A Prospective Study on the Impact of Clinical Factors and Adjusted Triple D System for Success Rate of ESWL
Abstract
1. Introduction
2. Materials and Methods
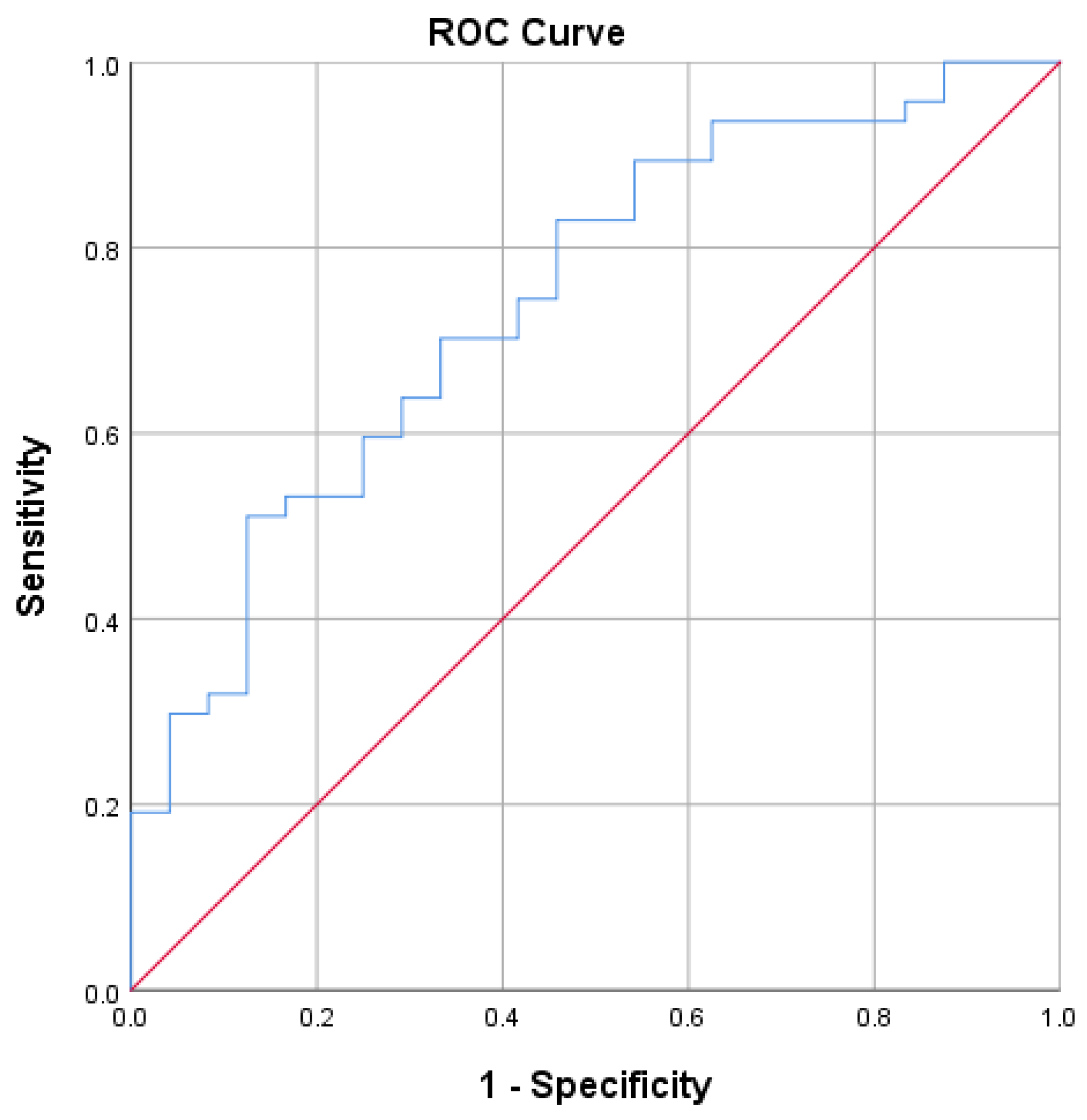
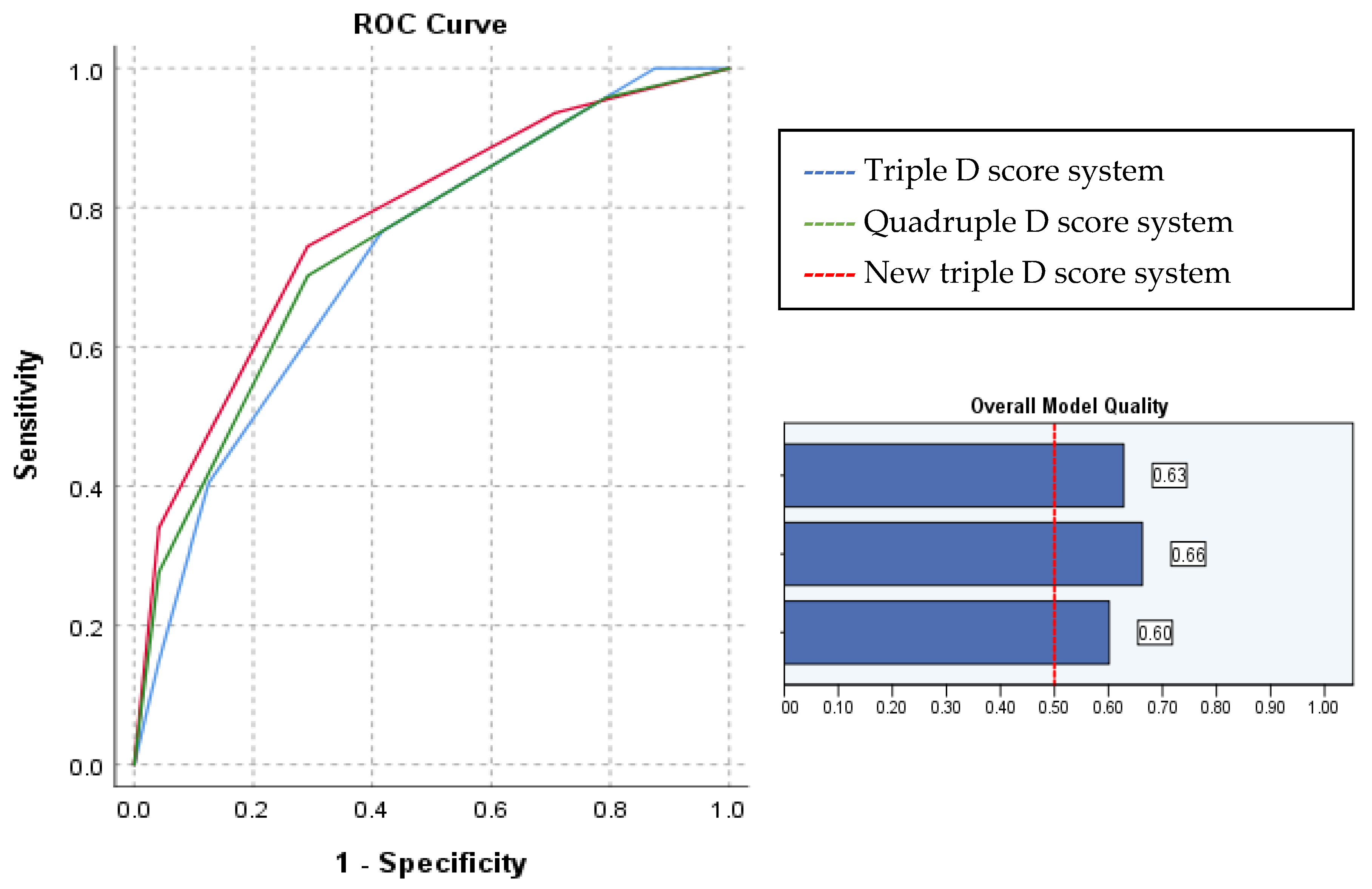
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Abufaraj, M.; Al Karmi, J.; Yang, L. Prevalence and trends of urolithiasis among adults. Curr. Opin. Urol. 2022, 32, 425–432. [Google Scholar] [CrossRef]
- Wagner, C.A. Etiopathogenic factors of urolithiasis. Arch. Esp. Urol. 2021, 74, 16–23, (In English and Spanish). [Google Scholar]
- Turk, C.; Petrik, A.; Sarica, K.; Seitz, C.; Skolarikos, A.; Straub, M.; Knoll, T. EAU guidelines on interventional treatment for urolithiasis. Eur. Urol. 2016, 69, 475–482. [Google Scholar] [CrossRef] [PubMed]
- Assimos, D.; Krambeck, A.; Miller, N.L.; Monga, M.; Murad, M.H.; Nelson, C.P.; Pace, K.T.; Pais, V.M.; Pearle, M.S.; Preminger, G.M.; et al. Surgical management of stones: American Urological Association/Endourological Society guideline, PART II. J. Urol. 2016, 196, 1161–1169. [Google Scholar] [CrossRef] [PubMed]
- Jung, H.D.; Lee, J.Y.; Kang, D.H.; Ko, K.; Koh, D.H.; Kwon, O.; Koo, K.C.; Kim, K.T.; Kim, M.S.; Kim, B.S.; et al. Korean Society of Endourology and Robotics (KSER) recommendation on the diagnosis, treatment, and prevention of urolithiasis. Investig. Clin. Urol. 2023, 64, 325–337. [Google Scholar] [CrossRef]
- Leavitt, D.; de la Rosette, J.; Hoenig, D. Strategies for nonmedical management of upper urinary tract calculi. In Campbell-Walsh’s Urology; Wein, A., Kavoussi, L., Partin, A., Peters, C., Eds.; Elsevier: Philadelphia, PA, USA, 2016; pp. 1235–1259. [Google Scholar]
- Pareek, G.; Armenakas, N.A.; Fracchia, J.A. Hounsfield units on computerized tomography predict stone-free rates after extracorporeal shock wave lithotripsy. J. Urol. 2003, 169, 1679–1681. [Google Scholar] [CrossRef] [PubMed]
- Pareek, G.; Hedican, S.P.; Lee, F.T., Jr.; Nakada, S.Y. Shock wave lithotripsy success determined by skin-to-stone distance on computed tomography. Urology 2005, 66, 941–944. [Google Scholar] [CrossRef] [PubMed]
- Ng, C.F.; Siu, D.Y.; Wong, A.; Goggins, W.; Chan, E.S.; Wong, K.T. Development of a scoring system from noncontrast computerized tomography measurements to improve the selection of upper ureteral stone for extracorporeal shock wave lithotripsy. J. Urol. 2009, 181, 1151–1157. [Google Scholar] [CrossRef] [PubMed]
- Pareek, G.; Armenakas, N.A.; Panagopoulos, G.; Bruno, J.J.; Fracchia, J.A. Extracorporeal shock wave lithotripsy success based on body mass index and Hounsfield units. Urology 2005, 65, 33–36. [Google Scholar] [CrossRef]
- Tran, T.Y.; McGillen, K.; Cone, E.B.; Pareek, G. Triple D Score is a reportable predictor of shockwave lithotripsy stone free rates. J. Endourol. 2015, 29, 226–230. [Google Scholar] [CrossRef]
- Gokce, M.I.; Esen, B.; Gulpinar, B.; Suer, E.; Gulpinar, O. External validation of Triple D Score in an elderly (≥65 years) population for prediction of success following shockwave lithotripsy. J. Endourol. 2016, 30, 1009–1016. [Google Scholar] [CrossRef]
- Ozgor, F.; Tosun, M.; Kayali, Y.; Savun, M.; Binbay, M.; Tepeler, A. External validation and evaluation of reliability and validity of the Triple D Score to predict stone-free status after extracorporeal shockwave lithotripsy. J. Endourol. 2017, 31, 169–173. [Google Scholar] [CrossRef]
- Ichiyanagi, O.; Fukuhara, H.; Kurokawa, M.; Izumi, T.; Suzuki, H.; Naito, S.; Nishida, H.; Kato, T.; Tsuchiya, N. Reinforcement of the Triple D score with simple addition of the intrarenal location for the prediction of the stone free rate after shockwave lithotripsy for renal stones 10–20 mm in diameter. Int. Urol. Nephrol. 2019, 51, 239–245. [Google Scholar] [CrossRef] [PubMed]
- Snicorius, M.; Bakavicius, A.; Cekauskas, A.; Miglinas, M.; Platkevicius, G.; Zelvys, A. Factors influencing extracorporeal shock wave lithotripsy efficiency for optimal patient selection. Videosurgery Other Miniinvasive Tech. 2021, 16, 409–416. [Google Scholar] [CrossRef]
- Keskin, S.K.; Spencer, M.; Lovegrove, C.; Turney, B.W. The New Lithotripsy Index predicts success of shock wave lithotripsy. World J. Urol. 2022, 40, 3049–3053. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.-Y.; Yang, Y.-H.; Lee, Y.-L.; Shen, J.-T.; Jang, M.-Y.; Shih, P.M.-C.; Wu, W.-J.; Chou, Y.-H.; Juan, Y.-S. Noncontrast computed tomography factors that predict the renal stone outcome after shock wave lithotripsy. Clin. Imaging 2015, 39, 845–850. [Google Scholar] [CrossRef]
- Shinde, S.; Al Balushi, Y.; Hossny, M.; Jose, S.; Al Busaidy, S. Factors affecting the outcome of extracorporeal shockwave lithotripsy in urinary stone treatment. Oman Med. J. 2018, 33, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Wagenius, M.; Oddason, K.; Utter, M.; Popiolek, M.; Forsvall, A.; Lundström, K.-J.; Linder, A. Factors influencing stone-free rate of Extracorporeal Shock Wave Lithotripsy (ESWL); a cohort study. Scand. J. Urol. 2022, 56, 237–243. [Google Scholar] [CrossRef]
- Abdel-Khalek, M.; Sheir, K.Z.; Mokhtar, A.A.; Eraky, I.; Kenawy, M.; Bazeed, M. Prediction of success rate after extracorporeal shock-wave lithotripsy of renal stones-a multivariate analysis model. Scand. J. Urol. Nephrol. 2004, 38, 161–167. [Google Scholar] [CrossRef]
- Mullhaupt, G.; Engeler, D.S.; Schmid, H.P.; Abt, D. How do stone attenuation and skin-to-stone distance in computed tomography influence the performance of shock wave lithotripsy in ureteral stone disease? BMC Urol. 2015, 15, 72. [Google Scholar] [CrossRef]
- Patel, T.; Kozakowski, K.; Hruby, G.; Gupta, M. Skin to stone distance is an independent predictor of stone-free status following shockwave lithotripsy. J. Endourol. 2009, 23, 1383–1385. [Google Scholar] [CrossRef] [PubMed]
- Nakasato, T.; Morita, J.; Ogawa, Y. Evaluation of hounsfield units as a predictive factor for the outcome of extracorporeal shock wave lithotripsy and stone composition. Urolithiasis 2015, 43, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Wiesenthal, J.D.; Ghiculete, D.; Ray, A.A.; Honey, R.J.; Pace, K.T. A clinical nomogram to predict the successful shock wave lithotripsy of renal and ureteral calculi. J. Urol. 2011, 186, 556–562. [Google Scholar] [CrossRef] [PubMed]
- El-Nahas, A.R.; El-Assmy, A.M.; Mansour, O.; Sheir, K.Z. A prospective multivariate analysis of factors predicting stone disintegration by extracorporeal shock wave lithotripsy: The value of high-resolution noncontrast computed tomography. Eur. Urol. 2007, 51, 1688–1693. [Google Scholar] [CrossRef]
- Perks, A.E.; Schuler, T.D.; Lee, J.; Ghiculete, D.; Chung, D.G.; Honey, R.J.D.A.; Pace, K.T. Stone attenuation and skin-to-stone distance on computed tomography predicts for stone fragmentation by shock wave lithotripsy. Urology 2008, 72, 765–769. [Google Scholar] [CrossRef]
- Rodríguez-Plata, I.T.; Medina-Escobedo, M.; Basulto-Martínez, M.; Avila-Nava, A.; Gutiérrez-Solis, A.L.; Méndez-Domínguez, N.; Lugo, R. Implementation of a Technique Based on Hounsfield Units and Hounsfield Density to Determine Kidney Stone Composition. Tomography 2021, 7, 606–613. [Google Scholar] [CrossRef]
- Shahnani, P.S.; Karami, M.; Astane, B.; Janghorbani, M. The comparative survey of Hounsfield units of stone composition in urolithiasis patients. J. Res. Med. Sci. 2014, 19, 650–653. [Google Scholar]
- Muter, S.; Abd, Z.; Saeed, R. Renal stone density on native CT-scan as a predictor of treatment outcomes in shock wave lithotripsy. J. Med. Life 2022, 15, 1579–1584. [Google Scholar] [CrossRef] [PubMed]
- Cho, K.S.; Jung, H.D.; Ham, W.S.; Chung, D.Y.; Kang, Y.J.; Jang, W.S.; Kwon, J.K.; Choi, Y.D.; Lee, J.Y. Optimal skin-to-stone distance is a positive predictor for successful outcomes in upper ureter calculi following extracorporeal shock wave lithotripsy: A bayesian model averaging approach. PLoS ONE 2015, 10, e0144912. [Google Scholar] [CrossRef]
- Choi, J.W.; Song, P.H.; Kim, H.T. Predictive factors of the outcome of extracorporeal shockwave lithotripsy for ureteral stones. Korean J. Urol. 2012, 53, 424–430. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.Y.; Kim, J.H.; Kang, D.H.; Chung, D.Y.; Lee, D.H.; Jung, H.D.; Kwon, J.K.; Cho, K.S. Stone heterogeneity index as the standard deviation of Hounsfield units: A novel predictor for shock-wave lithotripsy outcomes in ureter calculi. Sci. Rep. 2016, 6, 23988. [Google Scholar] [CrossRef] [PubMed]
- Yamashita, S.; Kohjimoto, Y.; Iguchi, T.; Nishizawa, S.; Iba, A.; Kikkawa, K.; Hara, I. Variation Coefficient of Stone Density: A Novel Predictor of the Outcome of Extracorporeal Shockwave Lithotripsy. J. Endourol. 2017, 31, 384–390. [Google Scholar] [CrossRef] [PubMed]
| Variable | All Patients (N = 71) | Successful Treatment (N = 47) | Treatment Failure (N = 24) | p-Value * |
|---|---|---|---|---|
| Age [years] Mean ± SD | 50.85 (13.65) | 50.81 (14.40) | 50.92 (12.35) | 0.975 |
| Gender, N (%): Male Female | 46 (64.8%) 25 (35.2%) | 34 (72.3%) 13 (27.7%) | 12 (50%) 12 (50%) | 0.072 |
| BMI Mean ± SD | 26.76 (4.34) | 25.98 (3.87) | 28.18 (4.87) | 0.239 |
| Stone location, N (%): | 0.443 | |||
| Other | 26 (36.6%) | 18 (69.2%) | 8 (30.8%) | |
| Lower calyx | 45 (63.4%) | 29 (64.2%) | 16 (35.6%) | |
| Max. stone diameter [mm] Mean (± SD) | 8.58 (3.07) | 7.732 (2.84) | 10.229 (2.82) | 0.001 |
| Stone volume [mm3] Mean (± SD) | 196.40 (191.74) | 151.340 (159.56) | 284.625 (220.67) | 0.005 |
| Mean stone density [HU] (± SD) | 752.28 (271.58) | 689.57 (261.44) | 875.08 (252.97) | 0.006 |
| Skin to stone distance [mm] Mean (± SD) | 100.62 (19.81) | 97.94 (18.05) | 105.88 (22.36) | 0.111 |
| SMLI Mean (± SD) | 310.45 (105.61) | 293.96 (133.63) | 318.87 (100.80) | 0.349 |
| SMLI/stone volume ratio Mean (± SD) | 3.30 (2.85) | 4.02 (3.08) | 1.87 (1.58) | 0.002 |
| Clinical Factor | Treatment Efficacy | N of Cases | Mean (SD) | p-Value | Stone-Free after Treatment | N of Cases | Mean (SD) | p-Value |
|---|---|---|---|---|---|---|---|---|
| SSD | SFR or fragments <4 mm | 47 | 97.94 18.05 | 0.111 | Totally stone free | 18 | 96.17 15.23 | 0.273 |
| Fragments >4 mm | 24 | 105.88 22.36 | Residual fragments | 53 | 102.13 21.06 | |||
| MSD | SFR or fragments <4 mm | 47 | 7.73 2.84 | 0.001 | Totally stone free | 18 | 6.94 2.34 | 0.003 |
| Fragments >4 mm | 24 | 10.23 2.88 | Residual fragments | 53 | 9.13 3.11 | |||
| SV | SFR or fragments <4 mm | 47 | 151.34 159.56 | 0.005 | Totally stone free | 18 | 113.38 131.56 | 0.01 |
| Fragments >4 mm | 24 | 284.63 220.67 | Residual fragments | 53 | 224.58 201.58 | |||
| MD | SFR or fragments <4 mm | 47 | 689.57 261.44 | 0.006 | Totally stone free | 18 | 661.33 245.07 | 0.087 |
| Fragments >4 mm | 24 | 875.08 252.97 | Residual fragments | 53 | 783.17 275.335 | |||
| Maximum HU score | SFR or fragments <4 mm | 47 | 961.64 369.30 | 0.009 | Totally stone free | 18 | 975.06 365.286 | 0.375 |
| Fragments >4 mm | 24 | 1191.83 268.18 | Residual fragments | 53 | 1061.3 350.86 | |||
| SMLI/SV ratio | SFR or fragments <4 mm | 47 | 4.02 3.08 | 0.002 | Totally stone free | 18 | 5.32 3.72 | 0.009 |
| Fragments >4 mm | 24 | 1.87 1.58 | Residual fragments | 53 | 2.60 2.08 |
| Variable | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p Value | OR | 95% CI | p Value | |
| SV | 0.99 | 0.99–1.00 | 0.012 | 1.00 | 0.99–1.00 | 0.670 |
| Maximum diameter of stone | 0.75 | 0.62–0.90 | 0.002 | 0.77 | 0.52–1.13 | 0.174 |
| MD | 0.99 | 0.99–1.00 | 0.009 | 0.99 | 0.99–1.00 | 0.176 |
| SSD | 0.98 | 0.95–1.01 | 0.115 | 0.98 | 0.95–1.01 | 0.250 |
| SMLI/SV ratio | 1.58 | 1.15–2.17 | 0.005 | 1.06 | 0.68–1.65 | 0.811 |
| Sum of SMLI | 1.01 | 1.00–1.01 | 0.340 | 1.01 | 0.99–1.01 | 0.210 |
| Triple D Score | Successful Treatment | Treatment Failure % |
|---|---|---|
| 0 | 33% (2/6) | 67% (4/6) |
| 1 | 48% (12/25) | 52% (13/25) |
| 2 | 76.9% (20/26) | 23.1% (6/26) |
| 3 | 92.9% (13/14) | 7.1% (1/14) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Snicorius, M.; Drevinskaitė, M.; Miglinas, M.; Čekauskas, A.; Urbonienė, V.; Bandzevičiūtė, R.; Čeponkus, J.; Šablinskas, V.; Želvys, A. A Prospective Study on the Impact of Clinical Factors and Adjusted Triple D System for Success Rate of ESWL. Medicina 2023, 59, 1827. https://doi.org/10.3390/medicina59101827
Snicorius M, Drevinskaitė M, Miglinas M, Čekauskas A, Urbonienė V, Bandzevičiūtė R, Čeponkus J, Šablinskas V, Želvys A. A Prospective Study on the Impact of Clinical Factors and Adjusted Triple D System for Success Rate of ESWL. Medicina. 2023; 59(10):1827. https://doi.org/10.3390/medicina59101827
Chicago/Turabian StyleSnicorius, Marius, Mingailė Drevinskaitė, Marius Miglinas, Albertas Čekauskas, Vidita Urbonienė, Rimantė Bandzevičiūtė, Justinas Čeponkus, Valdas Šablinskas, and Arunas Želvys. 2023. "A Prospective Study on the Impact of Clinical Factors and Adjusted Triple D System for Success Rate of ESWL" Medicina 59, no. 10: 1827. https://doi.org/10.3390/medicina59101827
APA StyleSnicorius, M., Drevinskaitė, M., Miglinas, M., Čekauskas, A., Urbonienė, V., Bandzevičiūtė, R., Čeponkus, J., Šablinskas, V., & Želvys, A. (2023). A Prospective Study on the Impact of Clinical Factors and Adjusted Triple D System for Success Rate of ESWL. Medicina, 59(10), 1827. https://doi.org/10.3390/medicina59101827






