mummaneni, P.V.; Lu, D.C.; Dhall, S.S.; Mummaneni, V.P.; Chou, D. C1 lateral mass fixation: A comparison of constructs. Neurosurgery 2010, 66 (Suppl. 3), 153–160. [Google Scholar] [CrossRef]
- Tan, M.; Wang, H.; Wang, Y.; Zhang, G.; Yi, P.; Li, Z.; Wei, H.; Yang, F. Morphometric evaluation of screw fixation in atlas via posterior arch and lateral mass. Spine 2003, 28, 888–895. [Google Scholar] [CrossRef]
- Gan, G.; Kaliya-Perumal, A.K.; Yu, C.S.; Nolan, C.P.; Oh, J.Y. Spinal Navigation for Cervical Pedicle Screws: Surgical Pearls and Pitfalls. Global Spine J. 2021, 11, 196–202. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tanaka, M.; Fujiwara, Y.; Uotani, K.; Kadiri, V.; Yamauchi, T. C-Arm-Free Minimally Invasive Cervical Pedicle Screw Fixation (MICEPS): A Technical Note. Acta Med. Okayama. 2020, 74, 551–556. [Google Scholar] [CrossRef] [PubMed]
- Bahadur, R.; Goyal, T.; Dhatt, S.S.; Tripathy, S.K. Transarticular screw fixation for atlantoaxial instability—Modified Magerl’s technique in 38 patients. J. Orthop. Surg. Res. 2010, 5, 87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andermatten, J.A.; Elua Pinin, A.; Samprón Lebed, N.; Armendariz Guezala, M.; Arrazola Schlamilch, M.; Úrculo Bareño, E. Atlantoaxial subluxation secondary to retropharyngeal abcess in adults (Grisel’s syndrome). Review of literature about a clinical case. Neurocirugia 2020, 31, 201–205. [Google Scholar] [CrossRef] [PubMed]
- Kanai, M.; Kawano, K.; Murakami, T. Atlanto-axial subluxation posssibly due to eosinophilic granuloma of the axis: A case report. Neurol. Surg. 2004, 32, 1253–1260. (In Japanese) [Google Scholar]
- Rath, G.P.; Singh, D.; Prabhakar, H.; Bithal, P.K. Symptomatic atlantoaxial dislocation in Marfan’s syndrome: Anaesthetic considerations. Eur. J. Anaesthesiol. 2007, 24, 1058–1060. [Google Scholar] [CrossRef]
- Ali, F.E.; Al-Bustan, M.A.; Al-Busairi, W.A.; Al-Mulla, F.A.; Esbaita, E.Y. Cervical spine abnormalities associated with down syndrome. Int. Orthop. 2006, 30, 284–289. [Google Scholar] [CrossRef] [Green Version]
- Singh, D.K.; Pathak, V.; Singh, N.; Singh, R.K.; Kaif, M.; Yadav, K. C1 lateral mass reduction screws for treating atlantoaxial dislocations: Bringing ease by modification. J. Craniovert. Jun. Spine 2022, 13, 140–145. [Google Scholar] [CrossRef]
- Klepinowski, T.; Limanówka, B.; Sagan, L. Management of post-traumatic craniovertebral junction dislocation: A PRISMA-compliant systematic review and meta-analysis of casereports. Neurosurg. Rev. 2021, 44, 1391–1400. [Google Scholar] [CrossRef]
- Liu, J.; Zhu, L.; Jiang, E.; Zou, S.; Xu, G. Ankylosing Spondylitis Manifested by Extensive Cervical Erosions with Spontaneous Anterior Atlantoaxial Subluxation. World Neurosurg. 2019, 122, 583–589. [Google Scholar] [CrossRef]
- Kauppi, M.; Leppänen, L.; Heikkilä, S.; Lahtinen, T.; Kautiainen, H. Active conservative treatment of atlantoaxial subluxation in rheumatoid arthritis. Br. J. Rheumatol. 1998, 37, 417–420. [Google Scholar] [CrossRef] [PubMed]
- Robinson, H.S. Rheumatoid arthritis—Atlanto-axial subluxation and its clinical presentation. Can. Med. Assoc. J. 1966, 94, 470–477. [Google Scholar] [PubMed]
- Guyard, T.; Le Quellec, A.; Garrigues, F.; Saraux, A. Reproducibility and diagnostic value of a new method using ratios to diagnose anterior atlanto-axial subluxation on plain radiographs. Jt. Bone Spine 2021, 88, 105229. [Google Scholar] [CrossRef] [PubMed]
- Shih, Y.T.; Kao, T.H.; Pan, H.C.; Chen, H.T.; Tsou, H.K. The Surgical Treatment Principles of Atlantoaxial Instability Focusing on Rheumatoid Arthritis. Biomed. Res. Int. 2015, 2015, 518164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ranawat, C.S.; O’Leary, P.; Pellicci, P.; Tsairis, P.; Marchisello, P.; Dorr, L. Cervical spine fusion in rheumatoid arthritis. J. Bone Jt. Surg. Am. 1979, 61, 1003–1010. [Google Scholar] [CrossRef]
- Yonenobu, K.; Abumi, K.; Nagata, K.; Taketomi, E.; Ueyama, K. Interobserver and intraobserver reliability of the japanese orthopaedic association scoring system for evaluation of cervical compression myelopathy. Spine (Phila Pa 1976) 2001, 26, 1890–1894. [Google Scholar] [CrossRef]
- Gallie, W.E. Fractures and dislocations of the cervical spine. Am. J. Surg. 1939, 46, 495–499. [Google Scholar] [CrossRef]
- Kleinstück, F.S.; Fekete, T.F.; Loibl, M.; Jeszenszky, D.; Haschtmann, D.; Porchet, F.; Mannion, A.F. Patient-rated outcome after atlantoaxial (C1-C2) fusion: More than a decade of evaluation of 2-year outcomes in 126 patients. Eur. Spine J. 2021, 30, 3620–3630. [Google Scholar] [CrossRef]
- Guo, J.; Lu, W.; Ji, X.; Ren, X.; Tang, X.; Zhao, Z.; Hu, H.; Song, T.; Du, Y.; Li, J.; et al. Surgical treatment of atlantoaxial subluxation by intraoperative skull traction and C1-C2 fixation. BMC Musculoskelet. Disord. 2020, 21, 239. [Google Scholar] [CrossRef]
- Maruo, Y.; Maruo, Y. The Comparison between O-Arm Navigation System and C-Arm Fluoroscopy Navigation System for the Amount of Radiation Exposure in Balloon Kyphoplasty. Global Spine J. 2016, 6. [Google Scholar] [CrossRef]
- Tanaka, M.; Suthar, H.; Fujiwara, Y.; Oda, Y.; Uotani, K.; Arataki, S.; Yamauchi, T.; Misawa, H. Intraoperative O-arm navigation guided anterior cervical surgery; A technical note and case series. Interdis Neurosurg. 2021, 26, 101288. [Google Scholar] [CrossRef]
- Lee, H.R.; Lee, D.H.; Cho, J.H.; Hwang, E.S.; Seok, S.Y.; Park, S.; Lee, C.S. Feasibility of lateral mass screw insertion in patients with the risky triad of C1: Evaluation of the over-the-arch technique. J. Neurosurg. Spine 2021, 26, 1–8. [Google Scholar] [CrossRef] [PubMed]






Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tanaka, M.; Sake, N.; Kim, D.-G.; Arataki, S.; Desai, D.; Fujiwara, Y.; Yamauchi, T. Innovative C-Arm-Free Navigation Technique for Posterior Spinal Fixation for Atlantoaxial Subluxation: A Technical Note. Medicina 2023, 59, 11. https://doi.org/10.3390/medicina59010011
Tanaka M, Sake N, Kim D-G, Arataki S, Desai D, Fujiwara Y, Yamauchi T. Innovative C-Arm-Free Navigation Technique for Posterior Spinal Fixation for Atlantoaxial Subluxation: A Technical Note. Medicina. 2023; 59(1):11. https://doi.org/10.3390/medicina59010011
Chicago/Turabian StyleTanaka, Masato, Naveen Sake, Dae-Geun Kim, Shinya Arataki, Dhvanit Desai, Yoshihiro Fujiwara, and Taro Yamauchi. 2023. "Innovative C-Arm-Free Navigation Technique for Posterior Spinal Fixation for Atlantoaxial Subluxation: A Technical Note" Medicina 59, no. 1: 11. https://doi.org/10.3390/medicina59010011





