An Evaluation of the Effectiveness of Melatonin and n-Acetylcysteine in Cerebral Ischemia-Reperfusion Injury in Adult Rats
Abstract
:1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Experimental Protocol
2.3. Chemicals Employed in the Experiments
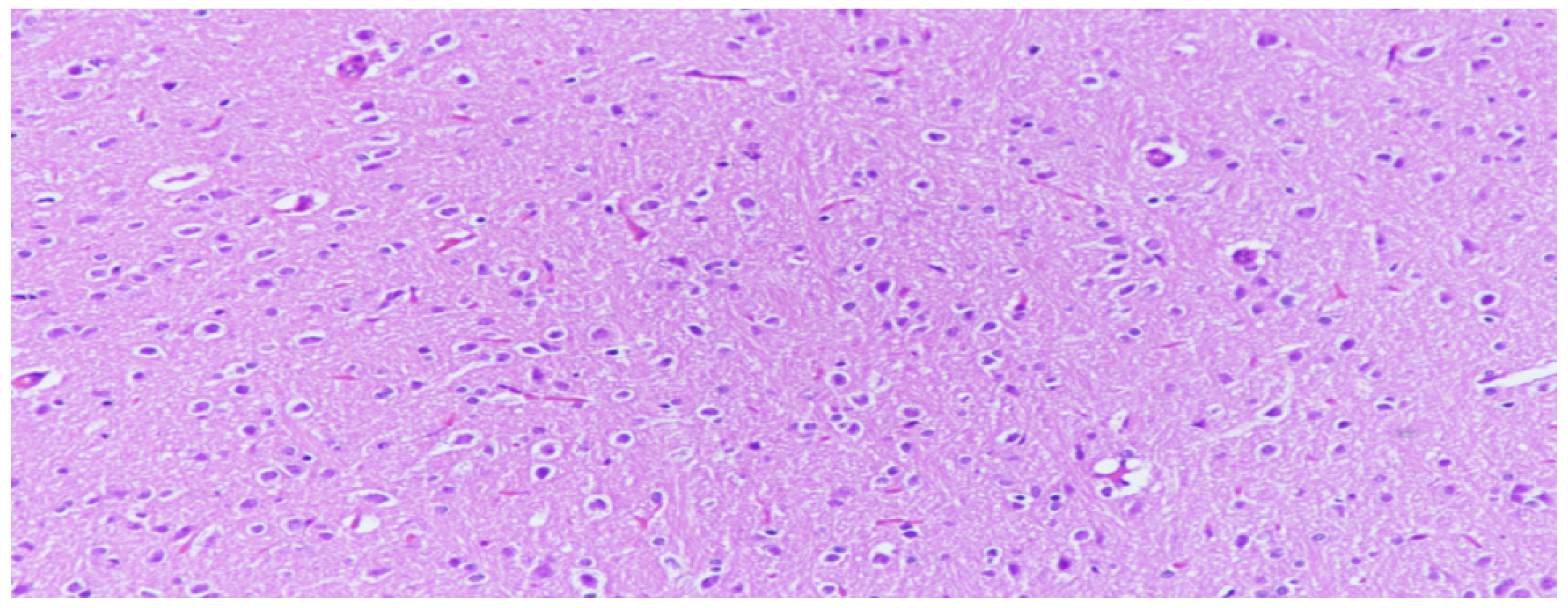
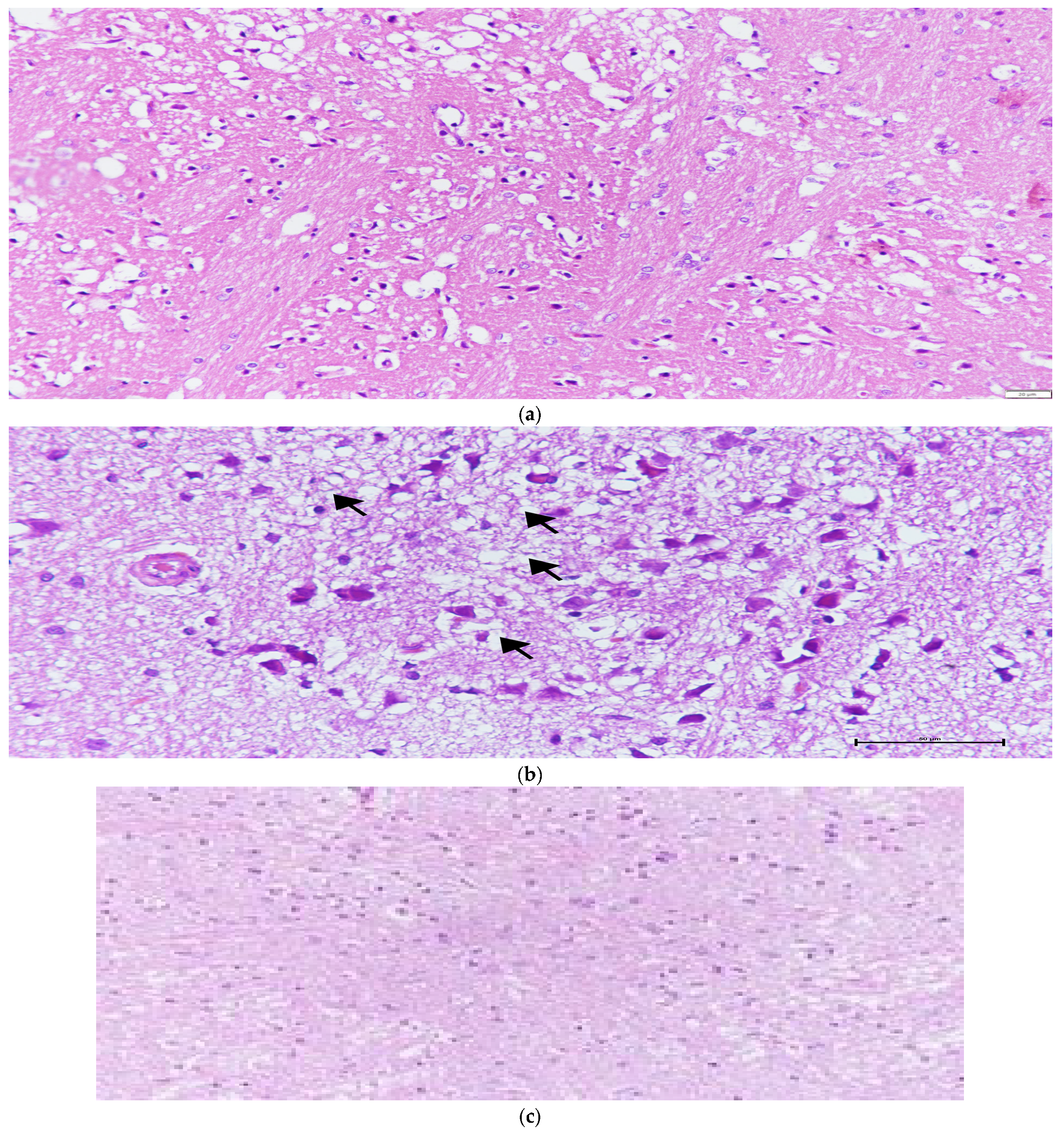
2.4. Histopathological and Immunohistochemical Analysis
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Barroso-Aranda, J.; Schmid-Schönbein, G.W.; Zweifach, B.W.; Engler, R.L. Granulocytes and no-reflow phenomenon in irreversible hemorrhagic shock. Circ. Res. 1988, 63, 437–447. [Google Scholar] [CrossRef] [PubMed]
- Epstein, F.H.; McCord, J.M. Oxygen-Derived Free Radicals in Postischemic Tissue Injury. N. Engl. J. Med. 1985, 312, 159–163. [Google Scholar] [CrossRef] [PubMed]
- Chouchani, E.T.; Pell, V.R.; James, A.M.; Work, L.M.; Saeb-Parsy, K.; Frezza, C.; Krieg, T.; Murphy, M.P. A Unifying Mechanism for Mitochondrial Superoxide Production during Ischemia-Reperfusion Injury. Cell Metab. 2016, 23, 254–263. [Google Scholar] [CrossRef] [PubMed]
- Bilbao, G.; Contreras, J.L.; Eckhoff, D.E.; Mikheeva, G.; Krasnykh, V.; Douglas, J.T.; Thomas, F.T.; Thomas, J.M.; Curiel, D.T. Reduction of Ischemia-Reperfusion Injury of the Liver by In Vivo Adenovirus-Mediated Gene Transfer of the Antiapoptotic Bcl-2 Gene. Ann. Surg. 1999, 230, 185–193. [Google Scholar] [CrossRef]
- McMillen, M.A.; Huribal, M.; Sumpio, B. Common pathway of endothelial-leukocyte interaction in shock, ischemia, and reperfusion. Am. J. Surg. 1993, 166, 557–562. [Google Scholar] [CrossRef]
- Collard, C.D.; Gelman, S. Pathophysiology, Clinical Manifestations, and Prevention of Ischemia-Reperfusion Injury. Anesthesiology 2001, 94, 1133–1138. [Google Scholar] [CrossRef]
- Jaeschke, H. Molecular mechanisms of hepatic ischemia-reperfusion injury and preconditioning. Am. J. Physiol. Gastrointest. Liver Physiol. 2003, 284, G15–G26. [Google Scholar] [CrossRef]
- Nduhirabandi, F.; Lamont, K.; Albertyn, Z.; Opie, L.H.; Lecour, S. Role of toll-like receptor 4 in melatonin-induced cardioprotection. J. Pineal Res. 2016, 60, 39–47. [Google Scholar] [CrossRef]
- Pandi-Perumal, S.R.; Srinivasan, V.; Maestroni, G.J.M.; Cardinali, D.P.; Poeggeler, B.; Hardeland, R. Melatonin: Nature’s most versatile biological signal? FEBS J. 2006, 273, 2813–2838. [Google Scholar] [CrossRef]
- Conti, A.; Conconi, S.; Hertens, E.; Markowska, M.; Maestroni, G.J.; Skwarlo-Sonta, K. Evidence for melatonin synthesis in mouse and human bone marrow cells. J. Pineal Res. 2000, 28, 193–202. [Google Scholar] [CrossRef]
- Lindsey, R.W.; Gugala, Z.; Pneumaticos, S.G. Injury to the vertebrae and spinal cord. Trauma 2004, 459–492. [Google Scholar]
- Hutton, L.C.; Abbass, M.; Dickinson, H.; Ireland, Z.; Walker, D. Neuroprotective properties of melatonin in a model of birth asphyxia in the spiny mouse (Acomys cahirinus). Dev. Neurosci. 2009, 31, 437–451. [Google Scholar] [CrossRef] [PubMed]
- Kilic, E.; Uzdemir, Y.G.Ö.; Bolay, H.; Keleştimur, H.; Dalkara, T. Pinealectomy aggravates and melatonin administration attenuates brain damage in focal ischemia. J. Cereb. Blood Flow Metab. 1999, 19, 511–516. [Google Scholar] [CrossRef] [PubMed]
- Hazinedaroglu, S.M.; Dulger, F.; Kayaoglu, H.A.; Pehlivan, M.; Serinsoz, E.; Canbolat, O.; Erverdi, N. N-Acetylcysteine in intestinal reperfusion injury: An experimental study in rats. ANZ J. Surg. 2004, 74, 676–678. [Google Scholar] [CrossRef] [PubMed]
- Cuzzocrea, S.; Mazzon, E.; Costantino, G.; Serraino, I.; De Sarro, A.; Caputi, A.P. Effects of n-acetylcystein e in a rat model of ischemia and reperfusion injury. Cardiovasc. Res. 2000, 47, 537–548. [Google Scholar] [CrossRef] [PubMed]
- Yildirim, Z.; Kotuk, M.; Iraz, M.; Kuku, I.; Ulu, R.; Armutcu, F.; Ozen, S. Attenuation of bleomycin-induced lung fibrosis by oral sulfhydryl containing antioxidants in rats: Erdosteine and N-acetylcysteine. Pulm. Pharmacol. Ther. 2005, 18, 367–373. [Google Scholar] [CrossRef]
- Cakir, O.; Erdem, K.; Oruc, A.; Oruc, A.; Kilinc, N.; Eren, N. Neuroprotective effect of N-acetylcysteine and hypothermia on the spinal cord ischemia—Reperfusion injury. Cardiovasc. Surg. 2003, 11, 375–379. [Google Scholar]
- Sung, J.-H.; Shah, F.-A.; Gim, S.-A.; Koh, P.-O. Identification of proteins in hyperglycemia and stroke animal models. J. Surg. Res. 2016, 200, 365–373. [Google Scholar] [CrossRef]
- Cetin, C.; Erdogan, A.M.; Dincel, G.C.; Bakar, B.; Kisa, U. Effects of Sulphasalazine in Cerebral Ischemia Reperfusion Injury in Rat. Arch. Med. Res. 2017, 48, 247–256. [Google Scholar] [CrossRef]
- Korthuis, R.J.; Granger, D.N. Mechanisms of Ischemia/reperfusion. Annu. Rev. Physiol. 1995, 57, 311–332. [Google Scholar]
- Carloni, S.; Perrone, S.; Buonocore, G.; Buonocore, G.; Longini, M.; Proietti, F.; Balduini, W. Melatonin protects from the long-term consequences of a neonatal hypoxic-ischemic brain injury in rats. J. Pineal Res. 2008, 44, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Pei, Z.; Ho, H.T.; Cheung, R.T. Pre-treatment with melatonin reduces volume of cerebral infarction in a permanent middle cerebral artery occlusion stroke model in the rat. Neurosci. Lett. 2002, 318, 141–144. [Google Scholar] [CrossRef] [PubMed]
- Kilic, E.; Kilic, Ü.; Reiter, R.J.; Bassetti, C.L.; Hermann, D.M. Prophylactic use of melatonin protects against focal cerebral ischemia in mice: Role of endothelin converting enzyme-1. J. Pineal Res. 2004, 37, 247–251. [Google Scholar] [CrossRef]
- Reiter, R.J.; Tan, D.X.; Leon, J.; Kilic, Ü.; Kilic, E. When melatonin gets on your nerves: Its beneficial actions in experimental models of stroke. Exp. Biol. Med. 2005, 230, 104–117. [Google Scholar] [CrossRef] [PubMed]
- Cheung, R.T.F. The utility of melatonin in reducing cerebral damage resulting from ischemia and reperfusion. J. Pineal Res. 2003, 34, 153–160. [Google Scholar] [CrossRef]
- Reiter, R.J.; Sainz, R.M.; Lopez-Burillo, S.; Mayo, J.C.; Manchester, L.C.; Tan, D.X. Melatonin ameliorates neurologic damage and neurophysiologic deficits in experimental models of stroke. Ann. N. Y. Acad. Sci. 2003, 993, 35–47. [Google Scholar] [CrossRef]
- Lee, E.J.; Wu, T.S.; Lee, M.Y.; Chen, T.Y.; Tsai, Y.Y.; Chuang, J.I.; Chang, G.L. Delayed treatment with melatonin enhances electrophysiological recovery following transient focal cerebral ischemia in rats. J. Pineal Res. 2004, 36, 33–42. [Google Scholar] [CrossRef]
- Bolognan, C.V.; Yamamoto, M.; Takei, N. Gial cell survival is enhanced during melatonin-induced neuroprotection against cerebral edema. FASEB J. 2000, 14, 1307–1317. [Google Scholar]
- Sinha, K.; Degaonkar, M.N.; Jagannathan, N.R.; Gupta, Y.K. Effect of melatonin on ischemia reperfusion injury induced by middle cerebral artery occlusion in rats. Eur. J. Pharmacol. 2001, 428, 185–192. [Google Scholar] [CrossRef]
- Torii, K.; Uneyama, H.; Nishino, H.; Kondoh, T. Melatonin suppresses cerebral edema caused by middle cerebral artery occlusion/reperfusion in rats assessed by magnetic resonance imaging. J. Pineal Res. 2004, 36, 18–24. [Google Scholar] [CrossRef]
- Pei, Z.; Cheung, R.T.F. Pretreatment with melatonin exerts anti-inflammatory effects against ischemia/reperfusion injury in a rat middle cerebral artery occlusion stroke model. J. Pineal Res. 2004, 37, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.-Y.; Kuan, Y.-H.; Chen, H.-Y.; Chen, T.-Y.; Chen, S.-T.; Huang, C.-C.; Yang, I.-P.; Hsu, Y.-S.; Wu, T.-S.; Lee, E.-J. Intravenous administration of melatonin reduces the intracerebral cellular inflammatory response following transient focal cerebral ischemia in rats. J. Pineal Res. 2007, 42, 297–309. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.J.; Lee, M.Y.; Chen, H.Y. Melatonin attenuates gray and white matter damage in a mouse model of transient focal cerebral ischemia. J. Pineal Res. 2005, 38, 42–52. [Google Scholar] [CrossRef] [PubMed]
- Kaptanoglu, E.; Palaoglu, S.; Demirpence, E.; Akbıyık, F.; Solaroglu, I.; Kılınc, A. Different responsiveness of central nervous system tissues to oxidative conditions and to the antioxidant effect of melatonin. J. Pineal Res. 2003, 34, 32–35. [Google Scholar] [CrossRef]
- Chen, T.-Y.; Lee, M.-Y.; Chen, H.-Y.; Kuo, Y.-L.; Lin, S.-C.; Wu, T.-S.; Lee, E.-J. Melatonin attenuates the postischemic increase in blood-brain barrier permeability and decreases hemorrhagic transformation of tissue-plasminogen activator therapy following ischemic stroke in mice. J. Pineal Res. 2006, 40, 242–250. [Google Scholar] [CrossRef]
- Pei, Z.; Pang, S.F.; Cheung, R.T.F. Administration of Melatonin After Onset of Ischemia Reduces the Volume of Cerebral Infarction in a Rat Middle Cerebral Artery Occlusion Stroke Model. Stroke 2003, 34, 770–775. [Google Scholar] [CrossRef] [PubMed]
- Koh, P.-O. Melatonin Attenuates the Cerebral Ischemic Injury via the MEK/ERK/p90RSK/Bad Signaling Cascade. J. Veter. Med. Sci. 2008, 70, 1219–1223. [Google Scholar] [CrossRef]
- Maldonado, M.D.; Murillo-Cabezas, F.; Terron, M.P.; Flores, L.J.; Tan, D.X.; Manchester, L.C.; Reiter, R.J. The potential of melatonin in reducing morbidity–mortality after craniocerebral trauma. J. Pineal Res. 2007, 42, 1–11. [Google Scholar] [CrossRef]
- Tan, D.; Manchester, L.C.; Terron, M.P.; Flores, L.J.; Reiter, R.J. One molecule, many derivatives: A never-ending interaction of melatonin with reactive oxygen and nitrogen species? J. Pineal Res. 2007, 42, 28–42. [Google Scholar] [CrossRef]
- Allegra, M.; Reiter, R.; Tan, D.; Gentile, C.; Tesoriere, L.; Livrea, M. The chemistry of melatonin’s interaction with reactive species. J. Pineal Res. 2003, 34, 1–10. [Google Scholar] [CrossRef]
- Rodriguez, C.; Mayo, J.C.; Sainz, R.M.; Antolín, I.; Herrera, F.; Martín, V.; Reiter, R.J. Regulation of antioxidant enzymes: A significant role for melatonin. J. Pineal Res. 2004, 36, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Tomás-Zapico, C.; Coto-Montes, A. A proposed mechanism to explain the stimulatory effect of melatonin on antioxidative enzymes. J. Pineal Res. 2005, 39, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.W.; Chen, T.Y.; Hung, C.Y.; Tai, S.H.; Huang, S.Y.; Chang, C.C.; Hung, H.Y.; Lee, E.J. Melatonin protects brain against ischemia/reperfusion injury by attenuating endoplasmic reticulum stress. Int. J. Mol. Med. 2018, 42, 182–192. [Google Scholar] [CrossRef] [PubMed]
- Szczepanik, M. Melatonin and its influence on immune system. J. Physiol. Pharmacol. 2007, 58 (Suppl. S6), 115–124. [Google Scholar] [PubMed]
- Schiaveto-De-Souza, A.; Da-Silva, C.; Defino, H.; Bel, E. Effect of melatonin on the functional recovery from experimental traumatic compression of the spinal cord. Braz. J. Med. Biol. Res. 2013, 46, 348–358. [Google Scholar] [CrossRef]
- Toklu, H.; Deniz, M.; Yüksel, M.; Keyer-Uysal, M.; Şener, G. The protective effect of melatonin and amlodipine against cerebral ischemia/reperfusion-induced oxidative brain injury in rats. Marmara Med. J. 2009, 22, 034–044. [Google Scholar]
- Cuzzocrea, S.; Mazzon, E.; Costantino, G. Beneficial effects of n-acetylcysteine on ischaemic brain injury. Br. J. Pharmacol. 2000, 130, 1219–1226. [Google Scholar] [CrossRef]
- Dean, O.; Giorlando, F.; Berk, M. N-acetylcysteine in psychiatry: Current therapeutic evidence and potential mechanisms of action. J. Psychiatry Neurosci. 2011, 36, 78–86. [Google Scholar] [CrossRef]
- Neuwelt, E.A.; Pagel, M.A.; Hasler, B.P.; Deloughery, T.G.; Muldoon, L.L. Therapeutic efficacy of aortic administration of N-acetylcysteine as a chemoprotectant against bone marrow toxicity after intracarotid administration of alkylators, with or without glutathione depletion in a rat model. Cancer Res. 2001, 61, 7868–7874. [Google Scholar]
- Farr, S.A.; Poon, H.F.; Dogrukol-Ak, D.; Drake, J.; Banks, W.A.; Eyerman, E.; Butterfield, D.A.; Morley, J.E. The antioxidants α-lipoic acid and N-acetylcysteine reverse memory impairment and brain oxidative stress in aged SAMP8 mice. J. Neurochem. 2003, 84, 1173–1183. [Google Scholar] [CrossRef]
- Hicdonmez, T.; Kanter, M.; Tiryaki, M.; Parsak, T.; Cobanoglu, S. Neuroprotective Effects of N-acetylcysteine on Experimental Closed Head Trauma in Rats. Neurochem. Res. 2006, 31, 473–481. [Google Scholar] [CrossRef] [PubMed]
- Banaclocha, M. Therapeutic potential of N-acetylcysteine in age-related mitochondrial neurodegenerative diseases. Med. Hypotheses 2001, 56, 472–477. [Google Scholar] [CrossRef] [PubMed]
- Shen, W.H.; Zhang, C.Y.; Zhang, G.Y. Antioxidants attenuate reperfusion injury after global brain ischemia through inhibiting nuclear factor-kappa B activity in rats. Acta Pharmacol. Sin. 2003, 24, 1125–1130. [Google Scholar]
- Harrison, P.M.; Wendon, J.A.; Gimson, A.E.; Alexander, G.J.; Williams, R. Improvement by Acetylcysteine of Hemodynamics and Oxygen Transport in Fulminant Hepatic Failure. N. Engl. J. Med. 1991, 324, 1852–1857. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.; Sekhon, B.; Jatana, M.; Giri, S.; Gilg, A.G.; Sekhon, C.; Singh, I.; Singh, A.K. Administration of N-acetylcysteine after focal cerebral ischemia protects brain and reduces inflammation in a rat model of experimental stroke. J. Neurosci. Res. 2004, 76, 519–527. [Google Scholar] [CrossRef]
- Turkmen, S.; Gonenc, O.C.; Karaca, Y.; Mentese, A.; Demir, S.; Beyhun, E.; Sahin, A.; Gunduz, A.; Yulug, E.; Turedi, S. The effect of ethyl pyruvate and N-acetylcysteine on ischemia-reperfusion injury in an experimental model of ischemic stroke. Am. J. Emerg. Med. 2016, 34, 1804–1807. [Google Scholar] [CrossRef]
- Danduga, R.C.S.R.; Dondapati, S.R.; Kola, P.K.; Kavati, S.S.H.; Singapalli, M.S. Combination effect of Aspirin and N-acetylcysteine against global cerebral ischemic reperfusion injury in rats. Neurol. Psychiatry Brain Res. 2019, 33, 101–111. [Google Scholar] [CrossRef]
- Liu, Y.; Liu, W.-C.; Sun, Y.; Shen, X.; Wang, X.; Shu, H.; Pan, R.; Liu, C.-F.; Liu, W.; Liu, K.J. Normobaric hyperoxia extends neuro-and vaso-protection of N-acetylcysteine in transient focal ischemia. Mol. Neurobiol. 2017, 54, 3418–3427. [Google Scholar] [CrossRef]
- Shafiei, E.; Bahtoei, M.; Raj, P.; Ostovar, A.; Iranpour, D.; Akbarzadeh, S.; Shahryari, H.; Anvaripour, A.; Tahmasebi, R.; Netticadan, T.; et al. Effects of N-acetyl cysteine and melatonin on early reperfusion injury in patients undergoing coronary artery bypass grafting: A randomized, open-labeled, placebo-controlled trial. Medicine 2018, 97, e11383. [Google Scholar] [CrossRef]
- Sener, G.; Tosun, O.; Kaçmaz, A.; Arbak, S.; Ersoy, Y.; Ayanoğlu-Dülger, G. Melatonin and N-acetylcysteine have beneficial effects during hepatic ischemia and reperfusion. Life Sci. 2003, 72, 2707–2718. [Google Scholar] [CrossRef]
- Kekec, Z.; Seydaoglul, G.; Sever, H.; Ozturk, F. The effect of antioxidants (N-acetylcysteine and melatonin) on hypoxia due to carbonmonoxide poisoning. Bratisl. Lek. Listy 2010, 111, 189–193. [Google Scholar] [PubMed]
- Wang, X.; Romero, R.; Mallard, C.; Arvidsson, P.; Gustavsson, M.; Hagberg, H. Melatonin and N-acetylcysteine reduce brain injury in response to lipopolysaccharide-sensitized hypoxia-ischemia. Am. J. Obstet. Gynecol. 2005, 193, S28. [Google Scholar] [CrossRef]
- Jauch, E.C.; Saver, J.L.; Adams, H.P., Jr.; Bruno, A.; Connors, J.J.; Demaerschalk, B.M.; Khatri, P.; McMullan, P.W., Jr.; Qureshi, A.I.; Rosenfield, K.; et al. Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013, 44, 870–947. [Google Scholar] [CrossRef] [PubMed]
- Al Kury, L.T.; Zeb, A.; Abidin, Z.U.; Irshad, N.; Malik, I.; Alvi, A.M.; Khalil, A.A.K.; Ahmad, S.; Faheem, M.; Khan, A.U.; et al. Neuroprotective effects of melatonin and celecoxib against ethanol-induced neurodegeneration: A computational and pharmacological approach. Drug Des. Dev. Ther. 2019, 13, 2715–2727. [Google Scholar] [CrossRef] [PubMed]
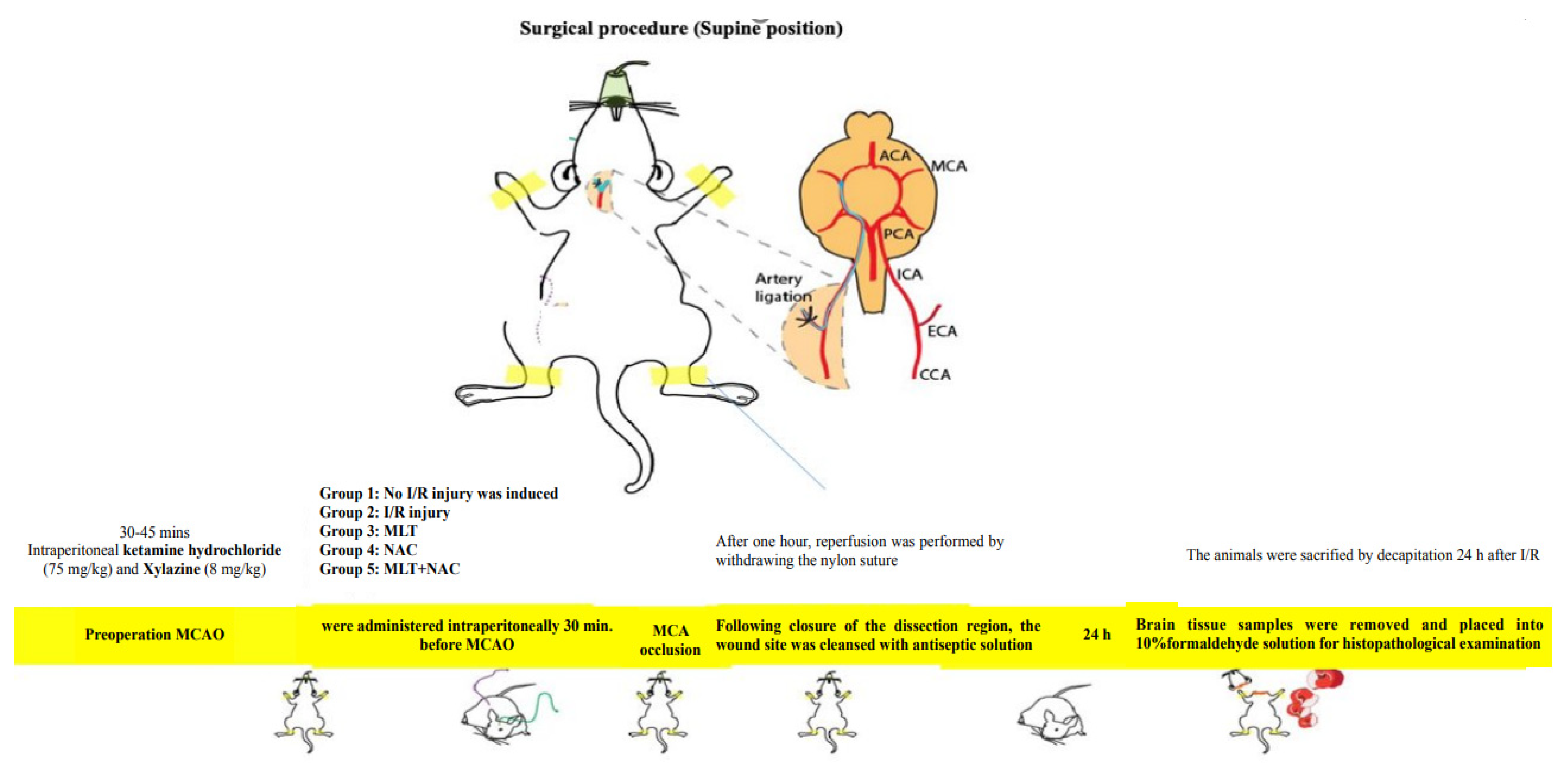
| Group | Name | Surgical Procedure | Medical Procedure |
|---|---|---|---|
| 1 | Control (n = 8) | None | Vehicle (SF + ethanol) |
| 2 | MCAO (n = 8) | MCAO ----> Reperfusion | Vehicle (SF + ethanol) |
| 3 | Melatonin (n = 8) | MCAO ----> Reperfusion | Melatonin (15 mg/kg) |
| 4 | NAC (n = 8) | MCAO ----> Reperfusion | NAC (50 mg/kg) |
| 5 | Melatonin + NAC (n = 9) | MCAO ----> Reperfusion | Melatonin (15 mg/kg) + NAC (50 mg/kg) |
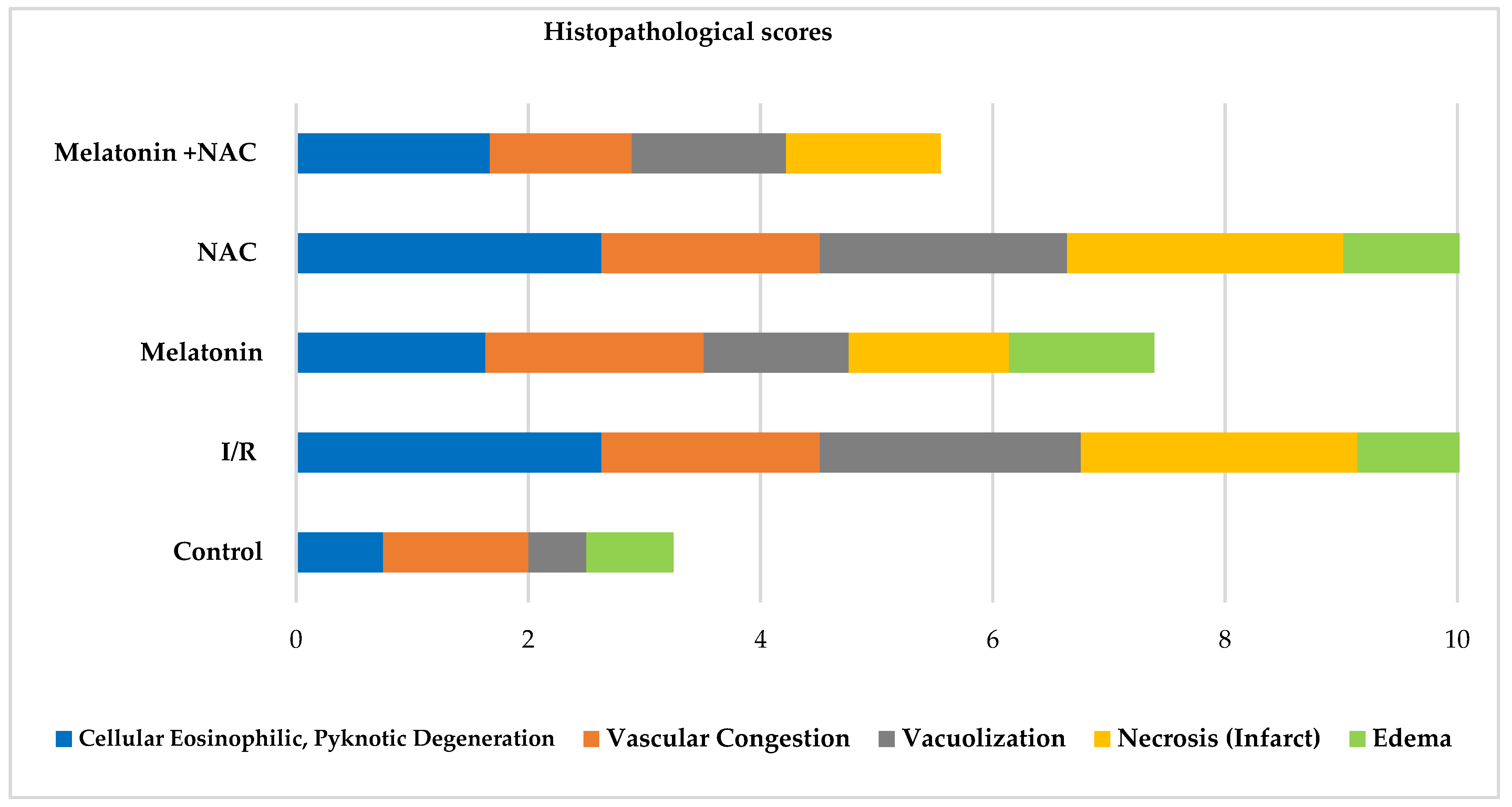
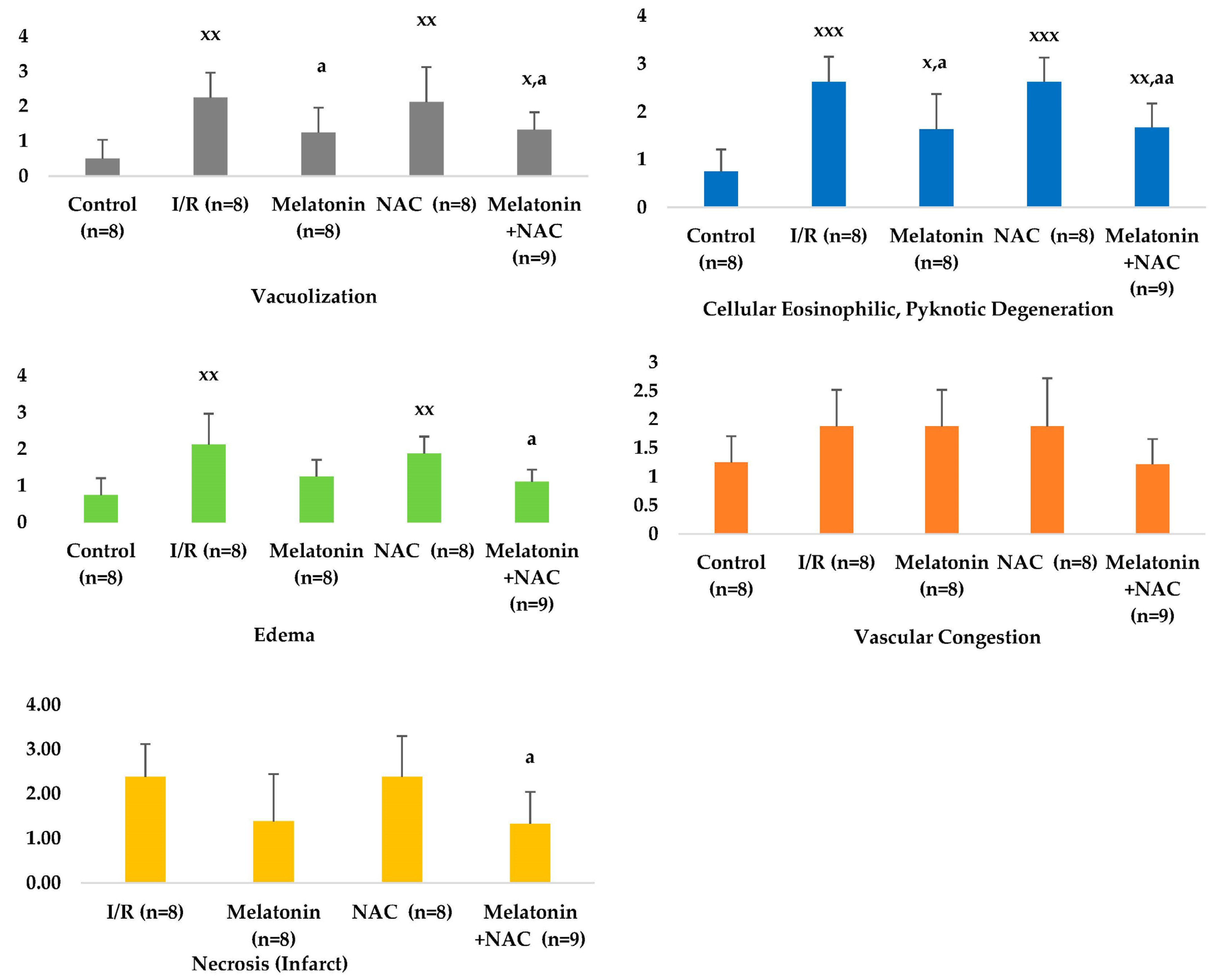
| Cellular Eosinophilic, Pyknotic Degeneration (Mean ± SD) | Vascular Congestion (Mean ± SD) | Vacuolization (Mean ± SD) | Necrosis (Infarct) (Mean ± SD) | Edema (Mean ± SD) | |
|---|---|---|---|---|---|
| Control (n = 8) | 0.75 ± 0.46 | 1.25 ± 0.46 | 0.50 ± 0.54 | 0.00 ± 0.00 | 0.75 ± 0.46 |
| I/R (n = 8) | 2.63 ± 0.52 | 1.88 ± 0.64 | 2.25 ± 0.71 | 2.38 ± 0.74 | 2.13 ± 0.84 |
| Melatonin (n = 8) | 1.63 ± 0.74 | 1.88 ± 0.64 | 1.25 ± 0.71 | 1.38 ± 1.06 | 1.25 ± 0.46 |
| NAC (n = 8) | 2.63 ± 0.502 | 1.88 ± 0.84 | 2.13 ± 0.99 | 2.38 ± 0.92 | 1.88 ± 0.64 |
| Melatonin +NAC (n = 9) | 1.67 ± 0.50 | 1.22 ± 0.44 | 1.33 ± 0.50 | 1.33 ± 0.71 | 1.11 ± 0.33 |
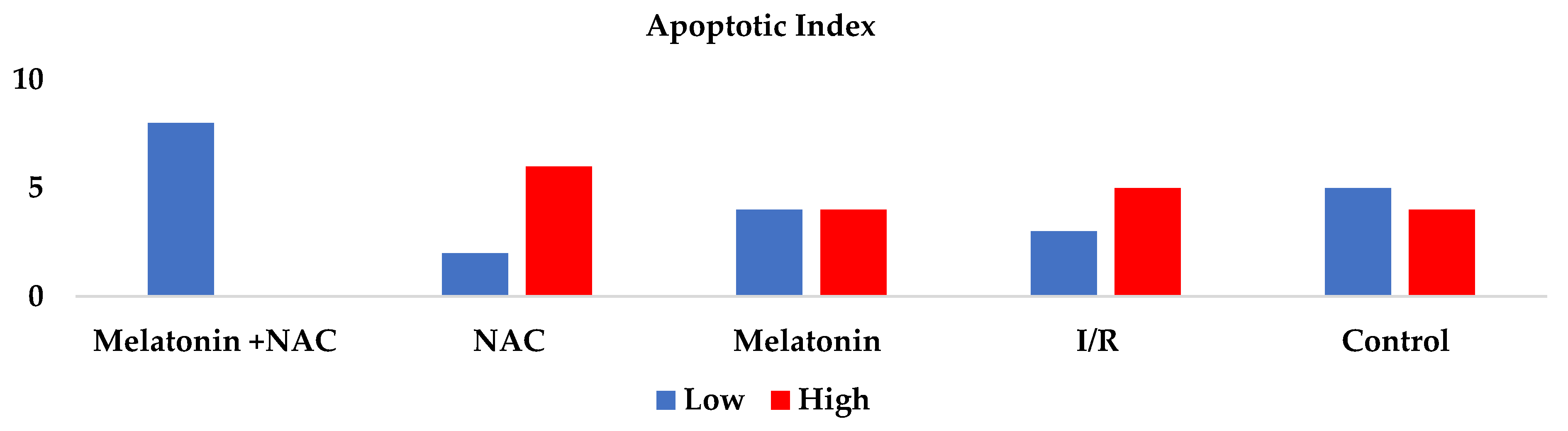
| Group | Apoptotic Index (TUNEL) Low/High (n) |
|---|---|
| Control (n = 8) | 8/0 |
| I/R (n = 8) | 2/6 |
| Melatonin (n = 8) | 4/4 |
| NAC (n = 8) | 3/5 |
| Melatonin + NAC (n = 9) | 5/4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aydin, H.; Bulmus, O.; Korkut, O.; Altun, E.; Ulusal, A.E. An Evaluation of the Effectiveness of Melatonin and n-Acetylcysteine in Cerebral Ischemia-Reperfusion Injury in Adult Rats. Medicina 2023, 59, 2026. https://doi.org/10.3390/medicina59112026
Aydin H, Bulmus O, Korkut O, Altun E, Ulusal AE. An Evaluation of the Effectiveness of Melatonin and n-Acetylcysteine in Cerebral Ischemia-Reperfusion Injury in Adult Rats. Medicina. 2023; 59(11):2026. https://doi.org/10.3390/medicina59112026
Chicago/Turabian StyleAydin, Hilal, Ozgur Bulmus, Oguzhan Korkut, Eren Altun, and Ali Engin Ulusal. 2023. "An Evaluation of the Effectiveness of Melatonin and n-Acetylcysteine in Cerebral Ischemia-Reperfusion Injury in Adult Rats" Medicina 59, no. 11: 2026. https://doi.org/10.3390/medicina59112026
APA StyleAydin, H., Bulmus, O., Korkut, O., Altun, E., & Ulusal, A. E. (2023). An Evaluation of the Effectiveness of Melatonin and n-Acetylcysteine in Cerebral Ischemia-Reperfusion Injury in Adult Rats. Medicina, 59(11), 2026. https://doi.org/10.3390/medicina59112026





