Change in Maxillary Sinus Mucosal Thickness in Patients with Preoperative Maxillary Sinus Mucosal Thickening as Assessed by Otolaryngologists: A Retrospective Study
Abstract
:1. Introduction
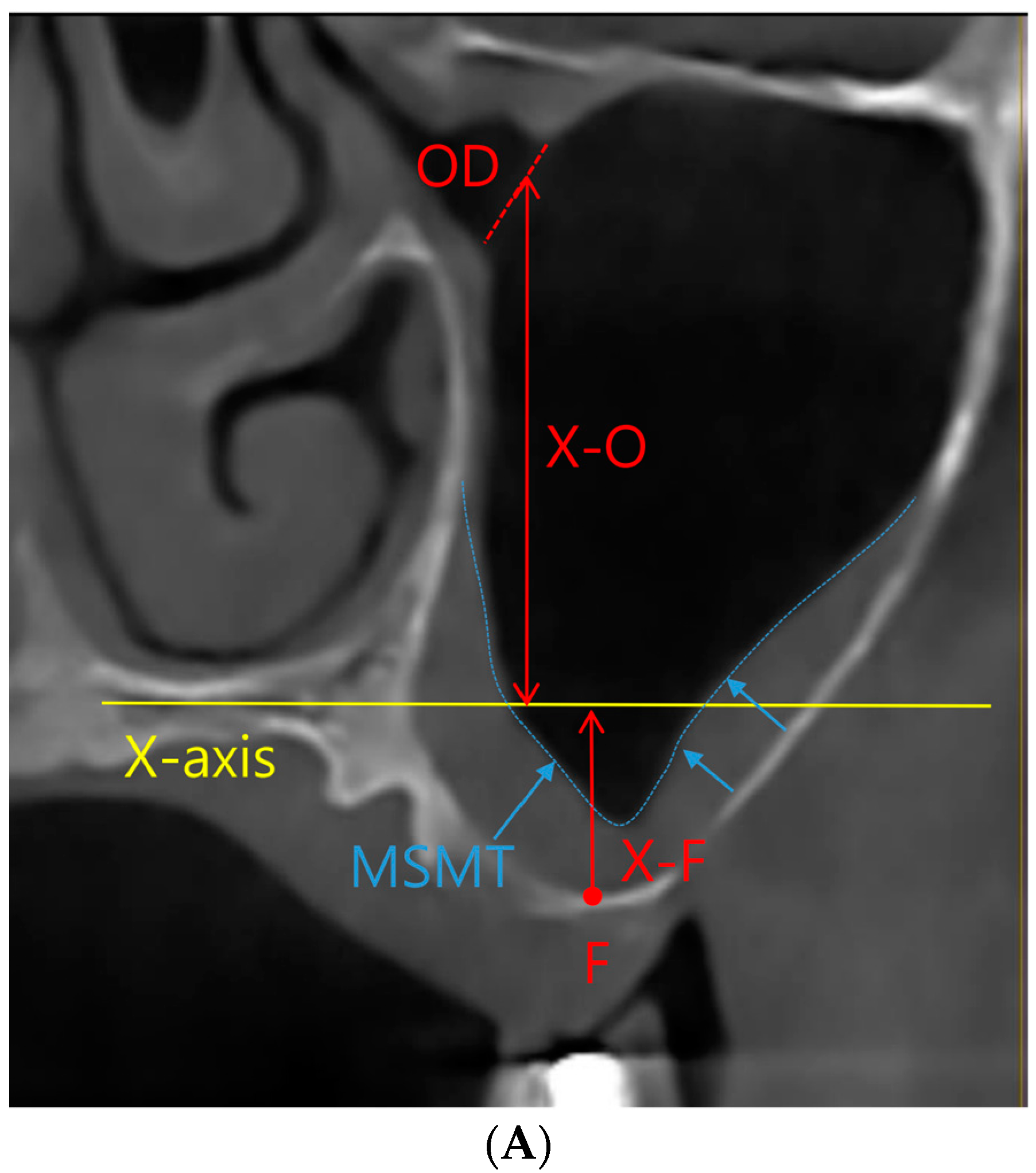
2. Materials and Methods
2.1. Study Design
2.2. Statistic Evaluation
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kayabasi, O. Design methodology for dental implant using approximate solution techniques. J. Stomatol. Oral Maxillofac. Surg. 2020, 121, 684–695. [Google Scholar] [CrossRef] [PubMed]
- Ahn, W.B.; Lee, Y.B.; Ji, Y.H.; Moon, K.S.; Jang, H.S.; Kang, S.W. Decellularized Human Adipose Tissue as an Alternative Graft Material for Bone Regeneration. Tissue Eng. Regen. Med. 2022, 19, 1089–1098. [Google Scholar] [CrossRef] [PubMed]
- Yeung, A.W.K.; Hung, K.F.; Li, D.T.S.; Leung, Y.Y. The Use of CBCT in Evaluating the Health and Pathology of the Maxillary Sinus. Diagnostics 2022, 12, 2819. [Google Scholar] [CrossRef]
- Ding, X.; Zhu, J.; Liu, A.; Guo, Q.; Cao, Q.; Xu, Y.; Hua, Y.; Yang, Y.; Li, P. Preparation and Biocompatibility Study of Contrast-Enhanced Hernia Mesh Material. Tissue Eng. Regen. Med. 2022, 19, 703–715. [Google Scholar] [CrossRef]
- Salari, A.; Seyed Monir, S.E.; Ostovarrad, F.; Samadnia, A.H.; Naser Alavi, F. The frequency of maxillary sinus pathologic findings in cone-beam computed tomography images of patients candidate for dental implant treatment. J. Adv. Periodontol. Implant Dent. 2021, 13, 2–6. [Google Scholar] [CrossRef]
- Ata-Ali, J.; Diago-Vilalta, J.V.; Melo, M.; Bagán, L.; Soldini, M.C.; Di-Nardo, C.; Ata-Ali, F.; Mañes-Ferrer, J.F. What is the frequency of anatomical variations and pathological findings in maxillary sinuses among patients subjected to maxillofacial cone beam computed tomography? A systematic review. Med. Oral Patol. Oral Y Cir. Bucal 2017, 22, e400–e409. [Google Scholar] [CrossRef]
- Di Girolamo, S.; Martino, F.; Guerrieri, M.; Turco, M.; Flora, B.; Fuccillo, E.; Di Girolamo, M. Odontogenic Maxillary Sinusopathies: A Radiological Classification. J. Maxillofac. Oral Surg. 2022, 21, 141–149. [Google Scholar] [CrossRef]
- Amid, R.; Kadkhodazadeh, M.; Moscowchi, A.; Nami, M. Effect of Schneiderian Membrane Thickening on the Maxillary Sinus Augmentation and Implantation Outcomes: A Systematic Review. J. Maxillofac. Oral Surg. 2021, 20, 534–544. [Google Scholar] [CrossRef]
- Manji, A.; Faucher, J.; Resnik, R.R.; Suzuki, J.B. Prevalence of maxillary sinus pathology in patients considered for sinus augmentation procedures for dental implants. Implant Dent. 2013, 22, 428–435. [Google Scholar] [CrossRef]
- Lee, W. Corticotomy for orthodontic tooth movement. J. Korean Assoc. Oral Maxillofac. Surg. 2018, 44, 251–258. [Google Scholar] [CrossRef]
- Hammuda, A.A.; Ghoneim, M.M. Assessment of maxillary sinus lifting procedure in the presence of chronic sinusitis, a retrospective comparative study. Ann. Med. Surg. 2021, 66, 102379. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.W.; Yang, B.E.; Cheon, K.J.; Jang, W.S.; Kim, J.W.; Byun, S.H. A Simple and Safe Approach for Maxillary Sinus Augmentation with the Advanced Surgical Guide. Int. J. Environ. Res. Public Health 2020, 17, 3785. [Google Scholar] [CrossRef] [PubMed]
- Lumbau, A.I.; Meloni, S.M.; Tallarico, M.; Melis, L.; Spano, G.; Baldoni, E.; Koshovari, A.; Pisano, M. Implant Placement Following Crestal Sinus Lift with Sequential Drills and Osteotomes: Five Years after Final Loading Results from a Retrospective Study. J. Funct. Biomater. 2021, 12, 10. [Google Scholar] [CrossRef] [PubMed]
- Cheon, K.J.; Yang, B.E.; Cho, S.W.; Chung, S.M.; Byun, S.H. Lateral Window Design for Maxillary Sinus Graft Based on the Implant Position. Int. J. Environ. Res. Public Health 2020, 17, 6335. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.; Vinitha, B.; Fathima, G. Bone grafts in dentistry. J. Pharm. Bioallied Sci. 2013, 5, S125–S127. [Google Scholar] [CrossRef]
- Borges, F.L.; Dias, R.O.; Piattelli, A.; Onuma, T.; Gouveia Cardoso, L.A.; Salomão, M.; Scarano, A.; Ayub, E.; Shibli, J.A. Simultaneous sinus membrane elevation and dental implant placement without bone graft: A 6-month follow-up study. J. Periodontol. 2011, 82, 403–412. [Google Scholar] [CrossRef]
- Kim, J.; Jang, H. A review of complications of maxillary sinus augmentation and available treatment methods. J. Korean Assoc. Oral Maxillofac. Surg. 2019, 45, 220–224. [Google Scholar] [CrossRef]
- Grawish, M.E.; Grawish, L.M.; Grawish, H.M.; Grawish, M.M.; Holiel, A.A.; Sultan, N.; El-Negoly, S.A. Demineralized Dentin Matrix for Dental and Alveolar Bone Tissues Regeneration: An Innovative Scope Review. Tissue Eng. Regen. Med. 2022, 19, 687–701. [Google Scholar] [CrossRef]
- Akbari, S.; Taheri, M.; Aslroosta, H.; Ordoukhani, A.; Paknejad, M.; Hashemi, F.; Farimani, Z. Relationship of Maxillary Sinus Mucosal Thickening and Residual Alveolar Ridge Height: A CBCT Analysis. Front. Dent. 2022, 19, 19. [Google Scholar] [CrossRef]
- Küçükkurt, S. Evaluation of the survival of implant placement simultaneously with sinus augmentation: Relationship in maxillary sinus pathologies. Oral Radiol. 2020, 36, 225–237. [Google Scholar] [CrossRef]
- Shpachynskyi, O.; Didkovskij, V.; Kopchak, A. Radiological changes in maxillary sinus morphology after lateral sinus floor augmentation. Otolaryngol. Pol.=Pol. Otolaryngol. 2020, 74, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Mayer, Y.; Ben-Dor, A.; Zigdon-Giladi, H.; Gutmacher, Z. Dimensional changes in the sinus membrane following maxillary sinus augmentation. Quintessence Int. 2018, 49, 841–847. [Google Scholar] [CrossRef]
- Bilge, N.H.; Dagistanli, S.; Karasu, Y.; Orhan, K. Comparison of Pathologic Changes in the Maxillary Sinus Before and After Dental Implant Surgery Using Cone Beam Computed Tomography. Int. J. Oral Maxillofac. Implant. 2023, 1–8. [Google Scholar] [CrossRef]
- Rey-Martínez, M.H.; Ruiz-Sáenz, P.L.; Martínez-Rodríguez, N.; Barona-Dorado, C.; Meniz-García, C.; Cortés-Bretón Brinkmann, J.; Suárez-Quintanilla, J.A.; Martínez-González, J.M. Analysis of the Radiological Changes of the Sinus Membrane Using Cone Beam Computed Tomography and Its Relationship with Dental Treatments. A Retrospective Study. Biology 2022, 11, 165. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; He, Z.; Tian, H. Association between periodontal status and degree of maxillary sinus mucosal thickening: A retrospective CBCT study. BMC Oral Health 2021, 21, 392. [Google Scholar] [CrossRef] [PubMed]
- Park, W.B.; Kim, J.; Kim, Y.J.; Kang, P.; Lim, H.C.; Han, J.Y. Changes in sinus mucosal thickening in the course of tooth extraction and lateral sinus augmentation with surgical drainage: A cone-beam computed tomographic study. Clin. Oral Implant. Res. 2023, 34, 95–104. [Google Scholar] [CrossRef]
- Kayabasoglu, G.; Nacar, A.; Altundag, A.; Cayonu, M.; Muhtarogullari, M.; Cingi, C. A retrospective analysis of the relationship between rhinosinusitis and sinus lift dental implantation. Head Face Med. 2014, 10, 53. [Google Scholar] [CrossRef]
- Wei, Y.; Zhang, B.; Yang, G.; Xu, T.; Hu, W.; Chung, K.H. Effect of ridge preservation at molar extraction sites with severe periodontitis on the Schneiderian membrane thickness changes: A pilot study. BMC Oral Health 2021, 21, 184. [Google Scholar] [CrossRef]
- Alrayyes, Y.; Al-Jasser, R. Regenerative Potential of Platelet Rich Fibrin (PRF) in Socket Preservation in Comparison with Conventional Treatment Modalities: A Systematic Review and Meta-Analysis. Tissue Eng. Regen. Med. 2022, 19, 463–475. [Google Scholar] [CrossRef]
- Zirk, M.; Dreiseidler, T.; Pohl, M.; Rothamel, D.; Buller, J.; Peters, F.; Zöller, J.E.; Kreppel, M. Odontogenic sinusitis maxillaris: A retrospective study of 121 cases with surgical intervention. J. Cranio-Maxillo-Facial Surg. Off. Publ. Eur. Assoc. Cranio-Maxillo-Facial Surg. 2017, 45, 520–525. [Google Scholar] [CrossRef]
- Çelik, O.E.; Ceylan, M.E. Sinus Augmentation Using Caldwell-Luc Technique in the Existence of Ectopic Tooth in the Maxillary Sinus: A Multidisciplinary Approach. J. Craniofacial Surg. 2022, 33, e758–e761. [Google Scholar] [CrossRef] [PubMed]
- Janner, S.F.M.; Dubach, P.; Suter, V.G.A.; Caversaccio, M.D.; Buser, D.; Bornstein, M.M. Sinus floor elevation or referral for further diagnosis and therapy: A comparison of maxillary sinus assessment by ENT specialists and dentists using cone beam computed tomography. Clin. Oral Implant. Res. 2020, 31, 463–475. [Google Scholar] [CrossRef] [PubMed]
- Ritter, A.; Rozendorn, N.; Avishai, G.; Rosenfeld, E.; Koren, I.; Soudry, E. Preoperative Maxillary Sinus Imaging and the Outcome of Sinus Floor Augmentation and Dental Implants in Asymptomatic Patients. Ann. Otol. Rhinol. Laryngol. 2020, 129, 209–215. [Google Scholar] [CrossRef]
- Bornstein, M.M.; Yeung, A.W.K.; Tanaka, R.; von Arx, T.; Jacobs, R.; Khong, P.L. Evaluation of Health or Pathology of Bilateral Maxillary Sinuses in Patients Referred for Cone Beam Computed Tomography Using a Low-Dose Protocol. Int. J. Periodontics Restor. Dent. 2018, 38, 699–710. [Google Scholar] [CrossRef]
- Chen, Y.W.; Lee, F.Y.; Chang, P.H.; Huang, C.C.; Fu, C.H.; Huang, C.C.; Lee, T.J. A paradigm for evaluation and management of the maxillary sinus before dental implantation. Laryngoscope 2018, 128, 1261–1267. [Google Scholar] [CrossRef]
- Park, W.B.; Kim, Y.J.; Park, J.S.; Han, J.Y.; Lim, H.C. Complication and Salvage of Sinus Floor Elevation in the Maxillary Sinus With Asymptomatic and Noncalcified Fungus Colonization: A Case Report. J. Oral Implantol. 2021, 47, 242–248. [Google Scholar] [CrossRef]
- Zimbler, M.S.; Lebowitz, R.A.; Glickman, R.; Brecht, L.E.; Jacobs, J.B. Antral augmentation, osseointegration, and sinusitis: The otolaryngologist’s perspective. Am. J. Rhinol. 1998, 12, 311–316. [Google Scholar] [CrossRef]
- Chiesa-Estomba, C.M.; Aiastui, A.; González-Fernández, I.; Hernáez-Moya, R.; Rodiño, C.; Delgado, A.; Garces, J.P.; Paredes-Puente, J.; Aldazabal, J.; Altuna, X.; et al. Three-Dimensional Bioprinting Scaffolding for Nasal Cartilage Defects: A Systematic Review. Tissue Eng. Regen. Med. 2021, 18, 343–353. [Google Scholar] [CrossRef]
- Park, W.B.; Kim, Y.J.; Han, J.Y.; Park, J.S.; Kang, P. Radiographic and Nasal Endoscopic Observation of Accidentally Perforated Anterior Nasal Cavity with Dental Implants: Case Reports with 5-23 Years of Follow-Up. J. Oral Implantol. 2021, 47, 492–497. [Google Scholar] [CrossRef]
- Costa, F.; Emanuelli, E.; Robiony, M. Incidence of Maxillary Sinus Disease Before Sinus Floor Elevation Surgery as Identified by Cone-Beam Computed Tomography: A Literature Review. J. Oral Implantol. 2018, 44, 161–166. [Google Scholar] [CrossRef]
- Hellings, P.W.; Fokkens, W.J.; Orlandi, R.; Adriaensen, G.F.; Alobid, I.; Baroody, F.M.; Bjermer, L.; Senior, B.A.; Cervin, A.; Cohen, N.A.; et al. The EUFOREA pocket guide for chronic rhinosinusitis. Rhinology 2023, 61, 85–89. [Google Scholar] [CrossRef] [PubMed]
- Cohen, R.; Haas, H.; Lorrot, M.; Biscardi, S.; Romain, O.; Vie Le Sage, F.; Hentgen, V.; Grimprel, E. Antimicrobial treatment of ENT infections. Arch. Pediatr. Organe Off. Soc. Fr. Pediatr. 2017, 24, S9–S16. [Google Scholar] [CrossRef]
- Choi, Y.S.; Ham, D.S.; Lim, J.Y.; Lee, Y.K. Validation of the Osteomyelitis Induced by Methicillin-Resistant Staphylococcus aureus (MRSA) on Rat Model with Calvaria Defect. Tissue Eng. Regen. Med. 2021, 18, 671–683. [Google Scholar] [CrossRef]
- Becker, D.G. The minimally invasive, endoscopic approach to sinus surgery. J. Long-Term Eff. Med. Implant. 2003, 13, 207–221. [Google Scholar] [CrossRef] [PubMed]
- Miyazaki, H.; Takahashi, Y.; Kuruma, T.; Someda, S.K.; Kakizaki, H. Treatment Strategies for Orbital Gas-producing Necrotizing Fasciitis Secondary to Odontogenic Maxillary Sinusitis: Technical Notes. J. Stomatol. Oral Maxillofac. Surg. 2023, 101544. [Google Scholar] [CrossRef] [PubMed]
- Tobita, T.; Nakamura, M.; Ueno, T.; Sano, K. Sinus augmentation surgery after endoscopic sinus surgery for the treatment of chronic maxillary sinusitis: A case report. Implant Dent. 2011, 20, 337–340. [Google Scholar] [CrossRef] [PubMed]
- Procacci, P.; Zangani, A.; Rossetto, A.; Rizzini, A.; Zanette, G.; Albanese, M. Odontogenic orbital abscess: A case report and review of literature. Oral Maxillofac. Surg. 2017, 21, 271–279. [Google Scholar] [CrossRef]
- Chen, Y.W.; Huang, C.C.; Chang, P.H.; Chen, C.W.; Wu, C.C.; Fu, C.H.; Lee, T.J. The characteristics and new treatment paradigm of dental implant-related chronic rhinosinusitis. Am. J. Rhinol. Allergy 2013, 27, 237–244. [Google Scholar] [CrossRef]
- Faber, J.; Fonseca, L.M. How sample size influences research outcomes. Dent. Press J. Orthod. 2014, 19, 27–29. [Google Scholar] [CrossRef]
- Bathla, S.C.; Fry, R.R.; Majumdar, K. Maxillary sinus augmentation. J. Indian Soc. Periodontol. 2018, 22, 468–473. [Google Scholar] [CrossRef]
- Shenvi, E.C.; Meeker, D.; Boxwala, A.A. Understanding data requirements of retrospective studies. Int. J. Med. Inform. 2015, 84, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Gatti, F.; Gatti, C.; Tallarico, M.; Tommasato, G.; Meloni, S.M.; Chiapasco, M. Maxillary Sinus Membrane Elevation Using a Special Drilling System and Hydraulic Pressure: A 2-Year Prospective Cohort Study. Int. J. Periodontics Restor. Dent. 2018, 38, 593–599. [Google Scholar] [CrossRef] [PubMed]






Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.-H.; Min, E.J.; Ko, Y.; Kim, D.H.; Park, J.-B. Change in Maxillary Sinus Mucosal Thickness in Patients with Preoperative Maxillary Sinus Mucosal Thickening as Assessed by Otolaryngologists: A Retrospective Study. Medicina 2023, 59, 1750. https://doi.org/10.3390/medicina59101750
Kim J-H, Min EJ, Ko Y, Kim DH, Park J-B. Change in Maxillary Sinus Mucosal Thickness in Patients with Preoperative Maxillary Sinus Mucosal Thickening as Assessed by Otolaryngologists: A Retrospective Study. Medicina. 2023; 59(10):1750. https://doi.org/10.3390/medicina59101750
Chicago/Turabian StyleKim, Jin-Hyeong, Eun Jeong Min, Youngkyung Ko, Do Hyun Kim, and Jun-Beom Park. 2023. "Change in Maxillary Sinus Mucosal Thickness in Patients with Preoperative Maxillary Sinus Mucosal Thickening as Assessed by Otolaryngologists: A Retrospective Study" Medicina 59, no. 10: 1750. https://doi.org/10.3390/medicina59101750
APA StyleKim, J.-H., Min, E. J., Ko, Y., Kim, D. H., & Park, J.-B. (2023). Change in Maxillary Sinus Mucosal Thickness in Patients with Preoperative Maxillary Sinus Mucosal Thickening as Assessed by Otolaryngologists: A Retrospective Study. Medicina, 59(10), 1750. https://doi.org/10.3390/medicina59101750






