Successful Endoscopic Transsphenoidal Approach Treatment of Sphenoid Sinus Organized Hematoma Causing Visual Deficit: A Case Report
Abstract
:1. Introduction
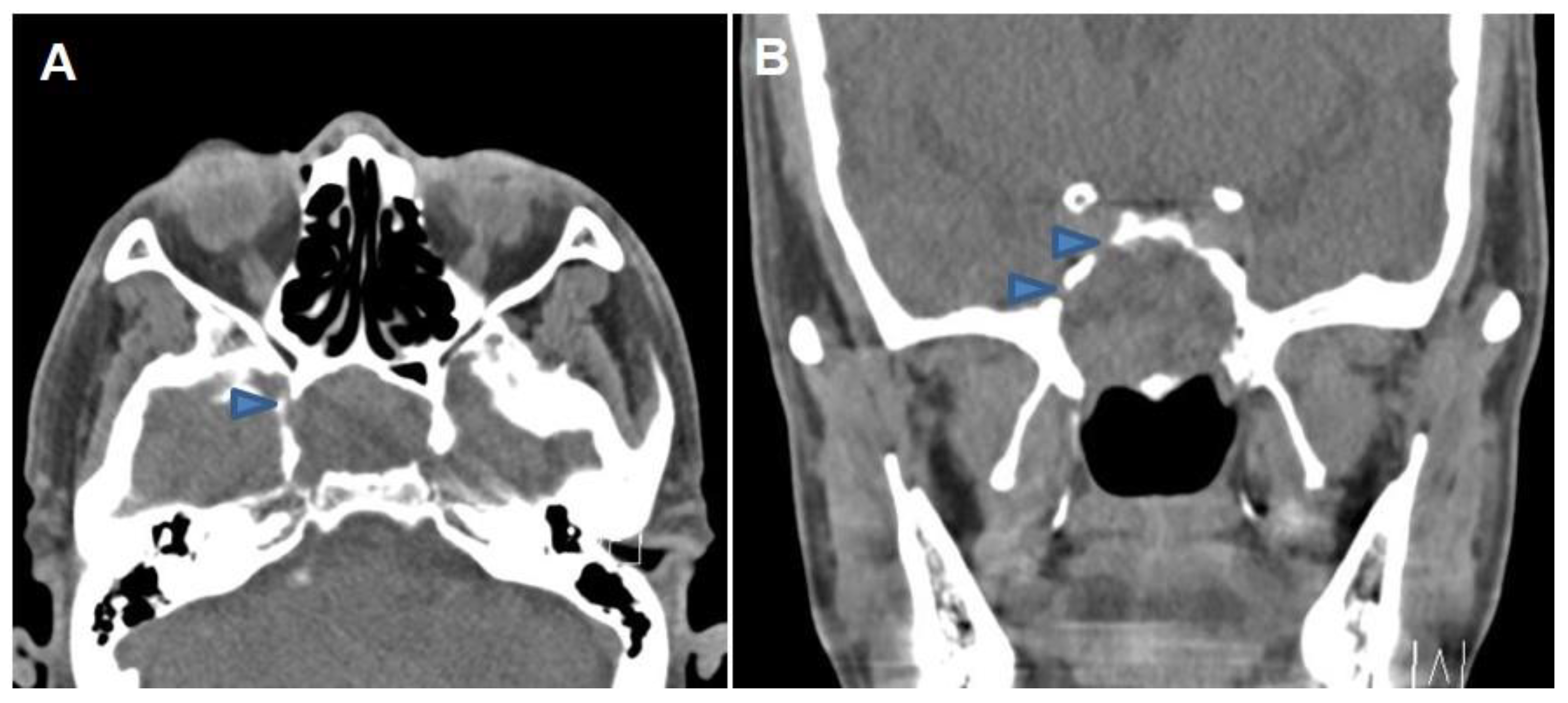
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lin, G.C.; Wells Porrmann, J.; Paz, M.; Moshel, Y.A.; LeBenger, J.; Benitez, R.P. Organized hematoma of the sphenoid sinus with acute blindness: Insight into pathogenesis of disease. Ear Nose Throat J. 2020, 99, 605–609. [Google Scholar] [CrossRef]
- Lin, Y.H.; Wang, P.C.; Lin, Y.S. Sphenoid sinus organized hematoma with cranial neuropathies masquerading as a malignancy: A case report. Oncol. Lett. 2016, 11, 3571–3574. [Google Scholar] [CrossRef] [PubMed]
- Yoon, Y.H.; Kim, S.H.; Kim, Y.M.; Rha, K.S. Organized hematoma of the sphenoid sinus causing acute visual loss. Eur. J. Ophthalmol. 2018, 28, NP7–NP9. [Google Scholar] [CrossRef] [PubMed]
- Nakagawa, T.; Kawai, Y.; Sakamoto, T.; Ito, J. Organised haematoma of the sphenoid sinus mimicking a pituitary tumour. J. Laryngol. Otol. 2010, 124, 83–85. [Google Scholar] [CrossRef]
- Wu, A.W.; Ting, J.Y.; Borgie, R.C.; Busaba, N.Y.; Sadow, P.M.; Juliano, A.F.; Gray, S.T.; Holbrook, E.H. Diagnostic characteristics of sinonasal organizing hematomas: Avoiding misdiagnosis. Int. Forum Allergy Rhinol. 2013, 3, 598–602. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.J.; Seo, S.T.; Rha, K.-S.; Kim, Y.M. Sinonasal organized hematoma: Clinical features of seventeen cases and a systematic review. Laryngoscope 2015, 125, 2027–2033. [Google Scholar] [CrossRef]
- Min, H.J.; Kim, K.S. Sinonasal organized hematoma mimicking nasal polyposis. Ear Nose Throat J. 2021, 100, NP381–NP383. [Google Scholar] [CrossRef]
- Tanida, M.; Hayama, M.; Maeda, Y.; Obata, S.; Nakatani, A.; Amano, Y.; Inohara, H. Organized hematoma after intra-arterial chemoradiotherapy for maxillary sinus cancer: A case report. Ear Nose Throat J. 2022, 7, 1455613221091099. [Google Scholar] [CrossRef]
- Nishiguchi, T.; Nakamura, A.; Mochizuki, K.; Tokuhara, Y.; Yamane, H.; Inoue, Y. Expansile organized maxillary sinus hematoma: MR and CT findings and review of literature. AJNR Am. J. Neuroradiol. 2007, 28, 1375–1377. [Google Scholar] [CrossRef]
- Kim, J.S.; Oh, J.S.; Kwon, S.H. The increasing incidence of paranasal organizing hematoma: A 20-year experience of 23 cases at a single center. Rhinology 2016, 54, 176–182. [Google Scholar] [CrossRef]
- Ashwini, R.; Narayana, G.K.; Shetty, R.; Gopal, N.K. Sinonasal Organised Haematoma- A Case Report and Review of Literature. Indian J. Otolaryngol. Head Neck Surg. 2023, 75, 1009–1013. [Google Scholar]
- Varghese, L.; Mukhopadhyay, S.; Mehan, R.; Kurien, R.; Thomas, M.; Rupa, V. Sinonasal organising haematoma—A little known entity. Braz. J. Otorhinolaryngol. 2019, 85, 698–704. [Google Scholar] [CrossRef] [PubMed]
- Ohta, N.; Watanabe, T.; Ito, T.; Kubota, T.; Suzuki, Y.; Ishida, A.; Aoyagi, M.; Matsubara, A.; Izuhara, K.; Kakehata, S. Clinical and pathological characteristics of organized hematoma. Int. J. Otolaryngol. 2013, 2013, 539642. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.K.; Kim, K.S. Organizing hematoma of the maxillary sinus mimicking malignancy diagnosed by Fluorodeoxyglucose Positron-Emission Tomography (FDG PET/CT): A case feport. Iran. J. Radiol. 2015, 12, e18924. [Google Scholar] [CrossRef] [PubMed]
- Sekino, H.; Ishii, S.; Sato, H.; Nomoto, M.; Kawana, S.; Suenaga, H.; Kuroiwa, D.; Ito, H. Three cases of organized hematoma of the maxillary sinus in patients who underwent preoperative arterial embolization. Radiol. Case Rep. 2021, 16, 3945–3949. [Google Scholar] [CrossRef]
- Sinha, D.; Dasegowda, G.; Gayatri, Y.; Viswamitra, S. Sino nasal organizing hematoma masquerading as sino-nasal neoplasm. Indian J. Otolaryngol. Head Neck Surg. 2022, 74, 4669–4672. [Google Scholar] [CrossRef]
- James, J.; Shackelford, A.J.; Gudis, D.A.; Overdevest, J.B. Diagnostic dilemma—Sinonasal organizing hematoma. SAGE Open Med. Case Rep. 2020, 8, 2050313X20945843. [Google Scholar] [CrossRef]
- Hur, J.; Kim, J.K.; Byun, J.S.; Lee, W.J. Imaging characteristics of sinonasal organized hematoma. Acta Radiol. 2015, 56, 955–959. [Google Scholar] [CrossRef]
- Eissa, L.; Eid, M.; Razek, A.A.K.A. MR and CT imaging features of sino-nasal organized hematomas. Oral Radiol. 2021, 37, 297–304. [Google Scholar] [CrossRef]
- Kim, E.Y.; Kim, H.J.; Chung, S.K.; Dhong, H.J.; Kim, H.Y.; Yim, Y.J.; Kim, S.T.; Jeon, P.; Ko, Y.H. Sinonasal organized hematoma: CT and MR imaging findings. AJNR Am. J. Neuroradiol. 2008, 29, 1204–1208. [Google Scholar] [CrossRef]
- Pang, W.; Hu, L.; Wang, H.; Sha, Y.; Ma, N.; Wang, S.; Liu, Q.; Sun, X.; Wang, D. Organized hematoma: An analysis of 84 cases with emphasis on difficult prediction and favorable management. Otolaryngol. Head Neck Surg. 2016, 154, 626–633. [Google Scholar] [CrossRef]
- Suzuki, M.; Nakamura, Y.; Ozaki, S.; Yokota, M.; Murakami, S. Sinonasal organised haematoma: Clinical features and successful application of modified transnasal endoscopic medial maxillectomy. J. Laryngol. Otol. 2017, 131, 696–701. [Google Scholar] [CrossRef] [PubMed]
- Jeong, S.H.; Lee, D.H.; Lim, S.C. Endoscopic surgical treatment of maxillary sinus organized hematoma. J. Craniofac. Surg. 2021, 32, e687–e689. [Google Scholar] [CrossRef] [PubMed]
- Park, H.R.; Kshettry, V.R.; Farrell, C.J.; Lee, J.M.; Kim, Y.H.; Won, T.-B.; Han, D.H.; Do, H.; Nyguist, G.; Rosen, M.; et al. Clinical outcome after extended endoscopic endonasal resection of craniopharyngiomas: Two-institution experience. World Neurosurg. 2017, 103, 465–474. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.-M.; Lee, C.H.; Kim, Y.H.; Pae, S.H.; Won, T.-B. Feasibility of the nasoseptal flap for reconstruction of large anterior skull base defects in Asians. Acta Otolaryngol. 2012, 132, S69–S76. [Google Scholar] [CrossRef]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, K.Y.; Choi, S.; Jeong, S.; Won, T.-B. Successful Endoscopic Transsphenoidal Approach Treatment of Sphenoid Sinus Organized Hematoma Causing Visual Deficit: A Case Report. Medicina 2023, 59, 1802. https://doi.org/10.3390/medicina59101802
Choi KY, Choi S, Jeong S, Won T-B. Successful Endoscopic Transsphenoidal Approach Treatment of Sphenoid Sinus Organized Hematoma Causing Visual Deficit: A Case Report. Medicina. 2023; 59(10):1802. https://doi.org/10.3390/medicina59101802
Chicago/Turabian StyleChoi, Kyu Young, Sun Choi, Suji Jeong, and Tae-Bin Won. 2023. "Successful Endoscopic Transsphenoidal Approach Treatment of Sphenoid Sinus Organized Hematoma Causing Visual Deficit: A Case Report" Medicina 59, no. 10: 1802. https://doi.org/10.3390/medicina59101802




