Comparative Evaluation of the Efficacy of Combined Intramedullary Pinning with K-Wires Pinning in the Treatment of Fifth Metacarpal Neck Fractures versus Conventional Techniques—K-Wires Pinning and Intramedullary Pinning
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
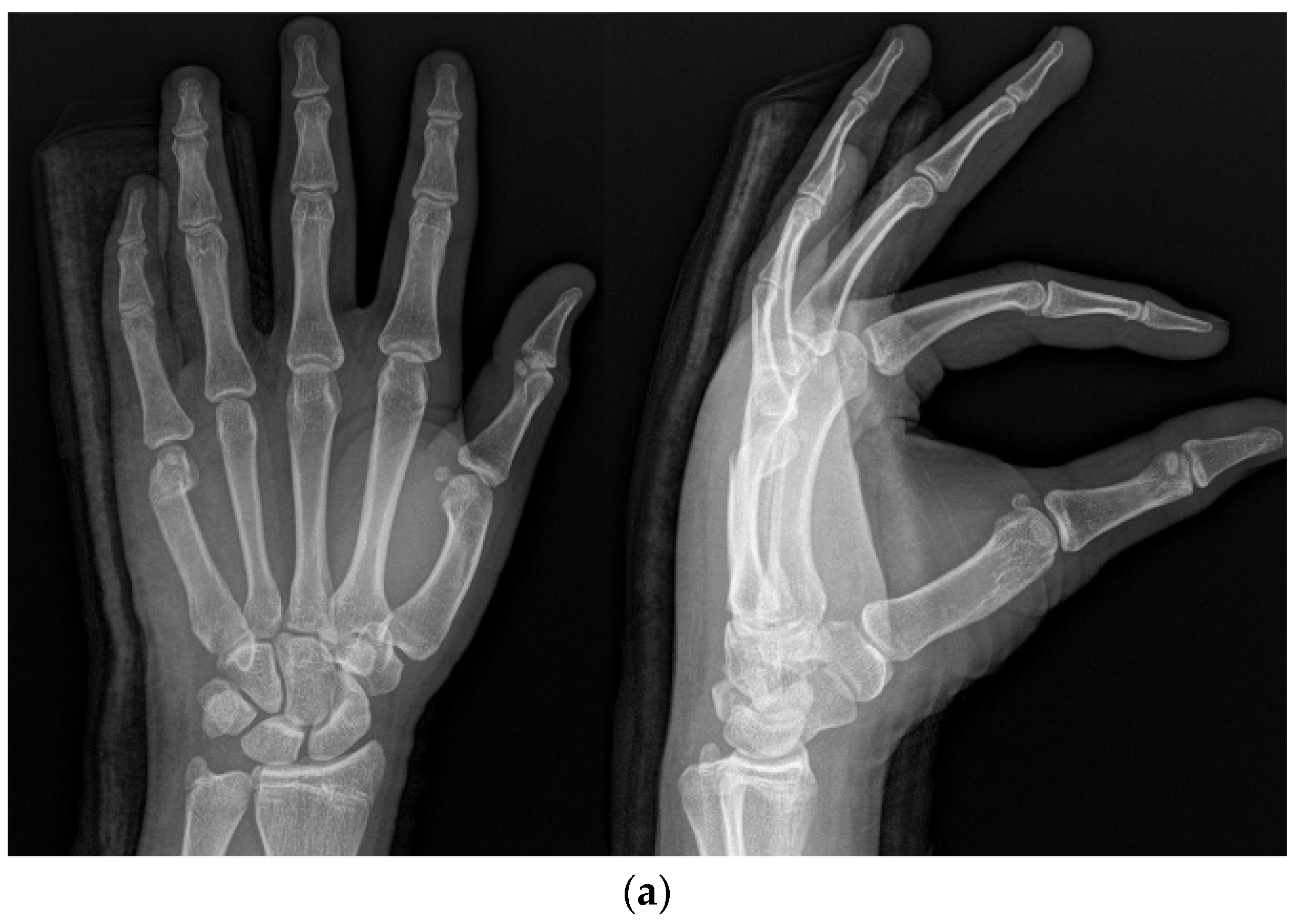
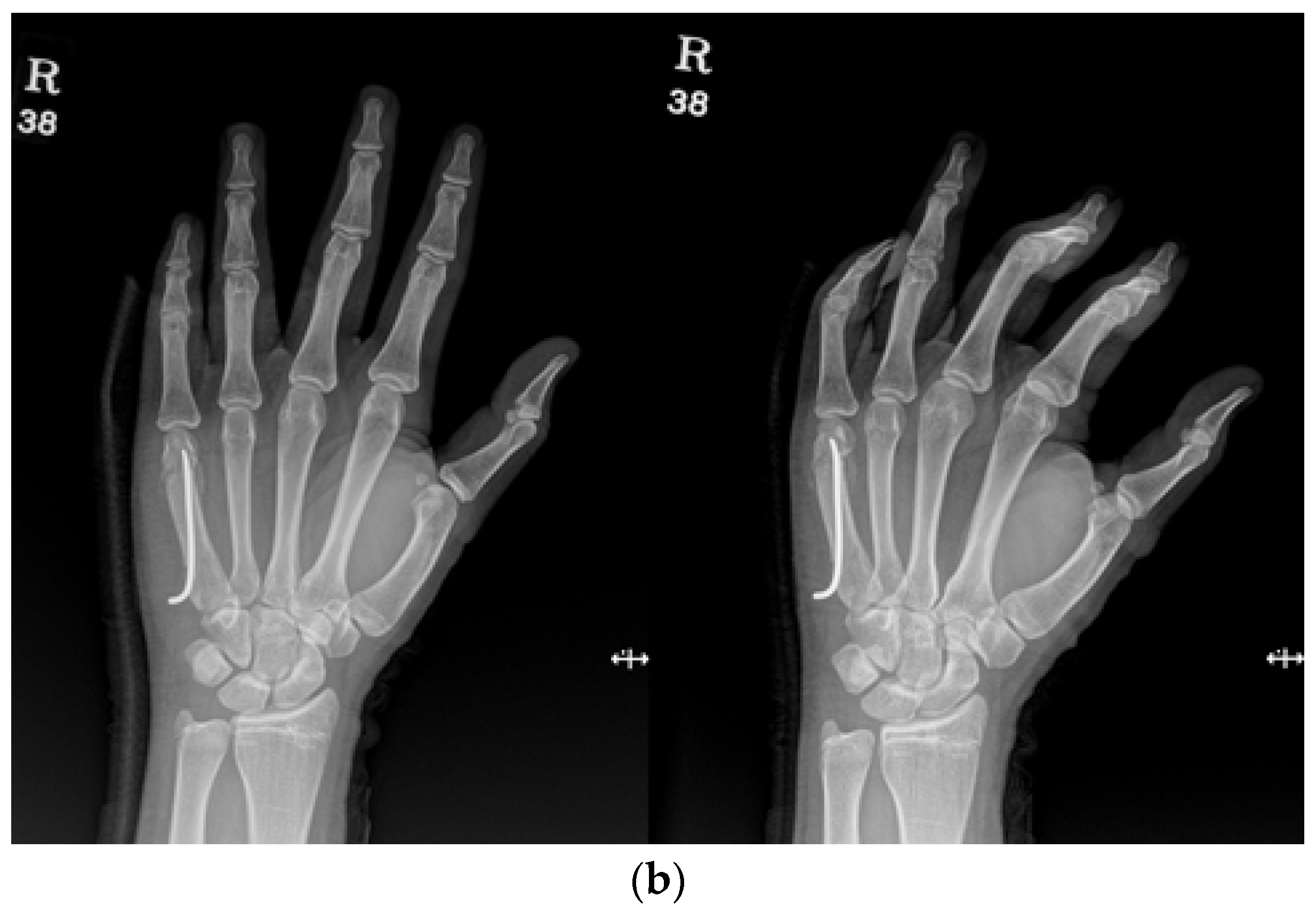
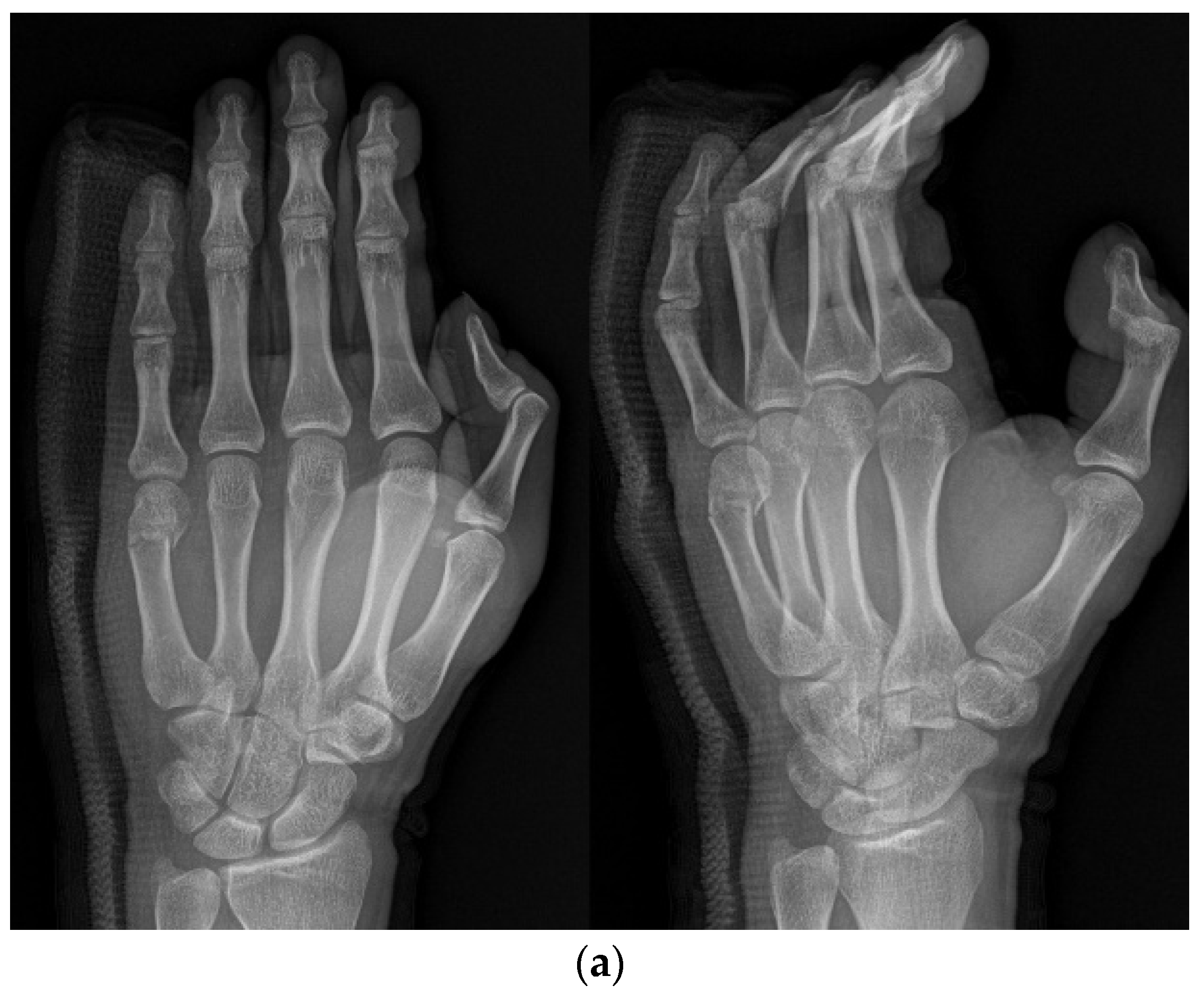
2.2. Methods
2.3. Surgical Technique
2.4. Statistical Analysis
3. Results
4. Discussion
5. Limitation
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Boussakri, H.; Elidrissi, M.; Azarkane, M.; Bensaad, S.; Bachiri, M.; Shimi, M.; Elibrahimi, A.; Elmrini, A. Fractures of the neck of the fifth metacarpal bone, treated by percutaneous intramedullary nailing: Surgical technique, radiological and clinical results study (28 cases). Pan Afr. Med. J. 2014, 18, 187. [Google Scholar] [CrossRef] [PubMed]
- Galal, S.; Safwat, W. Transverse pinning versus intramedullary pinning in fifth metacarpal’s neck fractures: A randomized controlled study with patient-reported outcome. J. Clin. Orthop. Trauma 2017, 8, 339–343. [Google Scholar] [CrossRef] [PubMed]
- Winter, M.; Balaguer, T.; Bessière, C.; Carles, M.; Lebreton, E. Surgical treatment of the boxer’s fracture: Transverse pinning versus intramedullary pinning. J. Hand Surg. 2007, 32, 709–713. [Google Scholar] [CrossRef] [PubMed]
- Sletten, I.N. Assessment of volar angulation and shortening in the 5th metacarpal neck fractures: An inter- and intra- observer validity and reliability study. J. Hand Surg. 2012, 38, 658–666. [Google Scholar] [CrossRef] [PubMed]
- Padegimas, E.M.; Warrender, W.J.; Jones, C.M.; Ilyas, A.M. Metacarpal Neck Fractures: A Review of Surgical Indications and Techniques. Arch. Trauma Res. 2016, 5, e32933. [Google Scholar] [CrossRef] [PubMed]
- Fan, X.L.; Wang, J.; Zhang, D.H.; Mao, F.; Liao, Y.; Xiao, R. Antegrade intramedullary fixation for adolescent fifth metacarpal neck fracture and its impact on epiphyseal growth. BMC Musculoskelet. Disord. 2021, 22, 546. [Google Scholar] [CrossRef]
- Malik, S. Fifth Metacarpal Fracture (Boxers Fracture); StatPearls: Tampa, FL, USA, 2020. [Google Scholar]
- Chiu, Y.C.; Tsai, M.T.; Hsu, C.E.; Hsu, H.C.; Huang, H.L.; Hsu, J.T. New fixation approach for transverse metacarpal neck fracture: A biomechanical study. J. Orthop. Surg. Res. 2018, 13, 183. [Google Scholar] [CrossRef]
- Page, S.M.; Stern, P.J. Complications and range of motion following plate fixation of metacarpal and phalangeal fractures. J. Hand. Surg. Am. 1998, 23, 827–832. [Google Scholar] [CrossRef]
- Zeng, L.; Zeng, L.; Miao, X.; Chen, Y.; Liang, W.; Jiang, Y. Single versus dual elastic nails for closed reduction and antegrade intramedullary nailing of displaced fifth metacarpal neck fractures. Sci. Rep. 2021, 11, 1778. [Google Scholar] [CrossRef]
- Eisenschenk, A.; Spitzmüller, R.; Güthoff, C.; Obladen, A.; Kim, S.; Henning, E.; Dornberger, J.E.; Stengel, D. Single versus dual Kirschner wires for closed reduction and intramedullary nailing of displaced fractures of the fifth metacarpal neck (1–2 KiWi): A randomized controlled trial. Bone Jt. J. 2019, 101, 1263–1271. [Google Scholar] [CrossRef]
- Lee, S.J.; Merrison, H.; Williams, K.A.; Vuillermin, C.B.; Bauer, A.S. Closed Reduction and I mmobilization of Pediatric Fifth Metacarpal Neck Fractures. HAND 2022, 17, 416–421. [Google Scholar] [CrossRef] [PubMed]
- Choi, N.Y.; Song, H.S. Treatment of Metacarpal Fractures using Transverse Kirschner-wire Fixation. J. Korean Orthop. Assoc. 2007, 42, 608–615. [Google Scholar] [CrossRef]
- Mohammed, R.; Farook, M.Z.; Newman, K. Percutaneous elastic intramedullary nailing of metacarpal fractures: Surgical technique and clinical results study. J. Orthop. Surg. Res. 2011, 6, 37. [Google Scholar] [CrossRef] [PubMed]
- Birndorf, M.S.; Daley, R.; Greenwald, D.P. Metacarpal fracture angulation decreases flexor mechanical efficiency in human hands. Plast. Reconstr. Surg. 1997, 99, 1079–1083. [Google Scholar] [CrossRef] [PubMed]
- Zong, S.L.; Zhao, G.; Su, L.X.; Liang, W.D.; Li, L.G.; Cheng, G.; Wang, A.J.; Cao, X.Q.; Zheng, Q.T.; Li, L.D.; et al. Treatments for the fifth metacarpal neck fractures: A network meta-analysis of randomized controlled trials. Medicine 2016, 95, e3059. [Google Scholar] [CrossRef] [PubMed]
- De Jonge, J.J.; Kingma, J.; van der Lei, B.; Klasen, H.J. Fractures of the metacarpals. A retrospective analysis of incidence and aetiology and a review of the English language literature. Injury 1994, 25, 365–369. [Google Scholar] [CrossRef]
- Potenza, V.; Caterini, R.; De Maio, F.; Bisicchia, S.; Farsetti, P. Fractures of the neck of the fifth metacarpal bone. Medium-term results in 28 cases treated by percutaneous transverse pinning. Injury 2012, 43, 242–245. [Google Scholar] [CrossRef]
- Wong, T.C.; Ip, F.K.; Yeung, S.H. Comparison between percutaneous transverse fixation and intramedullary K-wires in treating closed fractures of the metacarpal neck of the little finger. J. Hand. Surg. 2006, 31, 61–65. [Google Scholar] [CrossRef]
- Zemirline, A.; Vaiss, L.; Lebailly, F.; Gouzou, S.; Liverneaux, P.A.; Facca, S. The MetaHUS fixation system versus pinning and plating in 5th metacarpal neck fractures. Chirurgie de la Main 2014, 33, 207–210. [Google Scholar] [CrossRef]
- Ajay, K.; Balaram, M.D.; Michael, S.; Bednar, M.D. Complications After the Fractures of Metacarpal and Phalanges. Hand Clin. 2010, 26, 169–177. [Google Scholar]
- Singh, A.K.; Narsaria, N.; Arun, G.R.; Seth, R.R.S. Outcome of displaced metacarpal and proximal phalangeal fractures treated with intramedullary K-wire and cross Kwires: A prospective study of 105 patients. Int. J. Orthopaed. 2014, 1, 25–30. [Google Scholar]
- Braakman, M. Are lateral X-rays useful in the treatment of fractures of the fourth and fifth metacarpals? Injury 1998, 29, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Ozer, K.; Gillani, S.; Williams, A.; Peterson, S.L.; Morgan, S. Comparison of intramedullary nailing versus platescrew fixation of extra-articular metacarpal fractures. J. Hand. Surg. Am. 2008, 33, 1724–1731. [Google Scholar] [CrossRef] [PubMed]
- Hofmeister, E.P.; Kim, J.; Shin, A.Y. Comparison of 2 methods of i mmobilization of fifth metacarpal neck fractures: A prospective randomized study. J. Hand. Surg. Am. 2008, 33, 1362–1368. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.J.; Lee, Y.H.; Change, H.G.; Lee, C.J.; Cho, W.H. The 5th metacarpal neck fracture treated by closed reduction and percutaneous intramedullary K-wire fixation. J. Korean Soc. Fract. 1995, 8, 696–704. [Google Scholar] [CrossRef]
- Green, D.P.; Rowland, S.A. Fractures of the phalanges and metacarapals. In Fractures in Adults, 3rd ed.; J.B. Lippincott Co.: Philadelphia, PA, USA, 1991; pp. 441–562. [Google Scholar]
- Stern, P.J. Fracture of the metacarpals and phalanges. In Operative Hand Surgery, 3rd ed.; Churchill Livingstone: New York, NY, USA, 1993; pp. 695–758. [Google Scholar]



| Variable | KP (n = 60) | IP (n = 50) | IPKP (n = 48) | p-Value |
|---|---|---|---|---|
| Quick-DASH | 2.3 (±2.1) | 2.5 (±1.7) | 1.9 (±1.6) | <0.001 |
| ROM (TAM) | 272.6° (±17.5) | 271.1° (±18.0) | 274.1° (±14.9) | 0.42 |
| Angulation (Pre-op) | 42.5° (±3.7) | 40.8° (±4.4) | 43.6° (±5.3) | 0.09 |
| Angulation (Immediate) | 13.1° (±5.6) | 13.1° (±5.1) | 10.3° (±4.0) | 0.04 |
| Angulation (1 year f/u) | 15.7° (±7.7) | 17.0° (±5.9) | 12.6° (±2.5) | <0.001 |
| Shortening (Pre-op) | 2.8 mm (±0.3) | 2.8 mm (±0.4) | 2.6 mm (±0.4) | 0.26 |
| Shortening (Immediate) | 0.5 mm (±0.5) | 0.7 mm (±0.4) | 0.3 mm (±0.2) | <0.001 |
| Shortening (1 year f/u) | 0.9 mm (±0.3) | 1.4 mm (±0.2) | 0.4 mm (±0.1) | <0.001 |
| Duration of surgery (min) | 13.2 (±3.2) | 10.6 (±2.5) | 15.3 (±3.1) | 0.07 |
| Cosmetic score | 3.7 (±1.2) | 3.8 (±0.9) | 4.7 (±0.8) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, D.-E.; Lee, T.-J.; Na, Y.; Noh, Y.-G. Comparative Evaluation of the Efficacy of Combined Intramedullary Pinning with K-Wires Pinning in the Treatment of Fifth Metacarpal Neck Fractures versus Conventional Techniques—K-Wires Pinning and Intramedullary Pinning. Medicina 2023, 59, 1944. https://doi.org/10.3390/medicina59111944
Kim D-E, Lee T-J, Na Y, Noh Y-G. Comparative Evaluation of the Efficacy of Combined Intramedullary Pinning with K-Wires Pinning in the Treatment of Fifth Metacarpal Neck Fractures versus Conventional Techniques—K-Wires Pinning and Intramedullary Pinning. Medicina. 2023; 59(11):1944. https://doi.org/10.3390/medicina59111944
Chicago/Turabian StyleKim, Dong-Eun, Tong-Joo Lee, Yeop Na, and Ye-Geon Noh. 2023. "Comparative Evaluation of the Efficacy of Combined Intramedullary Pinning with K-Wires Pinning in the Treatment of Fifth Metacarpal Neck Fractures versus Conventional Techniques—K-Wires Pinning and Intramedullary Pinning" Medicina 59, no. 11: 1944. https://doi.org/10.3390/medicina59111944
APA StyleKim, D.-E., Lee, T.-J., Na, Y., & Noh, Y.-G. (2023). Comparative Evaluation of the Efficacy of Combined Intramedullary Pinning with K-Wires Pinning in the Treatment of Fifth Metacarpal Neck Fractures versus Conventional Techniques—K-Wires Pinning and Intramedullary Pinning. Medicina, 59(11), 1944. https://doi.org/10.3390/medicina59111944





