Combined Humeral Head and Shaft Fractures: Outcome Following Intramedullary Nailing and Plating
Abstract
:1. Introduction
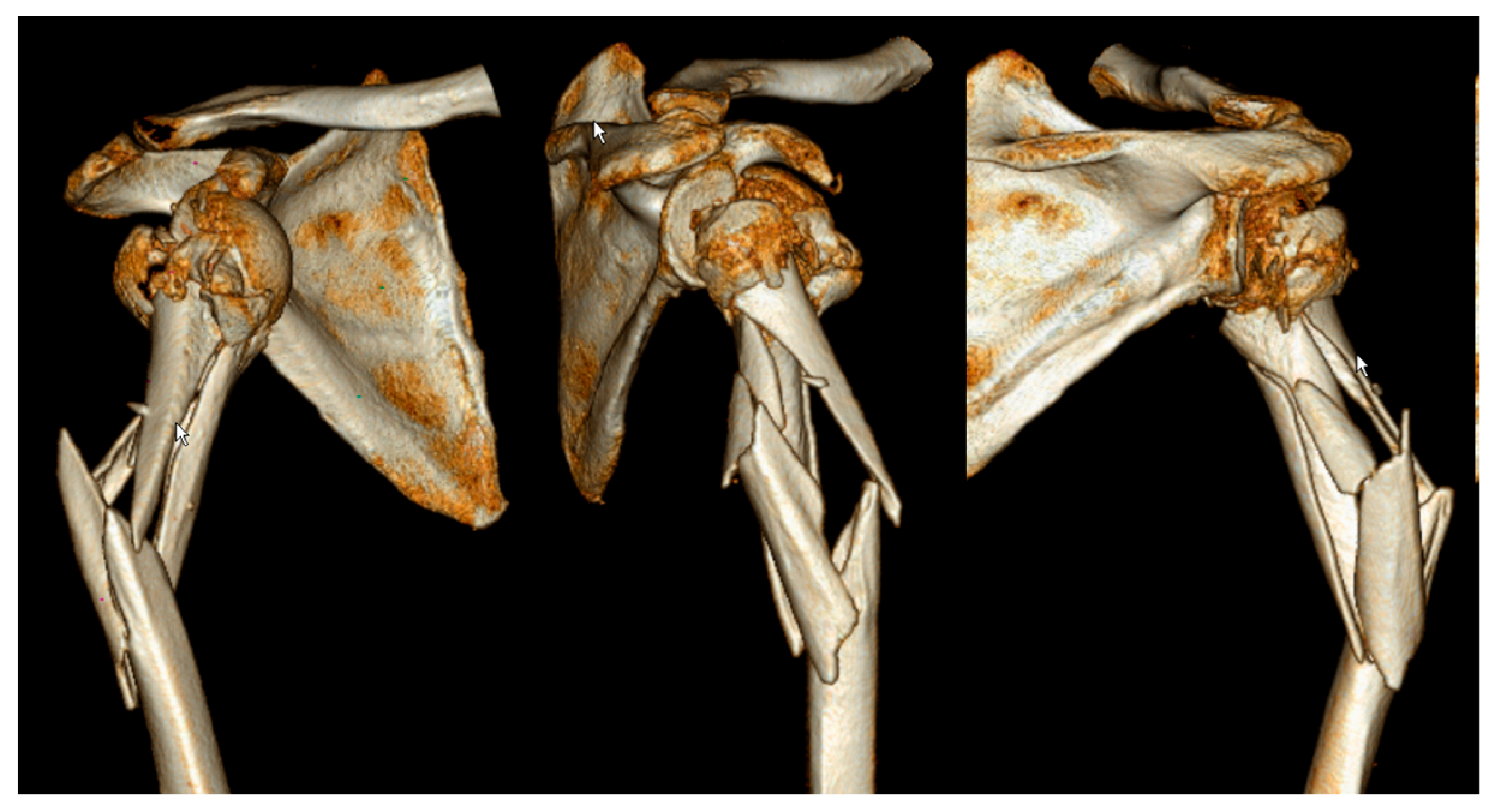
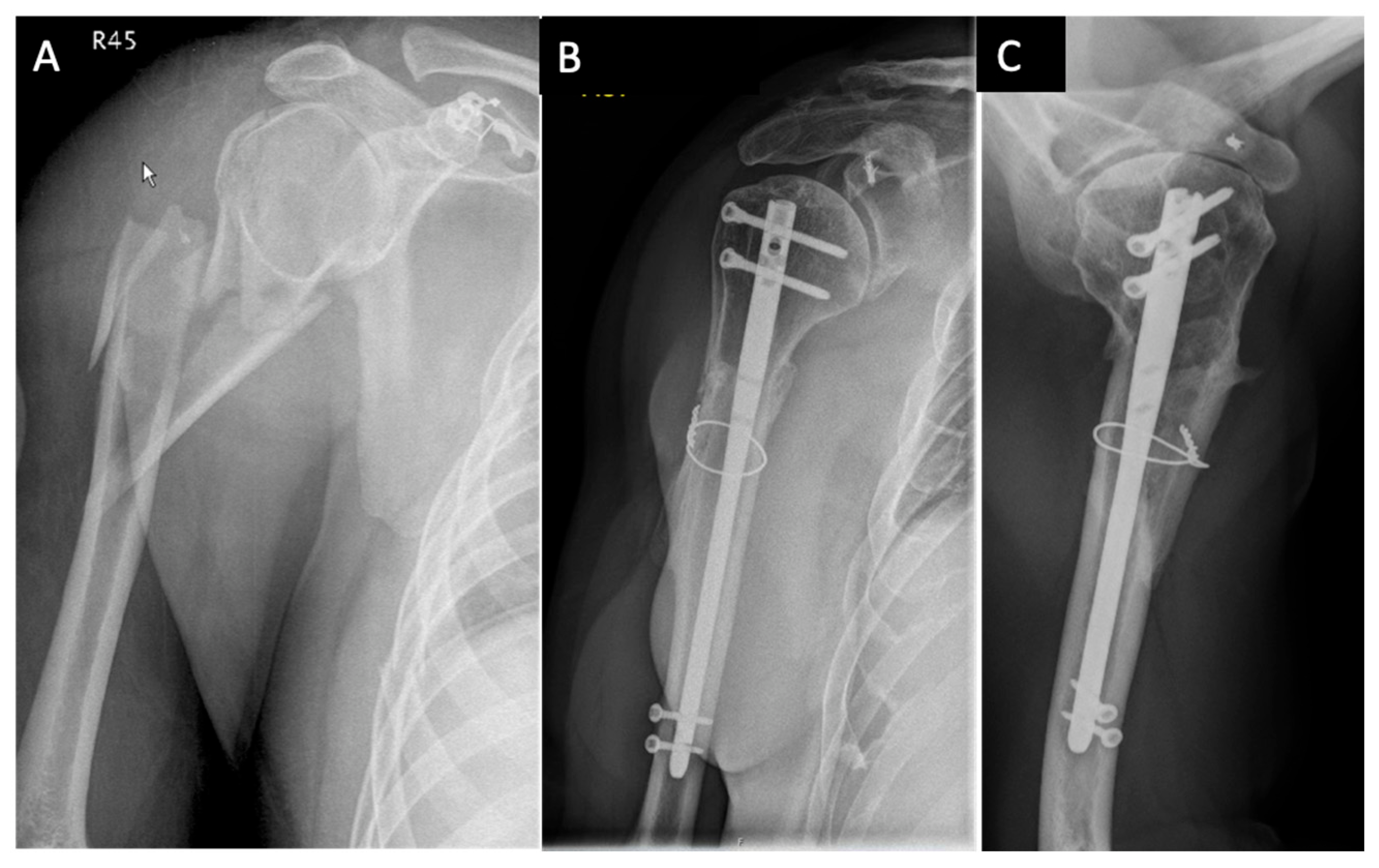
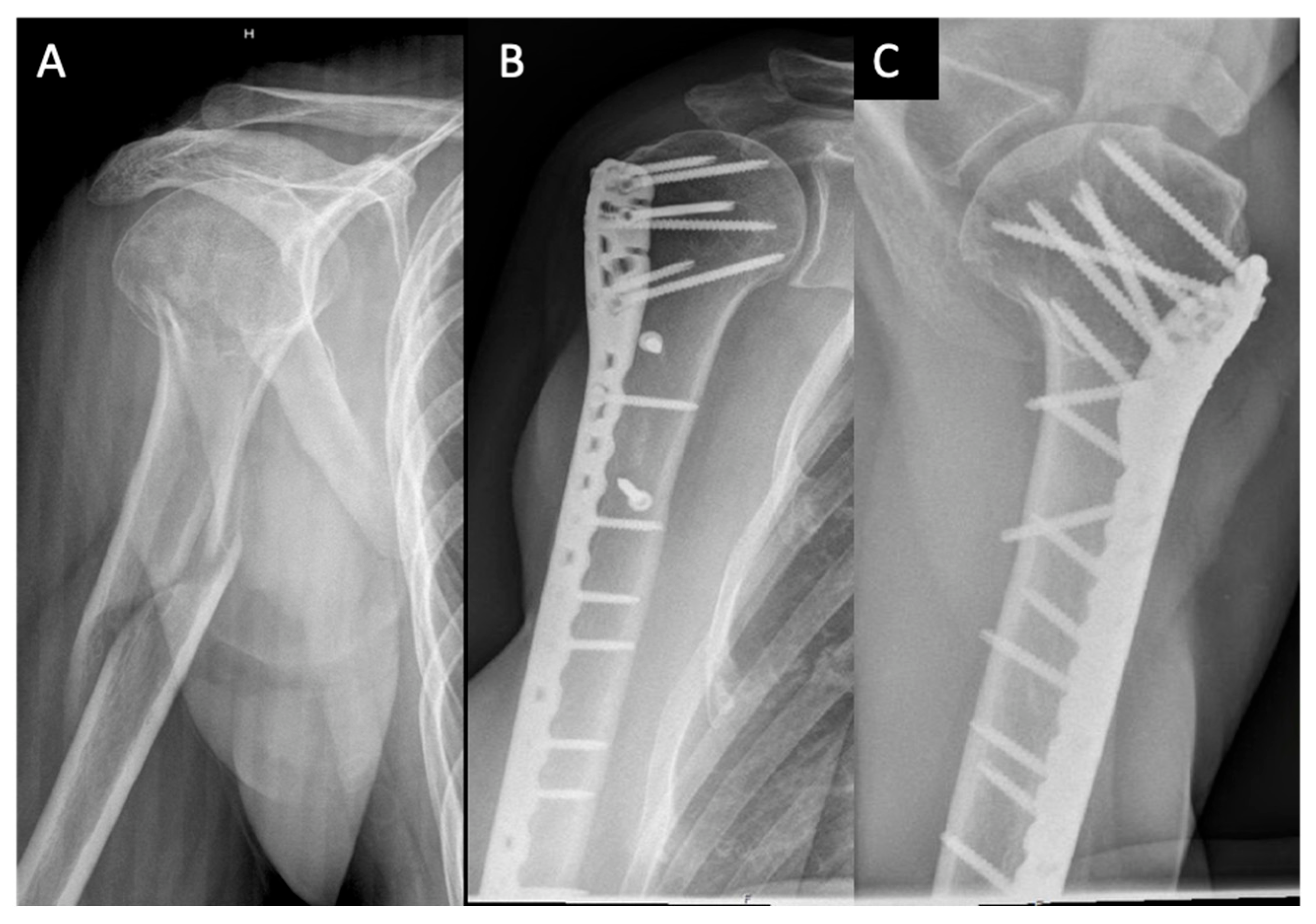
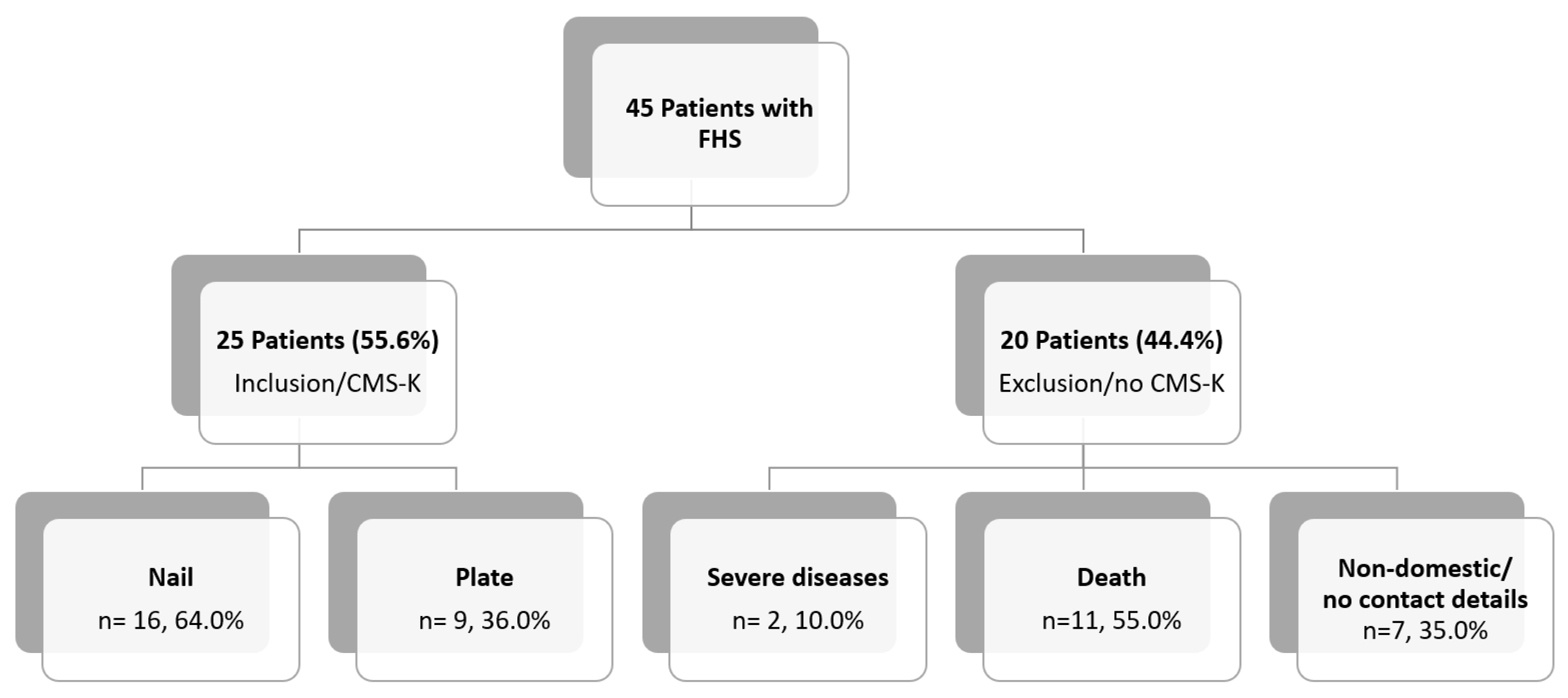
2. Materials and Methods
2.1. Patients
2.2. Baseline Data Acquisition
2.3. Surgical Procedure
2.4. Outcome
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Court-Brown, C.M.; Caesar, B. Epidemiology of Adult Fractures: A Review. Injury 2006, 37, 691–697. [Google Scholar] [CrossRef] [PubMed]
- Hepp, P.; Theopold, J.; Osterhoff, G.; Marquass, B.; Voigt, C.; Josten, C. Bone Quality Measured by the Radiogrammetric Parameter “Cortical Index” and Reoperations after Locking Plate Osteosynthesis in Patients Sustaining Proximal Humerus Fractures. Arch. Orthop. Trauma Surg. 2009, 129, 1251–1259. [Google Scholar] [CrossRef]
- Hertel, R. Fractures of the Proximal Humerus in Osteoporotic Bone. Osteoporos Int. 2005, 16 (Suppl S2), S65–S72. [Google Scholar] [CrossRef] [PubMed]
- Lill, H.; Ellwein, A.; Katthagen, C.; Voigt, C. Osteoporotic fractures of the proximal humerus. Chirurg 2012, 83, 858–865. [Google Scholar] [CrossRef] [PubMed]
- Yang, K.H. Helical Plate Fixation for Treatment of Comminuted Fractures of the Proximal and Middle One-Third of the Humerus. Injury 2005, 36, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Garnavos, C.; Lasanianos, N. Intramedullary Nailing of Combined/Extended Fractures of the Humeral Head and Shaft. J. Orthop. Trauma 2010, 24, 199–206. [Google Scholar] [CrossRef]
- Stedtfeld, H.W.; Biber, R. Proximal Third Humeral Shaft Fractures -- a Fracture Entity Not Fully Characterized by Conventional AO Classification. Injury 2014, 45 (Suppl. S1), S54–S59. [Google Scholar] [CrossRef]
- Handoll, H.H.; Brorson, S. Interventions for Treating Proximal Humeral Fractures in Adults. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef] [Green Version]
- Königshausen, M.; Kübler, L.; Godry, H.; Citak, M.; Schildhauer, T.A.; Seybold, D. Clinical Outcome and Complications Using a Polyaxial Locking Plate in the Treatment of Displaced Proximal Humerus Fractures. A Reliable System? Injury 2012, 43, 223–231. [Google Scholar] [CrossRef]
- Brorson, S.; Rasmussen, J.V.; Frich, L.H.; Olsen, B.S.; Hróbjartsson, A. Benefits and Harms of Locking Plate Osteosynthesis in Intraarticular (OTA Type C) Fractures of the Proximal Humerus: A Systematic Review. Injury 2012, 43, 999–1005. [Google Scholar] [CrossRef]
- Rancan, M.; Dietrich, M.; Lamdark, T.; Can, U.; Platz, A. Minimal Invasive Long PHILOS®-Plate Osteosynthesis in Metadiaphyseal Fractures of the Proximal Humerus. Injury 2010, 41, 1277–1283. [Google Scholar] [CrossRef]
- Neer, C.S. Displaced Proximal Humeral Fractures. II. Treatment of Three-Part and Four-Part Displacement. J. Bone Joint. Surg. Am. 1970, 52, 1090–1103. [Google Scholar] [CrossRef]
- Meinberg, E.; Agel, J.; Roberts, C.; Karam, M.; Kellam, J. Fracture and Dislocation Classification Compendium—2018. J. Orthop. Trauma 2018, 32, S1–S10. [Google Scholar] [CrossRef]
- Katolik, L.I.; Romeo, A.A.; Cole, B.J.; Verma, N.N.; Hayden, J.K.; Bach, B.R. Normalization of the Constant Score. J. Shoulder Elbow Surg. 2005, 14, 279–285. [Google Scholar] [CrossRef]
- Resch, H. Proximal Humeral Fractures: Current Controversies. J. Shoulder Elb. Surg. 2011, 20, 827–832. [Google Scholar] [CrossRef]
- Clement, N.D.; Duckworth, A.D.; McQueen, M.M.; Court-Brown, C.M. The Outcome of Proximal Humeral Fractures in the Elderly: Predictors of Mortality and Function. Bone Joint J. 2014, 96-B, 970–977. [Google Scholar] [CrossRef]
- Bahrs, C.; Stojicevic, T.; Tanja, S.; Blumenstock, G.; Gunnar, B.; Brorson, S.; Stig, B.; Badke, A.; Stöckle, U.; Ulrich, S.; et al. Trends in Epidemiology and Patho-Anatomical Pattern of Proximal Humeral Fractures. Int. Orthop. 2014, 38, 1697–1704. [Google Scholar] [CrossRef] [Green Version]
- Konrad, G.; Hirschmüller, A.; Audige, L.; Lambert, S.; Hertel, R.; Südkamp, N.P. Comparison of Two Different Locking Plates for Two-, Three- and Four-Part Proximal Humeral Fractures--Results of an International Multicentre Study. Int. Orthop. 2012, 36, 1051–1058. [Google Scholar] [CrossRef] [Green Version]
- Gradl, G.; Dietze, A.; Kääb, M.; Hopfenmüller, W.; Mittlmeier, T. Is Locking Nailing of Humeral Head Fractures Superior to Locking Plate Fixation? Clin. Orthop. Relat Res. 2009, 467, 2986–2993. [Google Scholar] [CrossRef] [Green Version]
- Zhu, Y.; Lu, Y.; Shen, J.; Zhang, J.; Jiang, C. Locking Intramedullary Nails and Locking Plates in the Treatment of Two-Part Proximal Humeral Surgical Neck Fractures: A Prospective Randomized Trial with a Minimum of Three Years of Follow-Up. J. Bone Joint Surg. Am. 2011, 93, 159–168. [Google Scholar] [CrossRef]
- Schader, J.F.; Mischler, D.; Dauwe, J.; Richards, R.G.; Gueorguiev, B.; Varga, P. One Size May Not Fit All: Patient-Specific Computational Optimization of Locking Plates for Improved Proximal Humerus Fracture Fixation. J. Shoulder Elb. Surg. 2022, 31, 192–200. [Google Scholar] [CrossRef] [PubMed]
- van Veelen, N.M.; Beeres, F.J.; Link, B.-C.; Babst, R. Augmentation in the treatment of proximal humeral and femoral fractures. Unfallchirurgie (Heidelb) 2022, 125, 436–442. [Google Scholar] [CrossRef] [PubMed]
- Caforio, M.; Maniscalco, P.; Colombo, M.; Calori, G.M. Long Endomedullary Nail in Proximal Third Humeral Shaft Fractures. Injury 2016, 47, S64–S70. [Google Scholar] [CrossRef] [PubMed]
- Schliemann, B.; Wähnert, D.; Theisen, C.; Herbort, M.; Kösters, C.; Raschke, M.J.; Weimann, A. How to Enhance the Stability of Locking Plate Fixation of Proximal Humerus Fractures? An Overview of Current Biomechanical and Clinical Data. Injury 2015, 46, 1207–1214. [Google Scholar] [CrossRef] [PubMed]
- Hristov, S.; Visscher, L.; Winkler, J.; Zhelev, D.; Ivanov, S.; Veselinov, D.; Baltov, A.; Varga, P.; Berk, T.; Stoffel, K.; et al. A Novel Technique for Treatment of Metaphyseal Voids in Proximal Humerus Fractures in Elderly Patients. Medicina 2022, 58, 1424. [Google Scholar] [CrossRef]

| Case | Age, years | Sex | Neer | AO/OTA Proximal | AO/OTA Metaphyseal | Stedtfeld | Garnavos/ Lasanianos | Implant/ Metaphyseal Fixation | FU, Months/ CMS-K | Revision |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 65 | M | IV | 11-B1 | 12-C2 | D4 | Combined | Retrograde nail | 48/83 | - |
| 2 | 74 | F | III | 11-A3 | 12-C3 | A2 | Extended | T-nail | 97/51 | Metaphyseal lack of fixation, material removal |
| 3 | 68 | F | IV | 11-B1 | 12-C1 | D2 | Extended | T-nail | 32/71 | Metaphyseal lack of fixation, change to plate |
| 4 | 43 | M | IV | 11-B1 | 12-C3 | D3 | Extended | T-nail/cerclage | 92/77 | - |
| 5 | 74 | F | V | 11-B2 | 12-C1 | B1-3 | Extended | T-nail/screw | 52/64 | - |
| 6 | 65 | M | III | 11-A2 | 12-A1 | A2 | Extended | T-nail/screw | 60/62 | - |
| 7 | 75 | F | III | 11-A2 | 12-C1 | C3 | Extended | T-nail | 91/64 | - |
| 8 | 72 | F | VI | 11-C3 | 12-C3 | D3 | Extended | T-nail/screw | 55/68 | Metaphyseal lack of fixation, inverse prothesis |
| 9 | 55 | F | III | 11-A2 | 12-C1 | B2-1 | Extended | T-nail | 70/99 | - |
| 10 | 67 | F | III | 11-A2 | 12-C1 | C2 | Extended | Locking plate/ cerclage, lag screw | 63/99 | - |
| 11 | 37 | F | IV | 11-B1 | 12-C1 | D3 | Extended | T-nail/screw | 34/86 | - |
| 12 | 50 | F | III | 11-A2 | 12-C1 | C4 | Combined | T-nail/cerclage | 49/97 | - |
| 13 | 76 | F | V | 11-C2 | 12-C2 | D4 | Combined | Locking plate/ lag screw | 58/65 | - |
| 14 | 71 | M | IV | 11-B1 | 12-C1 | D4 | Extended | T-nail/screw | 15/38 | Loss of reduction, proximal nail displacement, material removal |
| 15 | 70 | F | IV | 11-B1 | 12-C2 | D4 | Combined | T-nail/cerclage | 15/70 | - |
| 16 | 23 | M | IV | 11-B2 | 12-C2 | D4 | Combined | Locking plate/ plate | 35/99 | - |
| 17 | 46 | F | V | 11-C2 | 12-C3 | B1-3 | Extended | Locking plate/ lag screw | 57/100 | - |
| 18 | 76 | F | III | 11-A2 | 12-C1 | C2 | Extended | T-nail | 12/72 | - |
| 19 | 53 | F | III | 11-A3 | 12-C3 | C3 | Extended | T-nail/screw | 12/48 | Metaphyseal lack of fixation, change to plate |
| 20 | 53 | F | IV | 11-B1 | 12-A1 | B2-3 | Extended | T-nail | 12/74 | - |
| 21 | 51 | F | IV | 11-B1 | 12-C1 | D2 | Extended | Locking plate/ lag screw | 37/89 | - |
| 22 | 49 | M | V | 11-C2 | 12-C3 | D2 | Combined | Locking plate/ plate | 61/50 | - |
| 23 | 48 | F | V | 11-C2 | 12-C3 | B1-3 | Extended | Locking plate | 45/84 | - |
| 24 | 68 | M | IV | 11-B1 | 12-C1 | B1-2 | Extended | Locking plate/ lag screw | 12/45 | Metaphyseal lack of fixation, pseudarthrosis |
| 25 | 74 | F | III | 11-C1 | 12-C3 | C3 | Extended | Locking plate/ cerclage | 13/62 | - |
| Characteristics | Nail (n = 16) | Plate (n = 9) | p-Value |
|---|---|---|---|
| Age, years | 62.6 ± 12.4 | 55.8 ± 17.0 | 0.33 |
| Sex | 12F, 4M | 6F, 3M | 0.76 |
| High-energy trauma | n = 6, 37.5% | n = 3, 33.3% | – |
| ASA | 2.1 ± 0.7 | 2.2 ± 0.4 | 0.85 |
| Follow-up, months | 46.6 ± 29.9 | 42.3 ± 19.7 | 0.98 |
| CMS-K | 70.3 ± 32.3 | 76.0 ± 31.0 | 0.42 |
| Postoperative revision | n = 5; 31.3% | n = 1; 11.1% | – |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Souleiman, F.; Theopold, J.; Henkelmann, R.; Osterhoff, G.; Pastor, T.; Gueorguiev, B.; Fakler, J.; Hepp, P. Combined Humeral Head and Shaft Fractures: Outcome Following Intramedullary Nailing and Plating. Medicina 2023, 59, 113. https://doi.org/10.3390/medicina59010113
Souleiman F, Theopold J, Henkelmann R, Osterhoff G, Pastor T, Gueorguiev B, Fakler J, Hepp P. Combined Humeral Head and Shaft Fractures: Outcome Following Intramedullary Nailing and Plating. Medicina. 2023; 59(1):113. https://doi.org/10.3390/medicina59010113
Chicago/Turabian StyleSouleiman, Firas, Jan Theopold, Ralf Henkelmann, Georg Osterhoff, Torsten Pastor, Boyko Gueorguiev, Johannes Fakler, and Pierre Hepp. 2023. "Combined Humeral Head and Shaft Fractures: Outcome Following Intramedullary Nailing and Plating" Medicina 59, no. 1: 113. https://doi.org/10.3390/medicina59010113






