Abstract
Background and Objectives: Osteoporosis results in increasing morbidity and mortality in hemodialysis patients. The medication for treatment has been limited. There is evidence that beta-blockers could increase bone mineral density (BMD) and reduce the risk of fracture in non-dialysis patients, however, a study in hemodialysis patients has not been conducted. This study aims to determine the association between beta-blocker use and bone mineral density level in hemodialysis patients. Materials and Methods: We conducted a cross-sectional study in hemodialysis patients at Thammasat University Hospital from January 2018 to December 2020. A patient receiving a beta-blocker ≥ 20 weeks was defined as a beta-blocker user. The association between beta-blocker use and BMD levels was determined by univariate and multivariate linear regression analysis. Results: Of the 128 patients receiving hemodialysis, 71 were beta-blocker users and 57 were non-beta-blocker users (control group). The incidence of osteoporosis in hemodialysis patients was 50%. There was no significant difference in the median BMD between the control and the beta-blocker groups of the lumbar spine (0.93 vs. 0.91, p = 0.88), femoral neck (0.59 vs. 0.57, p = 0.21), total hip (0.73 vs. 0.70, p = 0.38), and 1/3 radius (0.68 vs. 0.64, p = 0.40). The univariate and multivariate linear regression analyses showed that the beta-blocker used was not associated with BMD. In the subgroup analysis, the beta-1 selective blocker used was associated with lower BMD of the femoral neck but not within the total spine, total hip, and 1/3 radius. The multivariate logistic regression showed that the factors of age ≥ 65 years (aOR 3.31 (1.25–8.80), p = 0.02), female sex (aOR 4.13 (1.68–10.14), p = 0.002), lower BMI (aOR 0.89 (0.81–0.98), p = 0.02), and ALP > 120 U/L (aOR 3.88 (1.33–11.32), p = 0.01) were independently associated with osteoporosis in hemodialysis patients. Conclusions: In hemodialysis patients, beta-blocker use was not associated with BMD levels, however a beta-1 selective blocker used was associated with lower BMD in the femoral neck.
1. Introduction
Osteoporosis from chronic kidney disease-mineral and bone disease (CKD-MBD) can be defined as impaired bone health, causing a higher risk of bone fracture, and is associated with higher morbidity and mortality [1,2]. For bone strength evaluation, the Kidney Disease Improving Global Outcome (KDIGO) CKD-MBD guideline from 2017 recommends bone mineral density (BMD) testing in patients with CKD G3a–G5D with evidence of CKD-MBD and/or risk factors for osteoporosis to assess fracture risk if results impact treatment decisions [3]. However, the current medications that treat osteoporosis in hemodialysis patients (CKD G5D) are of limited availability. Drugs with possible benefits, including antiresorptive agents and anabolic hormones, are expensive and have side effects that require close monitoring during usage.
Beta-blockers are antihypertensive drugs that are widely used in hemodialysis patients. Besides the benefits of controlling blood pressure and cardiovascular disease, many studies have shown the benefits of beta-blockers in improving BMD and lowering the risk of bone fractures in the general population [4,5,6,7,8,9,10].
Studies in animal models have shown that bone formation is regulated by the leptin–sympathetic nervous system pathway. The elevation in leptin stimulates beta-adrenergic and sympathetic responses. The increase in sympathetic activity then induces osteoblasts to release the receptor activator of nuclear factor kappa-B ligand (RANKL), which signals the activation of osteoclasts and bone resorption. Beta-adrenergic receptor blocker plays the role of an antisympathetic agent which reduces intracerebral leptin [11,12,13] and directly binds to the beta-2 adrenergic receptor on the osteoblasts, resulting in the inhibition of RANKL and reduction in osteoclast activity [14,15]. These changes in bone remodeling may explain the overall effect of beta-blockers on the reduction in bone resorption and the increase in bone mass. However, there has been no study conducted in hemodialysis patients. Therefore, the aim of this study is to determine the association between beta-blocker use and BMD in patients receiving hemodialysis.
2. Materials and Methods
We conducted a single-center, cross-sectional study at Thammasat University Hospital in patients with adequate hemodialysis from 1 January 2018 to 31 October 2022.
We retrospectively reviewed all medical records using a standard case report form. Data were collected, including demographic characteristics, comorbidities, dialysis vintage, history of alcohol consumption and smoking, current medications, mean laboratory data within 1 year before performing BMD, and BMD data. The patients with ages of 18 or more who received adequate hemodialysis for at least 90 days were included. The beta-blocker users were patients who were currently using and had received a beta-blocker for at least 20 weeks. Patients who had incomplete medical records, post-parathyroidectomy, were receiving anti-osteoporotic treatment within 6 months, were receiving hormone replacement therapy, were taking calcimimetic drugs or immunosuppressive agents, and a history of malignancy or bone metastasis were excluded.
The primary objective was to assess the association between beta-blocker usage and BMD of the femoral neck, total hip, and 1/3 radius of hemodialysis patients. The secondary objectives were to determine the incidence of osteoporosis in hemodialysis patients and to examine the factors influencing osteoporosis in hemodialysis patients which were diagnosed by a T-score ≤ −2.5 of the total spine, femoral neck, total hip, or 1/3 radius.
Categorical variables were reported as a frequency and percentage, and numerical data were reported as a mean with a standard deviation (SD) or a median with an interquartile range (IQR) where appropriate. Comparison of the categorical and continuous data between the two groups was conducted by Fisher’s exact test and Wilcoxon’s rank sum test, respectively. Univariate and multivariate linear regression analyses were performed to determine the factors associated with BMD. Univariate and multivariate logistic regression was performed to determine the risk factors of osteoporosis. The covariates with p ≤ 0.1 from the univariate model were included in the multivariate model. A statistical significance was considered as p < 0.05. Data were analyzed using STATA version 16.
3. Results
From 1 January 2018 to 31 October 2022, 128 hemodialysis patients were included. A total of 57 patients were non-beta-blocker users (control group) and 71 patients were beta-blocker users. Of them, 53.1% of patients were female with a mean (SD) age of 65 (15) years and median (IQR) dialysis vintage of 32 (14–64.5) months. The baseline characteristics were not significantly different between the two groups (Table 1). Among the beta-blocker users, 23 of them used beta-1 selective blockers and 48 used non-selective beta-blockers. The baseline characteristics were not significantly different, except in serum bicarbonate levels, which were slightly higher in the non-selective beta-blocker users (25 (24.8–48.4) vs. 24 (23.3–24.7) mEq/L, p = 0.03) (Table S1).

Table 1.
Baseline characteristics of patients.
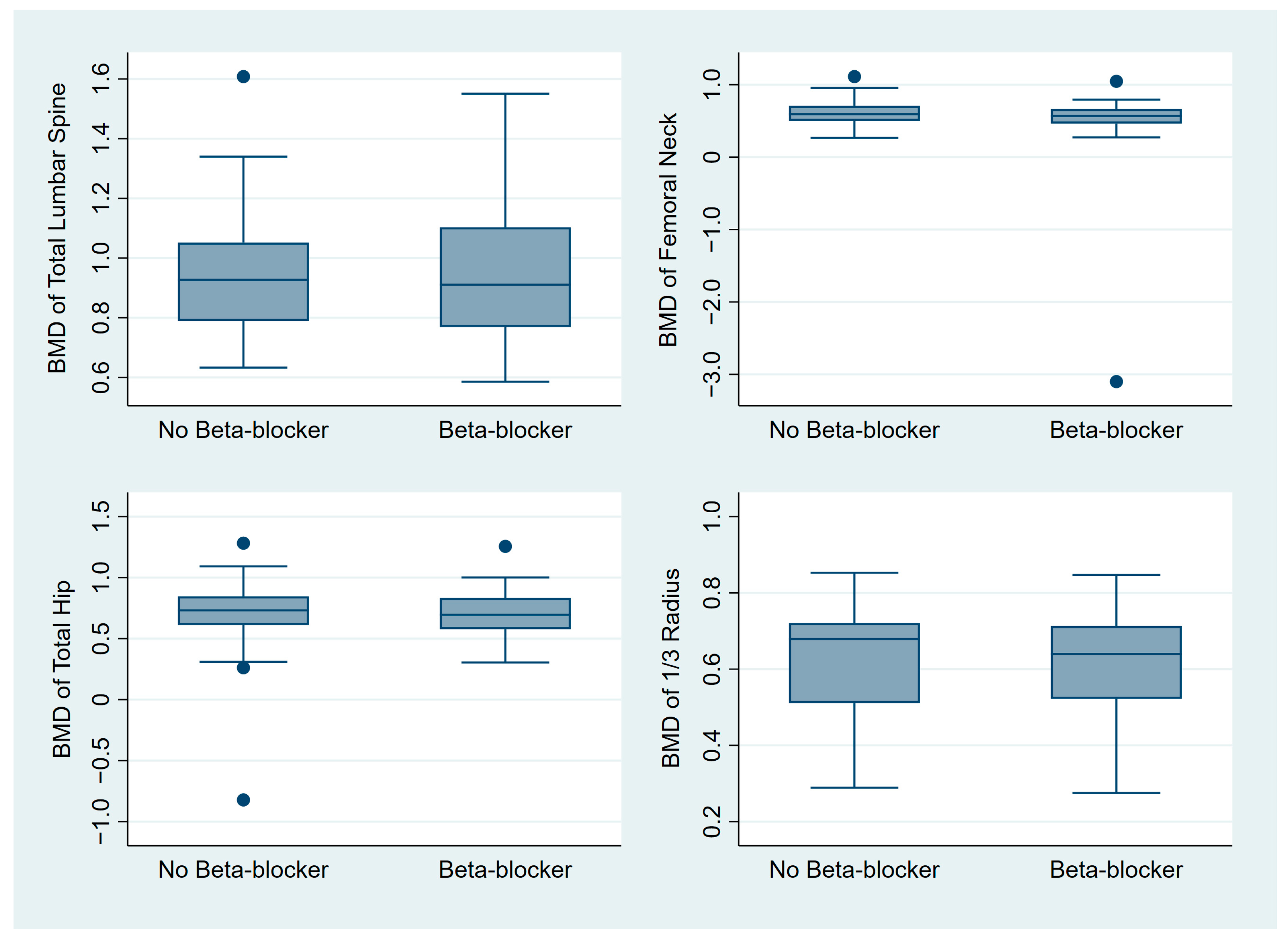
There was no difference in median BMD between the beta-blocker and control groups, including in total lumbar spine BMD (0.91 vs. 0.93, p = 0.88), femoral neck BMD (0.57 vs. 0.59, p = 0.21), total hip BMD (0.70 vs. 0.73, p = 0.38), and 1/3 radius BMD (0.68 vs. 0.64, p = 0.40), respectively (Figure 1, Table S2).
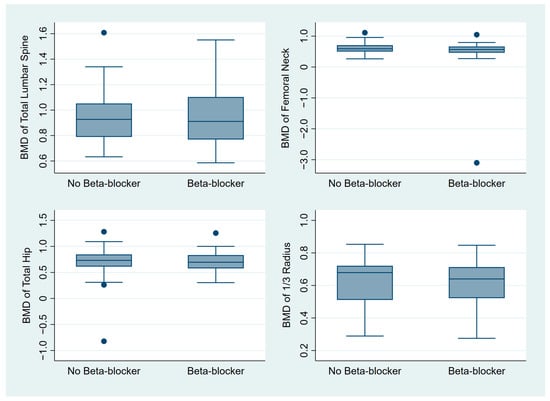
Figure 1.
Box plot graphs comparing the BMD between the beta-blocker and control groups. Abbreviation: BMD, bone mineral density.
From univariate linear regression analysis, the factors associated with BMD of the femoral neck were female, age ≥ 65 years, calcium < 8.5 mg/dL, and ALP > 120 U/L. Multivariate analysis showed that only the factors of age ≥ 65 years and female were associated with BMD of the femoral neck in Models 1 and 2. Beta-blocker use was not associated with BMD of the femoral neck in any models (Table 2). Beta-1 selective blocker use was significantly associated with BMD of the femoral neck in Model 1 (coefficient −0.17 (−0.33 to −0.005), p = 0.04), but not Model 2 (coefficient −0.16 (−0.33 to 0.003), p = 0.054) (Table S3).

Table 2.
Association of beta-blocker use and BMD of the femoral neck.
From univariate linear regression analysis, the factors associated with BMD of the total hip were female, age ≥ 65 years, lower BMI, and ALP > 120 U/L. Multivariate analysis showed that the factors of age ≥ 65 years, female, BMI, and ALP > 120 U/L were independently associated with BMD of the total hip in Models 1 and 2. Beta-blocker use was not associated with BMD of the total hip in any models (Table 3).

Table 3.
Association of beta-blocker use and BMD of the total hip.
From univariate linear regression analysis, the factors associated with BMD of the 1/3 radius were female, age ≥ 65 years, former smoking, dialysis vintage, PTH < 120 pg/mL, lower BMI, and ALP > 120 U/L. Multivariate analysis showed that the factors of age ≥ 65 years, female, and ALP > 120 U/L were independently associated with BMD of the 1/3 radius in Models 1 and 2. Beta-blocker use was not associated with BMD of the 1/3 radius in any models (Table 4).

Table 4.
Association of beta-blocker use and BMD of the 1/3 radius.
From univariate linear regression analysis, the factors associated with BMD of the total spine were female, BMI, ischemic stroke, gout, ACEi use, PTH > 585 pg/mL, and ALP > 120 U/L. Multivariate analysis showed that the factors of female, BMI, and gout were independently associated with BMD of the total spine in Models 1 and 2. Beta-blocker use was not associated with BMD of the total spine in any models (Table 5).

Table 5.
Association of beta-blocker use and BMD of the total spine.
The incidence of osteoporosis was 50% among all patients. When the on-site T-score ≤ −2.5 was investigated, the two most common sites were the femoral neck (35.94%) and 1/3 radius (35.16%) (Table S2). However, no difference in the incidence between the beta-blocker users and the control group was found.
From univariate logistic regression analysis, the risk factors of osteoporosis were female, age ≥ 65 years, lower BMI, and ALP > 120 U/L. Multivariate analysis showed that the factors of age ≥ 65 years (aOR 3.31 (1.25–8.80), p = 0.02), female (aOR 4.13 (1.68–10.14), p = 0.002), lower BMI (aOR 0.89 (0.81–0.98), p = 0.02), and ALP > 120 U/L (aOR 3.88 (1.33–11.32), p = 0.01) were independently associated with osteoporosis (Table 6).

Table 6.
Associated factors with osteoporosis.
4. Discussion
This is the first study to investigate the association between beta-blocker usage and BMD in hemodialysis patients. The study demonstrated that beta-blocker use was not associated with BMD levels, however in the subgroup analysis, beta-1 selective blocker use was associated with a lower BMD of the femoral neck. The prevalence of osteoporosis in hemodialysis patients was 50% and the risk factors for osteoporosis were age ≥ 65 years, female, lower BMI, and ALP over 120 U/L.
The association of beta-blocker use and BMD was found in non-hemodialysis patients, however the results remained inconsistent. Seven studies showed beta-blocker use was associated with higher BMD [4,5,6,7,8,9,10], but not in three other studies [16,17,18]. Compared to our study, our populations had a lower median femoral neck BMD than the population from previous positive studies (0.57 vs. 0.7–0.9) which might explain why the benefits of beta-blockers were not present in our study. Moreover, the most common mechanism of renal osteodystrophy in hemodialysis patients is not a high bone turnover but a low bone turnover process which has a prevalence of 56.1% [1]. In our study, only 16.41% of patients with a high level of both bone turnover markers (high PTH and ALP) possibly had a high turnover process. Only 2.34% of our patients had both low bone turnover markers (low PTH and ALP) and 82.46% had an undetermined process which needed a bone biopsy to prove. Since beta-blocker decreases bone remodeling via antisympathetic activity [11,12,13], the benefits of beta-blockers should be found only in the patients with high bone turnover process, but not in patients with a low bone turnover or undetermined bone turnover process (Figure S1). In our study, there was a high proportion of patients who possibly had a low bone turnover and undetermined bone turnover process; therefore, beta-blocker use did not associate with a higher BMD and even seemed to worsen it.
One meta-analysis [19] demonstrated that beta-1 selective blocker provides the benefit of reduced risk of fracture compared to non-selective beta-blocker which could be mediated systemically, unlike the direct effect on the beta-2 receptor of osteoclasts and osteoblasts. Nevertheless, our study demonstrated that selective beta-1 blocker was associated with lower BMD of the femoral neck. Since the BMD of the total spine might be falsely high from vascular calcification [20], which is the result of CKD-MBD, using BMD of the total spine to diagnose osteoporosis might be falsely negative. Thus, we focused on the BMD of the femoral neck, total hip, and 1/3 radius as the primary outcomes.
Compared with the study by Slouma et al. [21], the incidence of osteoporosis in hemodialysis patients in our study was higher, which might be explained by the higher mean age of our population (65 ± 15 vs. 53 ± 14). In contrast, our study found that the femoral neck and 1/3 radius were the most common sites of osteoporosis, while it was the total hip for the study by Slouma et al.
In concordance with our findings, we found the risk factors of osteoporosis were age ≥ 65 years, female, lower BMI, and ALP > 120 U/L. The study by Slouma et al. also found that age was a risk factor for osteoporosis; however this was not consistent with another study [1].
There were a few limitations in our study. First, the relatively small sample size of the population might result in a modest power of the study. Second, due to the nature of a cross-sectional study, the results could not indicate a causation. Third, the definite duration and dose of beta-blocker use were not available and they might affect the benefit of beta-blocker use on BMD.
5. Conclusions
There was no association between beta-blocker use and BMD levels in hemodialysis patients; however, the subgroup analysis showed beta-1 selective blocker was associated with a lower BMD of the femoral neck. The risk factors for osteoporosis in hemodialysis patients were age ≥ 65 years, sex, low BMD, and ALP over 120 U/L. Further studies to evaluate the effect of beta-blocker on BMD with a larger sample size and randomized controlled design in hemodialysis patients should be considered.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/medicina59010129/s1, Figure S1: Potential mechanism of beta-blocker use and bone remodeling in hemodialysis patients; Table S1: Baseline characteristics of beta-1 selective blockers versus non-selective beta-blocker users; Table S2: Comparison of BMD and incidence of osteoporosis between beta-blocker and control group; Table S3: Association of BMD with beta-blocker subtypes.
Author Contributions
Conceptualization, S.A. and P.P.; methodology, S.A. and P.P.; software, S.A. and P.P.; validation, P.T., P.P. and S.A.; formal analysis, S.A. and P.P.; investigation, S.T., S.A. and W.P.; resources, P.T. and S.T.; data curation, S.A. and P.P.; writing—original draft preparation, S.A., S.T. and P.P.; writing—review and editing, W.P. and P.T.; visualization, P.P.; supervision, S.A. and P.P.; project administration, S.A. and P.P.; funding acquisition, P.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Faculty of Medicine, Thammasat University.
Institutional Review Board Statement
This study was granted permission from the Human Research Ethics Committee of Thammasat University Hospital, Thailand (COA number 007/2021).
Informed Consent Statement
Patient consent was waived due to (1) The research protocol was less than minimal risk; (2) The research could not be carried out practicably without the waiver or alteration; and (3) The waiver or alteration had no impact the rights and well-being of research participants.
Data Availability Statement
Data are available from the corresponding author (P.P.) upon reasonable request.
Acknowledgments
This study was supported by the Research Group in Nephrology and Renal Replacement Therapy from the Faculty of Medicine, Thammasat University.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Barreto, F.D.C.; Barreto, D.V.; Moyses, R.M.A.; Neves, C.; Jorgetti, V.; Draibe, S.A.; Canziani, M.E.; Carvalho, A.B. Osteoporosis in hemodialysis patients revisited by bone histomorphometry: A new insight into an old problem. Kidney Int. 2006, 69, 1852–1857. [Google Scholar] [CrossRef]
- Iseri, K.; Dai, L.; Chen, Z.; Qureshi, A.R.; Brismar, T.B.; Stenvinkel, P.; Lindholm, B. Bone mineral density and mortality in end-stage renal disease patients. Clin. Kidney J. 2020, 13, 307–321. [Google Scholar] [CrossRef]
- Ketteler, M.; Block, G.A.; Evenepoel, P.; Fukagawa, M.; Herzog, C.A.; McCann, L.; Moe, S.M.; Shroff, R.; Tonelli, M.A.; Toussaint, N.D.; et al. Executive summary of the 2017 KDIGO Chronic Kidney Disease–Mineral and Bone Disorder (CKD-MBD) Guideline Update: What’s changed and why it matters. Kidney Int. 2017, 92, 26–36. [Google Scholar] [CrossRef]
- Reid, I.R.; Gamble, G.D.; Grey, A.B.; Black, D.M.; Ensrud, K.E.; Browner, W.S.; Bauer, D.C. β-Blocker Use, BMD, and Fractures in the Study of Osteoporotic Fractures. J. Bone Miner. Res. 2005, 20, 613–618. [Google Scholar] [CrossRef]
- Pasco, J.A.; Henry, M.J.; Sanders, K.M.; Kotowicz, M.A.; Seeman, E.; Nicholson, G.C. β-Adrenergic Blockers Reduce the Risk of Fracture Partly by Increasing Bone Mineral Density: Geelong Osteoporosis Study. J. Bone Miner. Res. 2004, 19, 19–24. [Google Scholar] [CrossRef]
- Turker, S.; Karatosun, V.; Gunal, I. [beta]-blockers Increase Bone Mineral Density. Clin. Orthop. Relat. Res. 2006, 443, 73–74. [Google Scholar] [CrossRef]
- Yang, S.; Nguyen, N.D.; Center, J.R.; Eisman, J.A.; Nguyen, T.V. Association between beta-blocker use and fracture risk: The Dubbo Osteoporosis Epidemiology Study. Bone 2011, 48, 451–455. [Google Scholar] [CrossRef]
- Lary, C.W.; Hinton, A.C.; Nevola, K.T.; Shireman, T.I.; Motyl, K.J.; Houseknecht, K.L.; Lucas, F.L.; Hallen, S.; Zullo, A.R.; Berry, S.D.; et al. Association of Beta Blocker Use With Bone Mineral Density in the Framingham Osteoporosis Study: A Cross-Sectional Study. JBMR Plus 2020, 4, e10388. [Google Scholar] [CrossRef]
- Swathi, P.; Shobharani, B. Role of beta blockers and associated fracture risk in indian subjects with primary osteoporosis. Eur. J. Mol. Clin. Med. 2022, 9, 177–185. [Google Scholar]
- Bonnet, N.; Gadois, C.; McCloskey, E.; Lemineur, G.; Lespessailles, E.; Courteix, D.; Benhamou, C.L. Protective effect of β blockers in postmenopausal women: Influence on fractures, bone density, micro and macroarchitecture. Bone 2007, 40, 1209–1216. [Google Scholar] [CrossRef]
- Takeda, S.; Elefteriou, F.; Levasseur, R.; Liu, X.; Zhao, L.; Parker, K.L.; Armstrong, D.; Ducy, P.; Karsenty, G. Leptin Regulates Bone Formation via the Sympathetic Nervous System. Cell 2002, 111, 305–317. [Google Scholar] [CrossRef]
- Cherruau, M.; Facchinetti, P.; Baroukh, B.; Saffar, J. Chemical sympathectomy impairs bone resorption in rats: A role for the sympathetic system on bone metabolism. Bone 1999, 25, 545–551. [Google Scholar] [CrossRef]
- Elefteriou, F.; Ahn, J.D.; Takeda, S.; Starbuck, M.; Yang, X.; Liu, X.; Kondo, H.; Richards, W.G.; Bannon, T.W.; Noda, M.; et al. Leptin regulation of bone resorption by the sympathetic nervous system and CART. Nature 2005, 434, 514–520. [Google Scholar] [CrossRef]
- Ducy, P.; Amling, M.; Takeda, S.; Priemel, M.; Schilling, A.F.; Beil, F.T.; Shen, J.; Vinson, C.; Rueger, J.M.; Karsenty, G. Leptin Inhibits Bone Formation through a Hypothalamic Relay: A Central Control of Bone Mass. Cell 2000, 100, 197–207. [Google Scholar] [CrossRef]
- Motyl, K.J.; Rosen, C.J. Understanding leptin-dependent regulation of skeletal homeostasis. Biochimie 2012, 94, 2089–2096. [Google Scholar] [CrossRef]
- Rejnmark, L.; Vestergaard, P.; Kassem, M.; Christoffersen, B.R.; Kolthoff, N.-U.; Brixen, K.; Mosekilde, L. Fracture Risk in Perimenopausal Women Treated with Beta-Blockers. Calcif. Tissue Int. 2004, 75, 365–372. [Google Scholar] [CrossRef]
- Solomon, D.H.; Diem, S.J.; Ruppert, K.; Lian, Y.J.; Liu, C.-C.; Wohlfart, A.; Greendale, G.A.; Finkelstein, J.S. Bone Mineral Density Changes Among Women Initiating Proton Pump Inhibitors or H2 Receptor Antagonists: A SWAN Cohort Study. J. Bone Miner. Res. 2015, 30, 232–239. [Google Scholar] [CrossRef]
- Hijazi, N.; Alourfi, Z. Association between Hypertension, Antihypertensive Drugs, and Osteoporosis in Postmenopausal Syrian Women: A Cross-Sectional Study. Adv. Med. 2020, 2020, 7014212. [Google Scholar] [CrossRef]
- Toulis, K.A.; Hemming, K.; Stergianos, S.; Nirantharakumar, K.; Bilezikian, J.P. β-adrenergic receptor antagonists and fracture risk: A meta-analysis of selectivity, gender, and site-specific effects. Osteoporos. Int. 2014, 25, 121–129. [Google Scholar] [CrossRef]
- Toussaint, N.D.; Lau, K.K.; Strauss, B.J.; Polkinghorne, K.R.; Kerr, P.G. Associations between vascular calcification, arterial stiffness and bone mineral density in chronic kidney disease. Nephrol. Dial. Transplant. 2008, 23, 586–593. [Google Scholar] [CrossRef]
- Slouma, M.; Sahli, H.; Bahlous, A.; Laadhar, L.; Smaoui, W.; Rekik, S.; Gharsallah, I.; Sallami, M.; Ben Moussa, F.; Elleuch, M.; et al. Mineral bone disorder and osteoporosis in hemodialysis patients. Hortic. Bras. 2020, 60, 15–17. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).