Prognostic Implication of Small Dense LDL-Cholesterol Levels following Acute Coronary Syndrome
Abstract
:1. Background
2. Methods
2.1. Patient Selection
2.2. Study Design
2.3. Coronary Revascularization
2.4. Biomarker Measurement
2.5. Other Clinical Data Obtained
2.6. Follow-Up Data
2.7. Statistical Analysis
3. Results
3.1. Baseline Characteristics on Admission
3.2. Clinical Data at the Index Discharge
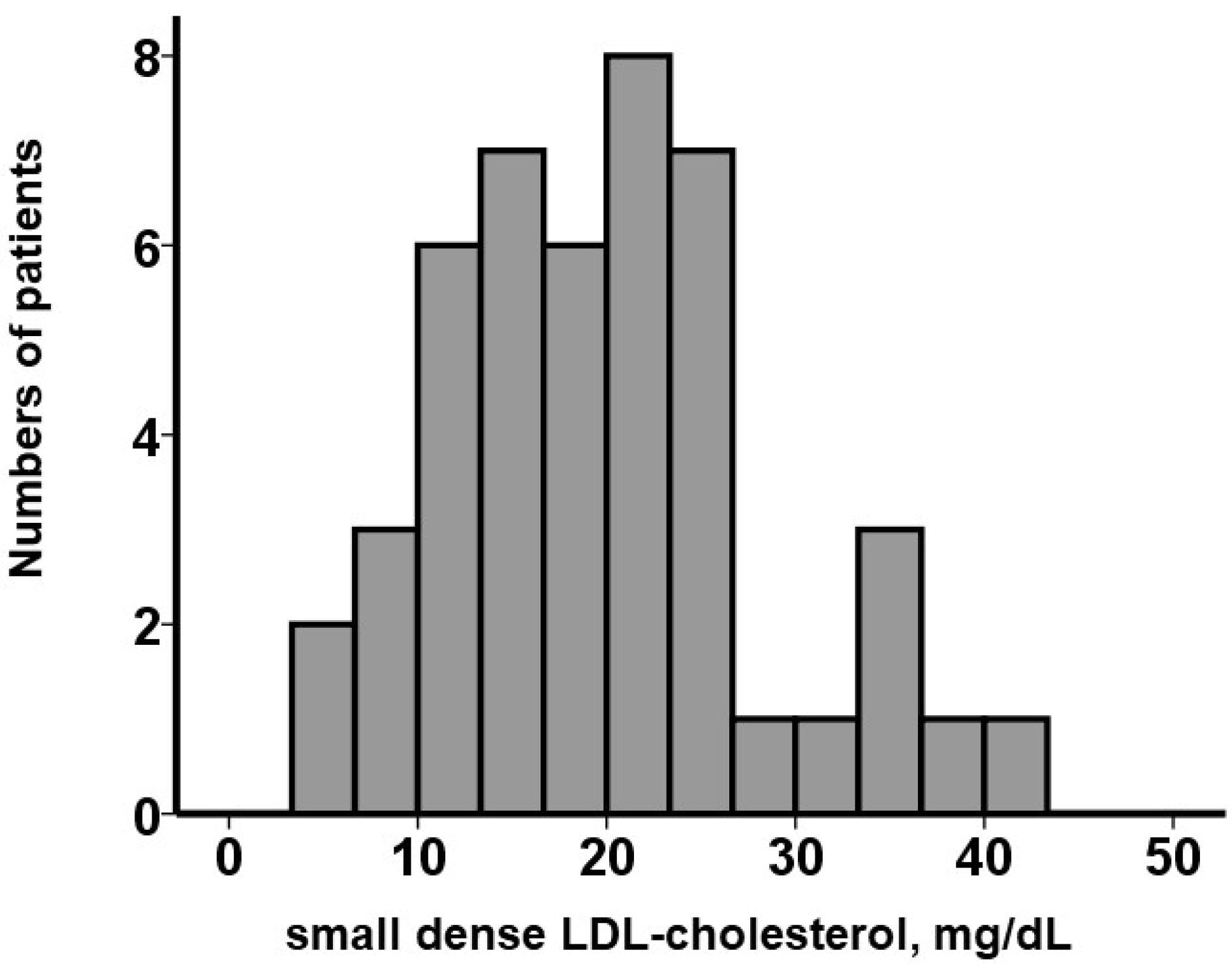
3.3. Prognostic Impact of Small Dense LDL-Cholesterol Levels at the Index Discharge
3.4. Clinical Data Follow-Up
4. Discussion
4.1. Impact of Small Dense LDL Cholesterol on the Occurrence of MACE
4.2. Future Directions
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ivanova, E.A.; Myasoedova, V.A.; Melnichenko, A.A.; Grechko, A.V.; Orekhov, A.N. Small Dense Low-Density Lipoprotein as Biomarker for Atherosclerotic Diseases. Oxid. Med. Cell. Longev. 2017, 2017, 1273042. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vekic, J.; Zeljkovic, A.; Cicero, A.F.G.; Janez, A.; Stoian, A.P.; Sonmez, A.; Rizzo, M. Atherosclerosis Development and Progression: The Role of Atherogenic Small, Dense LDL. Medicina 2022, 58, 299. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, T.; Koba, S.; Ito, Y.; Hirano, T. Method for estimating high sdLDL-C by measuring triglyceride and apolipoprotein B levels. Lipids Health Dis. 2017, 16, 21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hirano, T. Pathophysiology of Diabetic Dyslipidemia. J. Atheroscler. Thromb. 2018, 25, 771–782. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoogeveen, R.C.; Gaubatz, J.W.; Sun, W.; Dodge, R.C.; Crosby, J.R.; Jiang, J.; Couper, D.; Virani, S.S.; Kathiresan, S.; Boerwinkle, E.; et al. Small dense low-density lipoprotein-cholesterol concentrations predict risk for coronary heart disease: The Atherosclerosis Risk In Communities (ARIC) study. Arterioscler. Thromb. Vasc. Biol. 2014, 34, 1069–1077. [Google Scholar] [CrossRef] [Green Version]
- McPherson, R. Remnant cholesterol: “Non-(HDL-C + LDL-C)” as a coronary artery disease risk factor. J. Am. Coll. Cardiol. 2013, 61, 437–439. [Google Scholar] [CrossRef] [Green Version]
- St-Pierre, A.C.; Cantin, B.; Dagenais, G.R.; Mauriege, P.; Bernard, P.M.; Despres, J.P.; Lamarche, B. Low-density lipoprotein subfractions and the long-term risk of ischemic heart disease in men: 13-year follow-up data from the Quebec Cardiovascular Study. Arterioscler. Thromb. Vasc. Biol. 2005, 25, 553–559. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Higashioka, M.; Sakata, S.; Honda, T.; Hata, J.; Yoshida, D.; Hirakawa, Y.; Shibata, M.; Goto, K.; Kitazono, T.; Osawa, H.; et al. Small Dense Low-Density Lipoprotein Cholesterol and the Risk of Coronary Heart Disease in a Japanese Community. J. Atheroscler. Thromb. 2020, 27, 669–682. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qi, Y.; Liu, J.; Wang, W.; Wang, M.; Zhao, F.; Sun, J.; Liu, J.; Deng, Q.; Zhao, D. High sdLDL Cholesterol can be Used to Reclassify Individuals with Low Cardiovascular Risk for Early Intervention: Findings from the Chinese Multi-Provincial Cohort Study. J. Atheroscler. Thromb. 2020, 27, 695–710. [Google Scholar] [CrossRef] [Green Version]
- Williams, P.T.; Zhao, X.Q.; Marcovina, S.M.; Otvos, J.D.; Brown, B.G.; Krauss, R.M. Comparison of four methods of analysis of lipoprotein particle subfractions for their association with angiographic progression of coronary artery disease. Atherosclerosis 2014, 233, 713–720. [Google Scholar] [CrossRef]
- Jin, J.L.; Zhang, H.W.; Cao, Y.X.; Liu, H.H.; Hua, Q.; Li, Y.F.; Zhang, Y.; Wu, N.Q.; Zhu, C.G.; Xu, R.X.; et al. Association of small dense low-density lipoprotein with cardiovascular outcome in patients with coronary artery disease and diabetes: A prospective, observational cohort study. Cardiovasc. Diabetol. 2020, 19, 45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sakai, K.; Koba, S.; Nakamura, Y.; Yokota, Y.; Tsunoda, F.; Shoji, M.; Itoh, Y.; Hamazaki, Y.; Kobayashi, Y. Small dense low-density lipoprotein cholesterol is a promising biomarker for secondary prevention in older men with stable coronary artery disease. Geriatr. Gerontol. Int. 2018, 18, 965–972. [Google Scholar] [CrossRef] [Green Version]
- Sekimoto, T.; Koba, S.; Mori, H.; Sakai, R.; Arai, T.; Yokota, Y.; Sato, S.; Tanaka, H.; Masaki, R.; Oishi, Y.; et al. Small Dense Low-Density Lipoprotein Cholesterol: A Residual Risk for Rapid Progression of Non-Culprit Coronary Lesion in Patients with Acute Coronary Syndrome. J. Atheroscler. Thromb. 2021, 28, 1161–1174. [Google Scholar] [CrossRef]
- Zhang, J.; He, L. Relationship between small dense low density lipoprotein and cardiovascular events in patients with acute coronary syndrome undergoing percutaneous coronary intervention. BMC Cardiovasc. Disord. 2021, 21, 169. [Google Scholar] [CrossRef]
- Arai, H.; Kokubo, Y.; Watanabe, M.; Sawamura, T.; Ito, Y.; Minagawa, A.; Okamura, T.; Miyamato, Y. Small dense low-density lipoproteins cholesterol can predict incident cardiovascular disease in an urban Japanese cohort: The Suita study. J. Atheroscler. Thromb. 2013, 20, 195–203. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santos, H.O.; Earnest, C.P.; Tinsley, G.M.; Izidoro, L.F.M.; Macedo, R.C.O. Small dense low-density lipoprotein-cholesterol (sdLDL-C): Analysis, effects on cardiovascular endpoints and dietary strategies. Prog. Cardiovasc. Dis. 2020, 63, 503–509. [Google Scholar] [CrossRef] [PubMed]
- Maruyama, C.; Imamura, K.; Teramoto, T. Assessment of LDL particle size by triglyceride/HDL-cholesterol ratio in non-diabetic, healthy subjects without prominent hyperlipidemia. J. Atheroscler. Thromb. 2003, 10, 186–191. [Google Scholar] [CrossRef] [Green Version]
- Ikezaki, H.; Lim, E.; Cupples, L.A.; Liu, C.T.; Asztalos, B.F.; Schaefer, E.J. Small Dense Low-Density Lipoprotein Cholesterol Is the Most Atherogenic Lipoprotein Parameter in the Prospective Framingham Offspring Study. J. Am. Heart Assoc. 2021, 10, e019140. [Google Scholar] [CrossRef]
- Ikezaki, H.; Furusyo, N.; Yokota, Y.; Ai, M.; Asztalos, B.F.; Murata, M.; Hayashi, J.; Schaefer, E.J. Small Dense Low-Density Lipoprotein Cholesterol and Carotid Intimal Medial Thickness Progression. J. Atheroscler. Thromb. 2020, 27, 1108–1122. [Google Scholar] [CrossRef] [Green Version]
- Yamashita, S.; Masuda, D.; Matsuzawa, Y. Pemafibrate, a New Selective PPARalpha Modulator: Drug Concept and Its Clinical Applications for Dyslipidemia and Metabolic Diseases. Curr. Atheroscler. Rep. 2020, 22, 5. [Google Scholar] [CrossRef]
- Pradhan, A.D.; Paynter, N.P.; Everett, B.M.; Glynn, R.J.; Amarenco, P.; Elam, M.; Ginsberg, H.; Hiatt, W.R.; Ishibashi, S.; Koenig, W.; et al. Rationale and design of the Pemafibrate to Reduce Cardiovascular Outcomes by Reducing Triglycerides in Patients with Diabetes (PROMINENT) study. Am. Heart J. 2018, 206, 80–93. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.; Parhofer, K.G. Diabetic dyslipidemia. Metabolism 2014, 63, 1469–1479. [Google Scholar] [CrossRef] [PubMed]



| N = 46 | |
|---|---|
| Demographics | |
| Age, years | 75 (59, 83) |
| Men | 29 (63%) |
| Body mass index | 23.0 (21.1, 25.7) |
| Comorbidity | |
| Diabetes mellitus | 19 (41%) |
| Atrial fibrillation | 5 (11%) |
| History of stroke | 7 (15%) |
| History of heart failure | 4 (9%) |
| Echocardiography | |
| Left ventricular end-diastolic diameter, mm | 45 (40, 49) |
| Left ventricular ejection fraction, % | 53 (33, 60) |
| Moderate or greater mitral regurgitation | 1 (2%) |
| Moderate or greater tricuspid regurgitation | 4 (9%) |
| Laboratory data | |
| Estimated glomerular filtration ratio, mL/min/1.73m2 | 60.9 (34.5, 76.0) |
| Plasma B-type natriuretic peptide, pg/mL | 108 (41, 561) |
| HDL-cholesterol, mg/dL | 47 (41, 59) |
| LDL-cholesterol, mg/dL | 93 (76, 124) |
| Triglyceride, mg/dL | 82 (56, 133) |
| Medication | |
| Loop diuretics | 4 (9%) |
| Beta-blockers | 9 (20%) |
| Renin-angiotensin system inhibitors | 19 (41%) |
| Mineralocorticoid receptor antagonists | 3 (7%) |
| SGLT2 inhibitors | 4 (9%) |
| Statin | 14 (30%) |
| Fibrate | 1 (2%) |
| Ezetimibe | 0 (0%) |
| N = 46 | |
|---|---|
| Type of disease | |
| Acute myocardial infarction | 28 (61%) |
| Recent myocardial infarction | 4 (9%) |
| Unstable angina pectoris | 14 (30%) |
| Target vessel | |
| Left main trunk | 6 (13%) |
| Left anterior descending artery | 23 (50%) |
| Right coronary artery | 11 (24%) |
| Left circumflex artery | 6 (13%) |
| Procedure | |
| Percutaneous coronary intervention | 42 (91%) |
| Coronary artery bypass grafting | 4 (9%) |
| Maximum creatinine kinase, U/L | 2151 (533, 7091) |
| Days of hospitalization, days | 16 (10, 32) |
| N = 46 | |
|---|---|
| Laboratory data | |
| Estimated glomerular filtration ratio, mL/min/1.73m2 | 61.3 (52.4, 74.0) |
| Plasma B-type natriuretic peptide, pg/mL | 140 (73, 290) |
| HDL-cholesterol, mg/dL | 42 (35, 48) |
| LDL-cholesterol, mg/dL | 77 (64, 109) |
| Triglyceride, mg/dL | 109 (74, 140) |
| Triglyceride to HDL-cholesterol ratio | 2.41 (1.32, 3.48) |
| Medication | |
| Loop diuretics | 11 (24%) |
| Beta-blockers | 36 (78%) |
| Renin-angiotensin system inhibitors | 37 (80%) |
| Mineralocorticoid receptor antagonists | 12 (26%) |
| SGLT2 inhibitors | 12 (26%) |
| Statin | 46 (100%) |
| Fibrate | 1 (2%) |
| Ezetimibe | 10 (22%) |
| Hazard Ratio | 95% Confidence Interval | p Value | |
|---|---|---|---|
| Univariable | |||
| Small dense LDL cholesterol | 1.114 | 1.026–1.209 | 0.010 * |
| Multivariable | |||
| Small dense LDL cholesterol + age | 1.125 | 1.029–1.231 | 0.010 * |
| Small dense LDL cholesterol + men | 1.112 | 1.024–1.208 | 0.012 * |
| Small dense LDL cholesterol + max creatinine kinase | 1.114 | 1.026–1.209 | 0.010 * |
| Small dense LDL cholesterol + BNP | 1.174 | 1.054–1.308 | 0004 * |
| Small dense LDL cholesterol + LDL cholesterol | 1.114 | 1.016–1.222 | 0.021 * |
| Small Dense LDL >32.6 (N = 5) | Small Dense LDL ≤32.6 (N = 41) | p Value | |
|---|---|---|---|
| At index discharge | |||
| Estimated glomerular filtration ratio, mL/min/1.73 m2 | 58.9 (41.8, 65.1) | 61.7 (52.4, 76.5) | 0.49 |
| Plasma B-type natriuretic peptide, pg/mL | 101 (77, 154) | 160 (60, 327) | 0.66 |
| HDL-cholesterol, mg/dL | 35 (30, 40) | 43 (36, 50) | 0.042 * |
| LDL-cholesterol, mg/dL | 79 (61, 106) | 75 (61, 96) | 0.15 |
| Remnant cholesterol, mg/dL | 35 (9, 40) | 21 (15, 27) | 0.43 |
| Triglyceride, mg/dL | 185 (126, 230) | 107 (69, 140) | 0.21 |
| Triglyceride to HDL-cholesterol ratio | 4.52 (2.28, 5.00) | 2.40 (1.32, 3.20) | 0.16 |
| Three months follow-up | |||
| Estimated glomerular filtration ratio, mL/min/1.73 m2 | 56.7 (40.1, 63.4) | 61.2 (52.1, 75.6) | 0.41 |
| Plasma B-type natriuretic peptide, pg/mL | 142 (98, 243) | 121 (43, 223) | 0.45 |
| HDL-cholesterol, mg/dL | 33 (28, 38) | 45 (37, 52) | 0.037 * |
| LDL-cholesterol, mg/dL | 77 (60, 102) | 76 (60, 97) | 0.43 |
| Remnant cholesterol, mg/dL | 37 (11, 42) | 20 (14, 26) | 0.18 |
| Triglyceride, mg/dL | 192 (131, 245) | 103 (66, 137) | 0.13 |
| Triglyceride to HDL-cholesterol ratio | 4.77 (2.34, 5.14) | 2.34 (1.21, 3.14) | 0.084 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Imamura, T.; Hori, M.; Narang, N.; Ueno, H.; Kinugawa, K. Prognostic Implication of Small Dense LDL-Cholesterol Levels following Acute Coronary Syndrome. Medicina 2023, 59, 158. https://doi.org/10.3390/medicina59010158
Imamura T, Hori M, Narang N, Ueno H, Kinugawa K. Prognostic Implication of Small Dense LDL-Cholesterol Levels following Acute Coronary Syndrome. Medicina. 2023; 59(1):158. https://doi.org/10.3390/medicina59010158
Chicago/Turabian StyleImamura, Teruhiko, Masakazu Hori, Nikhil Narang, Hiroshi Ueno, and Koichiro Kinugawa. 2023. "Prognostic Implication of Small Dense LDL-Cholesterol Levels following Acute Coronary Syndrome" Medicina 59, no. 1: 158. https://doi.org/10.3390/medicina59010158
APA StyleImamura, T., Hori, M., Narang, N., Ueno, H., & Kinugawa, K. (2023). Prognostic Implication of Small Dense LDL-Cholesterol Levels following Acute Coronary Syndrome. Medicina, 59(1), 158. https://doi.org/10.3390/medicina59010158







