1. Introduction
For those with flail chest and stable hemodynamic status, pain is a major factor that exerts an adverse effect on respiratory function and quality of life [
1]. Current treatment plans focus on surgical fixation and non-operative treatment. Surgical fixation tends to be more beneficial because it results in a shorter duration of mechanical ventilation use, shorter intensive care unit stay, and lower risks of acute respiratory distress syndrome and pneumonia [
2]. Some studies reported surgery is associated with decreased hospital charges [
3,
4]. In Taiwan, the national health insurance (NHI) system covers most basic healthcare fees [
5]. Surgical rib fixation is reimbursed but the plates and screws are out-of-pocket expense until mid-2021 [
6]. For patients, higher healthcare expenses were incurred to the patients in the surgical fixation group [
7]. For those who are not suitable or unwilling for surgery, nonoperative treatment might be considered as an alternative, which has a major disadvantage of prolonged pain. Although regional block such as epidural anesthesia, an intercostal nerve block, an intrathecal opioid, intrapleural analgesia, and a paravertebral block tends to be more effective than systemic pain control, it needs skin puncture [
8,
9,
10].
A recent study has shown that rib splints have been designed to simultaneously reduce pain and increase lung capacity [
11]. We aimed to find an easy, fast, and effective solution for the majority of patients with flail chest for whom surgery is unsuitable. The solution is named the “Kaohsiung Medical University Rib Orthotic Device” (K-Rod), which is easily constructed using common materials. It incorporates a three-dimensional (3D) computed tomography (CT)-based assessment, a tailored design, and a portable application. The K-Rod is described in detail in the following.
2. Technique
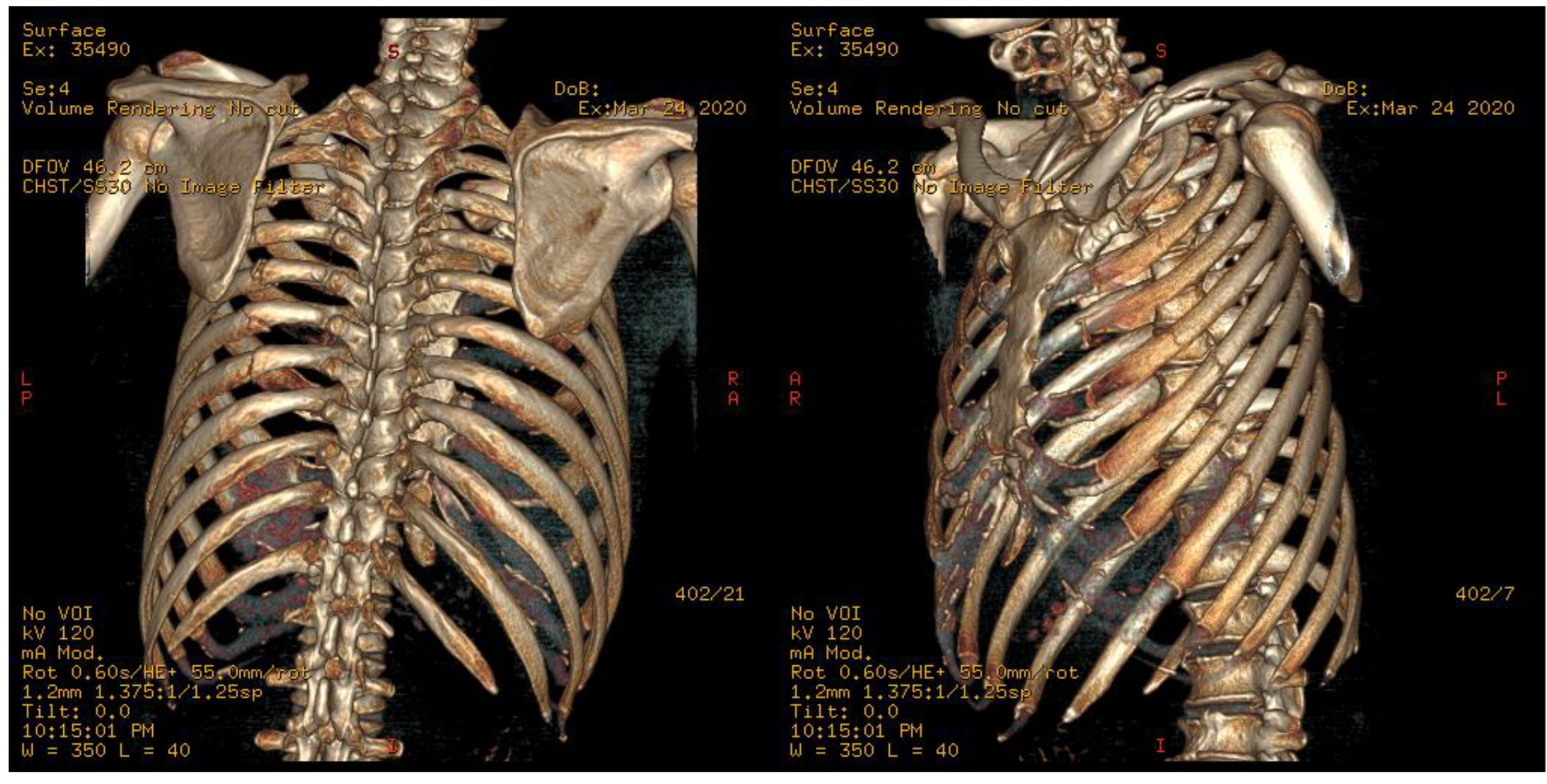
A 42-year-old man presented with severe chest pain after being involved in a fall. On arrival, he had clear consciousness, stable blood pressure, and slight tachypnea. Chest CT scan revealed overt left second to eighth rib fractures, and the fourth to eighth ribs were broken in two places, as flail chest is defined. Because of severe pain (visual analog scale (VAS) score: 9 points), he complained of shortness of breath, and supplemental oxygen was provided with a measured SpO2 of 90%. Oral and intravenous analgesics were applied, but his chest pain was intractably controlled during the first 24 h. Operation of rib fixation was proposed after evaluation by a thoracic surgeon, but he turned down the proposal because the out-of-pocket expense of surgery was unaffordable. We decided to apply the K-Rod. A reformatted 3D scan of the chest CT scan was acquired to evaluate fracture sites in all involved ribs (
Figure 1).
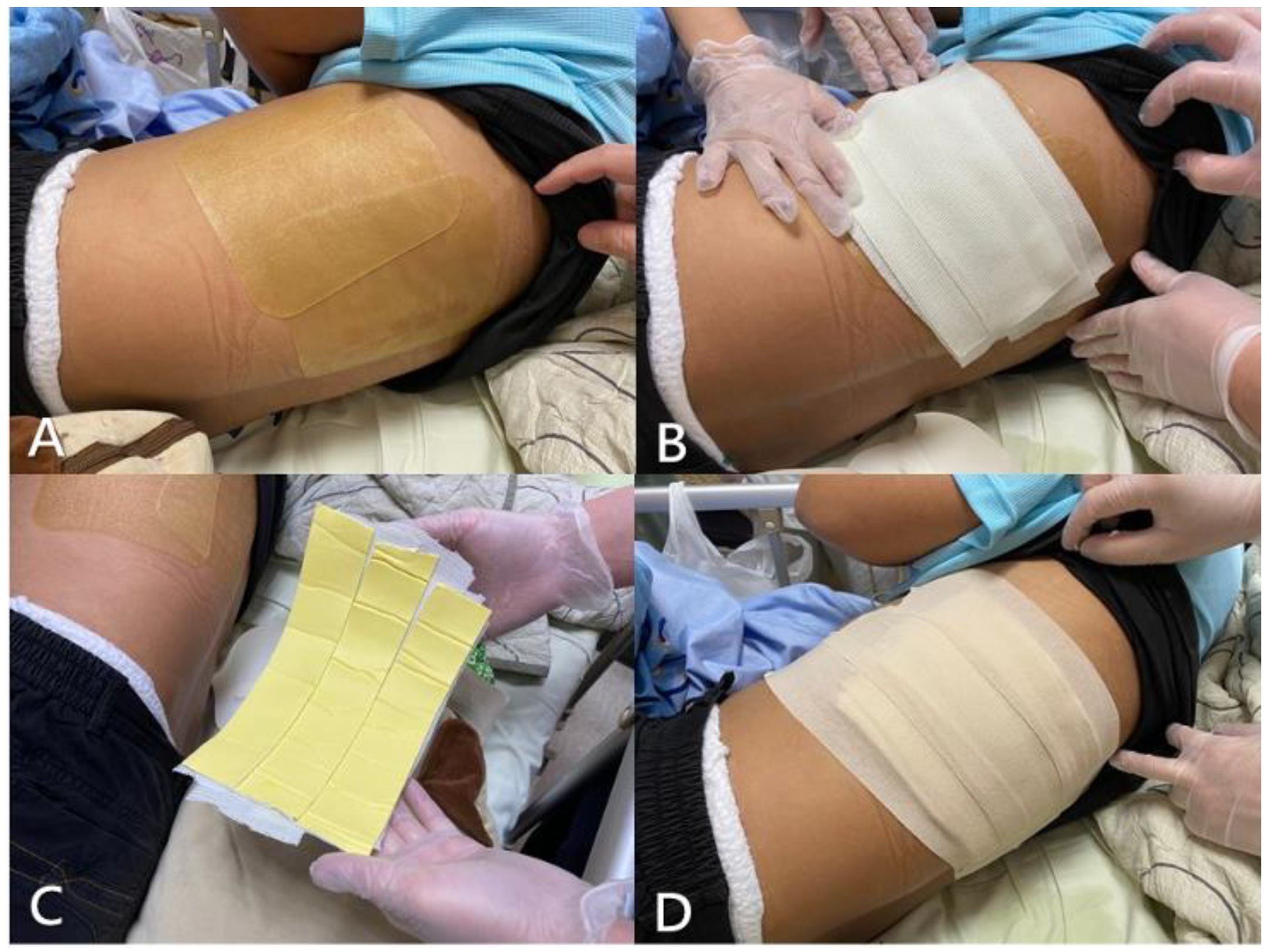
As the locations of fracture sites were crucial to the effectiveness of rib splinting, we inspected and palpated his torso in detail and then marked tender points on the basis of 3D images of his chest. Subsequently, a handmade K-Rod was placed that covered all fracture sites and adjacent stable ribs. The K-Rod comprised four layers (
Figure 2).
The first (innermost) layer was adhesive hydrocolloid dressing, which protected the skin and acted as an interface, providing stability between the splint and skin. The second layer was a double-sided foam tape applied to bridge the hydrocolloid dressing and hard part of the splint. The third layer, made of six-layered fiberglass casting tape (3M Scotchcast, 4 inches wide), was the only hard part of the K-Rod. The casting tape was trimmed and tailored for the complete coverage of injury sites. It was immersed in room-temperature water and then immediately adhered to the chest wall tightly before it hardened. Finally, the fiberglass layer of the splint was securely fixed over injury sites by using elastic adhesive tape, which formed the fourth (outermost) layer (
Figure 3).
Using this K-Rod for external fixation of fractured ribs, an expeditious and excellent result was achieved. The patient’s pain–inspiration–cough (PIC) score before and after splinting was 3 and 7. His pain was greatly alleviated, as indicated by a postprocedural VAS of 4 points, and he could ambulate on his own immediately. The next day, he stopped using supplemental oxygen and had an improved pain score (VAS: 1 point). We provided only oral acetaminophen three times daily as supplemental pain control. His PIC score improved to 9 points in the following 48 h, and he was uneventfully discharged after a 6-day stay.
From March to December 2020, we applied K-rod to 43 patients, pain score (VAS) significantly decreased after the application of the K-Rod from a median of 8/10 to 2/10 (
Table 1). Incentive spirometry was also used for these patients as a tool for lung function evaluations and risk of pulmonary complication prediction for those with fractured ribs [
12]. In our study, patients achieved a higher volume of incentive spirometry immediately after the K-Rod was applied (from 510 mL to 750 mL).
3. Discussion
In recent years, operative management of flail chest has gained popularity and proved with benefits [
2,
7,
13,
14,
15,
16]. Surgical rib fixation provides significant pain reduction, but it is actually performed for only a limited proportion of patients. For the majority of patients treated nonoperatively, optimal pain control is paramount [
17]. Our innovative method can be easily applied in nonoperative patients with flail chest and offers excellent pain control.
Rib splints have been proposed previously for relieving pain and increasing vital capacity, particularly in prehospital settings and when analgesia is inadequate. However, splinting ribs can be challenging because of their diverse location and complex severity. Furthermore, a circumferential bandage exerting compressive force over the chest restricts thoracic movement and prevents adequate ventilation. A previous study has shown the effectiveness of fixation through chest orthosis or rib splints [
11]. Uncustomizability, in addition to cost and accessibility, is the major weakness of this approach.
The K-Rod demonstrated several strengths. First, postprocedural pain relief is promptly achieved. Second, our rib splint is personalizable and scalable. By evaluating 3D CT scans, the fracture location and pattern were clearly recognized. Furthermore, by localizing tender points through palpation, we were confident regarding the size and shape of the rib splint required prior to splinting. Different from the previous use of circumferential rib belts, our tailored splint was employed to merely fix the injury site, having limited effect on lung expansion. Furthermore, because of the superior structural stability of the flail site compared with that achieved in other approaches, our patient had higher incentive spirometry performance after rib splinting. Lastly, our method has several other advantages including portable intervention, quick application, and lower cost compared with surgical fixation. The only challenge we had encountered before was inadequate fixation because fractured ribs were just under a woman’s large breast or scapula.
4. Conclusions
In summary, the K-Rod can be applied in an acute care setting and has numerous clinical and economic merits. Our method would have a vital positive effect on the current practice of flail chest management under limited resources.
Author Contributions
Conceptualization, C.-W.C.; methodology, C.-W.C.; software, C.-W.C. and C.-J.L.; validation, Y.-S.Y. and Y.-K.L.; formal analysis, C.-W.C. and C.-J.L.; investigation, Y.-S.Y. and Y.-K.L.; writing—original draft preparation, C.-W.C. and C.-J.L.; writing—review and editing, Y.-S.Y. and Y.-K.L.; visualization, C.-J.L.; supervision, Y.-S.Y., Y.-K.L. and C.-W.C. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by the Kaohsiung Medical University Hospital (KMUH105-5R25) and National Science and Technology Council of Taiwan (MOST 110-2314-B-037-044).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Kaohsiung Medical University (Date: 22 October 2021, number: KMUHIRB-E(II)-20210236).
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Farley, P.; Griffin, R.L.; Jansen, J.O.; Bosarge, P.L. Quantifying Pain Associated With Rib Fractures. J. Surg. Res. 2020, 246, 476–481. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Liu, P.; Chen, J.; Xie, J.; Yang, F.; Liao, Y. A Randomized Controlled Trial of Surgical Rib Fixation in Polytrauma Patients with Flail Chest. J. Surg. Res. 2019, 242, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Coleman, J.R.M.; Leasia, K.; Douglas, I.S.; Hosokawa, P.M.; Lawless, R.A.; Moore, E.E.; Pieracci, F.M. Quantifying the expense of deferring surgical stabilization of rib fractures: Operative management of rib fractures is associated with significantly lower charges. J. Trauma Acute Care Surg. 2020, 89, 1032–1038. [Google Scholar] [CrossRef] [PubMed]
- Bhatnagar, A.; Mayberry, J.; Nirula, R. Rib Fracture Fixation for Flail Chest: What Is the Benefit? J. Am. Coll. Surg. 2012, 215, 201–205. [Google Scholar] [CrossRef] [PubMed]
- Fang, K.; Shia, B.-C.; Ma, S. Health insurance coverage, medical expenditure and coping strategy: Evidence from Taiwan. BMC Health Serv. Res. 2012, 12, 442. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ku, Y.-C.; Chou, Y.-J.; Lee, M.-C.; Pu, C. Effects of National Health Insurance on household out-of-pocket expenditure structure. Soc. Sci. Med. 2019, 222, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Xiong, K. Surgical management versus non-surgical management of rib fractures in chest trauma: A systematic review and meta-analysis. J. Cardiothorac. Surg. 2019, 14, 45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ho, A.M.-H.; Ho, A.K.; Mizubuti, G.B.; Klar, G.; Karmakar, M.K. Regional analgesia for patients with traumatic rib fractures: A narrative review. J. Trauma Acute Care Surg. 2020, 88, e22–e30. [Google Scholar] [CrossRef] [PubMed]
- Rauchwerger, J.J.; Candido, K.D.; Deer, T.R.; Frogel, J.K.; Iadevaio, R.; Kirschen, N.B. Thoracic Epidural Steroid Injection for Rib Fracture Pain. Pain Pract. 2013, 13, 416–421. [Google Scholar] [CrossRef] [PubMed]
- De Almeida, C.R. Parascapular Sub-Iliocostalis Plane Block: Comparative Description of a Novel Technique for Posterior Rib Fractures. Pain Pract. 2021, 21, 708–714. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Lee, S.-H.; Kim, C.; Choi, H.J. Comparison of the effectiveness in pain reduction and pulmonary function between a rib splint constructed in the ER and a manufactured rib splint. Medicine 2018, 97, e10779. [Google Scholar] [CrossRef] [PubMed]
- Sadler, C.A.; Burgess, J.R.; Dougherty, K.E.; Collins, J.N. Bedside Incentive Spirometry Predicts Risk of Pulmonary Complication in Patients with Rib Fractures. Am. Surg. 2019, 85, 1051–1055. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, H.; Yukioka, T.; Yamaguti, Y.; Shimizu, S.; Goto, H.; Matsuda, H.; Shimazaki, S. Surgical Stabilization of Internal Pneumatic Stabilization? A Prospective Randomized Study of Management of Severe Flail Chest Patients. J. Trauma 2002, 52, 727–732. [Google Scholar] [CrossRef] [PubMed]
- Marasco, S.F.; Davies, A.R.; Cooper, J.; Varma, D.; Bennett, V.; Nevill, R.; Lee, G.; Bailey, M.; Fitzgerald, M. Prospective Randomized Controlled Trial of Operative Rib Fixation in Traumatic Flail Chest. J. Am. Coll. Surg. 2013, 216, 924–932. [Google Scholar] [CrossRef] [PubMed]
- Granetzny, A.; Abd El-Aal, M.; Emam, E.; Shalaby, A.; Boseila, A. Surgical versus conservative treatment of flail chest. Evaluation of the pulmonary status. Interact. Cardiovasc. Thorac. Surg. 2005, 4, 583–587. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pieracci, F.M.; Lin, Y.; Rodil, M.; Synder, M.; Herbert, B.; Tran, D.K.; Stoval, R.T.; Johnson, J.L.; Biffl, W.L.; Barnett, C.C.; et al. A prospective, controlled clinical evaluation of surgical stabilization of severe rib fractures. J. Trauma Acute Care Surg. 2016, 80, 187–194. [Google Scholar] [CrossRef] [PubMed]
- Davignon, K.; Kwo, J.; Bigatello, L.M. Pathophysiology and management of the flail chest. Minerva Anestesiol. 2004, 70, 193–199. [Google Scholar] [PubMed]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).