Abstract
Background and Objectives: Esophageal stenting with self-expandable metallic stents (SEMS), for both benign and malignant reasons, has been widely practiced for decades, but migration still remains the most common complication of the procedure. In this report we aim to review our experience and results in stent fixation with clips. Materials and Methods: We present 18 patients who underwent esophageal stenting for both benign and malignant reasons. The SEMSs used were partially covered and were fixated with two to four through the scope hemostatic clips in the proximal end of the prothesis. The procedure was performed only on patients with a high risk of migration of the stent. Results: Migration occurred in only one of the above-mentioned patients and was treated with stent repositioning. The other adverse events that occurred were related to tumor growth in patients with malignant diseases. Conclusions: Clip fixation of an esophageal self-expandable metallic stent in cases considered high-risk for migration is a safe procedure. It reduces the migration rate significantly for both benign and malignant indications.
1. Introduction
Placement of a self-expandable metallic stent (SEMS) in both benign and malignant strictures of the esophagus has been widely practiced for decades [1]. According to the European Society of Gastrointestinal Endoscopy’s (ESGE) latest guideline on stenting in the upper gastrointestinal tract, SEMSs are considered first line treatment for patients with malignant obstructions and short-term life expectancy or in combination with brachytherapy for longer life expectancy. Moreover, metallic stents have a pivotal role in the management of benign strictures, perforations and fistulas of the esophagus [2]. Stent migration remains the most common complication of the procedure. Benign reasons for stenting, including perforations, fistulas and strictures, have a higher risk of migration (30–62%) [1,3]. Patients with malignant disease at high risk of migration are those who are undergoing brachytherapy, as well as patients with distal strictures close to the gastroesophageal junction [1,4].
In this study, we review our experience and results in esophageal stenting and using through-the-scope hemostatic clips.
2. Materials and Methods
In the period from July 2018 to July 2023, in our tertiary medical center in Plovdiv, Bulgaria, we placed over 70 SEMSs in cases with both benign and malignant conditions. Due to the complication of migration, in the year of 2020, our team started fixating the proximal edge of the stent with through-the-scope hemostatic clips in the cases with higher risk for migration.
We present a total of 18 patients—12 male and 6 female, aged 41 to 84, that have undergone the procedure of SEMS placement with clips fixation, due to different reasons, shown in Table 1. Overall, out of the 18 cases, 13 had malignant obstruction due to adenocarcinoma of the cardia and/or distal esophagus [7], esophageal squamous cell carcinoma [1] and obstruction caused by mediastinal lymph nodes or progression of lung cancer [3]. The other five patients had benign reasons for stenting: perforations [2], benign strictures [2] and one broncho-esophageal fistula. Written consent was obtained from all patients prior to the procedure. All of the patients with malignant disease have been previously diagnosed and histologically verified.

Table 1.
Patients’ data.
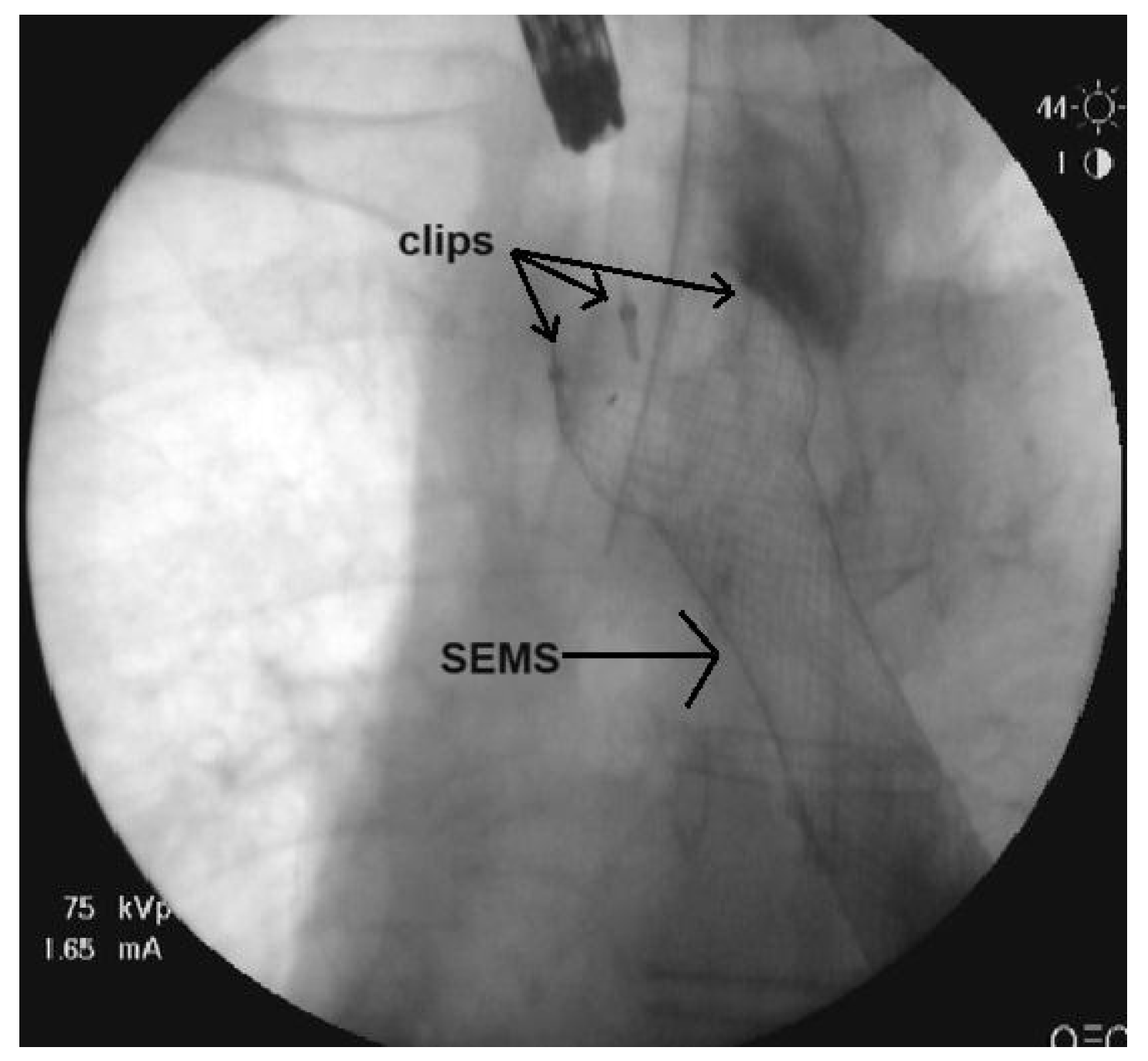
Our team used Partially Covered Esophageal Stents (Changzhou City Zhiye Medical Devices Institute, Changzhou, China and Wallflex, Boston Scientific, Boston, MA, USA) (Figure 1), which are both distal opening stents. A scarification test for Urografin sensibility took place prior to the manipulation. The procedure was performed under general anesthesia. The location and length of the stenosis was determined with endoscopy prior to the stenting. A submucosal injection of a solution of Urografin was placed 1 to 2 cm above the proximal end of the stricture and was used as a marker for the position of the SEMS. The stent was positioned over a guidewire and deployed under fluoroscopy guidance and its position and the efficiency of the procedure were verified through endoscopy. The SEMS was fixed in its proximal end using 2 to 4 EZ through-the-scope clips (Olympus) (Figure 2). The stent fixation was performed under endoscopic guidance and the clips were positioned either on two opposite sides or in the resemblance of the Mercedes sign. We used two clips in nine cases, three clips in eight cases and four clips in only one case.

Figure 1.
Partially covered self-expandable stent (Changzhou City Zhiye Medical Devices Institute, China).
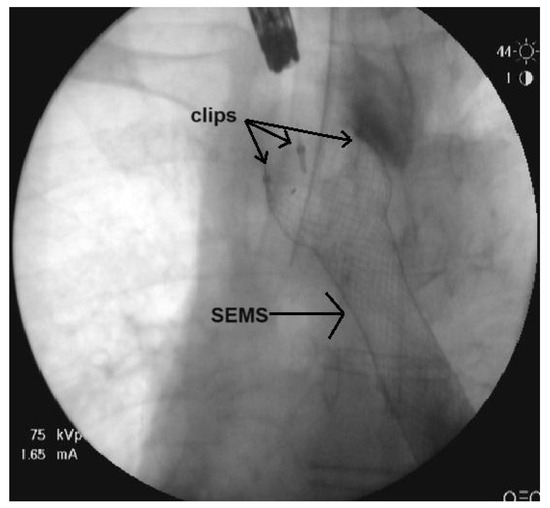
Figure 2.
Fluoroscopy film of the SEMS fixated with clips.
The length of the stent was chosen in correlation with the length of the stenosis. The stents we used were 20 mm in diameter and either 100 mm in length (Changzhou City Zhiye Medical Devices Institute, China) or 12 mm in length (Wallflex, Boston Scientific, MA, USA). The SEMS needed to be at least four centimeters longer than the obstruction. The following day, radiography with peroral contrast was performed to verify the correct position of the stent. The number of the clips depended on the reason for stenting. Typically, malignant obstruction with a higher grade of stricture is at lower risk of migration, so in those cases we placed a lesser number of clips (2 clips). In cases with benign reasons for stenting or malignant obstruction that is not that prominent, we placed a higher number of clips.
3. Results
In the malignant portion of the cases, three complications were reported. Only one of them was proximal migration of the prothesis noted in a patient with cardiac cancer and esophageal obstruction two weeks after the procedure. The migration resulted in repositioning of the SEMS. The other two complications were associated with tumor growth. In one of the patients with lung cancer and esophageal obstruction, tumor growth through the SEMS was noted. In the other case, tumor growth had spread higher than the proximal end of the stent and a second SEMS was placed overlying the first one. The follow-up period for the malignant cases was three months. No other short or long-term complications associated with the SEMS or the clip fixation were reported.
In the benign section of the research, no migrations or other complications were reported. The follow-up period for those cases was one year. The metallic stents were removed in a period from two weeks to two months, depending on the reason for stenting. There were no complications associated with the removal of the SEMS.
4. Discussion
The complications of esophageal stenting are divided into two groups—early and late complications. The early ones include pain, perforation, bleeding and technical failure in the deployment of the stent, whilst the late ones include migration of the stent, tissue ingrowth/overgrowth and clinical complications (recurrent dysphagia, gastrointestinal reflux, etc.) [5,6]. Migration is the most common complication after stent placement, ranging from 4–38% [4,7,8]. Typically, the fully covered SEMSs are more prone to migration than the partially covered and the non-covered ones [4]. The covering of the fully covered stents prevents embedding of the stent into the esophageal wall, which leaves them more prone to migration. Different kinds of anti-migration features were developed, ranging from means of outer fixation to shouldered ends, double-layer design, and endoscopic suturing and fixation [9]. In a study including 61 patients with both benign and malignant diseases, esophageal stents were externally fixated using a silk tread. No migrations occurred in this study, but external fixation adds additional discomfort for the patients [10]. A systematic review of six studies, consisting of 250 patients with malignant obstruction treated with double-layered SEMSs, showed 4.7% of migrations [11]. Endoscopic suturing and over-the-scope clip rates of migration were compared to those of non-fixated fully covered SEMSs. The results of this study show 32% risk of migration with endoscopic suturing and 12% risk with the over-the-scope clips, compared to 55% in the cases without fixation [12].
In the occasion that the stent is placed distally of the gastroesophageal junction or there is a lack of a stenosis in the esophagus (perforation, fistula), there is a higher risk of migration of the SEMS [13]. Even though methods of stent fixation significantly reduce the incidence of migration in these situations, a comparative study of 44 patients suggests that there is still a 13% risk of migration of the prothesis after clip fixation [14]. In our study, only one of eighteen procedures resulted in stent migration (5.5%), which shows even better results than the above-mentioned study [14].
5. Conclusions
Clip fixation of an esophageal self-expandable metallic stent in cases considered high-risk for migration is a safe procedure. It reduces the migration rate significantly for both benign and malignant indications. Further research with a greater number of cases and comparison between the different kinds of anti-migration measures must be performed.
Author Contributions
Conceptualization, N.B. and V.A.; methodology, L.K.; software, N.S.; validation, K.S. and K.M.; formal analysis, N.S.; investigation, L.K.; resources, K.S.; data curation, K.M.; writing—original draft preparation, K.S.; writing—review and editing, V.A.; visualization, N.B.; supervision, N.B.; project administration, L.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Hindy, P.; Hong, J.; Lam-Tsai, Y.; Gress, F. A comprehensive review of esophageal stents. Gastroenterol. Hepatol. N. Y. 2012, 8, 526–534. [Google Scholar] [PubMed]
- Spaander, M.C.; Baron, T.H.; Siersema, P.D.; Fuccio, L.; Schumacher, B.; Escorsell, À.; Garcia-Pagán, J.C.; Dumonceau, J.M.; Conio, M.; de Ceglie, A.; et al. Esophageal stenting for benign and malignant disease: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 2016, 48, 939–948. [Google Scholar] [CrossRef] [PubMed]
- Dua, K.S.; Vleggaar, F.P.; Santharam, R.; Siersema, P.D. Removable self-expanding plastic esophageal stent as a continuous, non-permanent dilator in treating refractory benign esophageal strictures: A prospective two-center study. Am. J. Gastroenterol. 2008, 103, 2988–2994. [Google Scholar] [CrossRef] [PubMed]
- Martins, B.C.; Retes, F.A.; Medrado, B.F.; de Lima, M.S.; Pennacchi, C.M.; Kawaguti, F.S.; Safatle-Ribeiro, A.V.; Uemura, R.S.; Maluf-Filho, F. Endoscopic management and prevention of migrated esophageal stents. World J. Gastrointest. Endosc. 2014, 6, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Saligram, S.; Lim, D.; Pena, L.; Friedman, M.; Harris, C.; Klapman, J. Safety and feasibility of esophageal self- expandable metal stent placement without the aid of fluoroscopy. Dis. Esophagus 2017, 30, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, F.C.; Dennert, B.; Zierer, S.T.; Sanowski, R.A. Esophageal self-expandable metallic stents--indications, practice, techniques, and complications: Results of a national survey. Gastrointest. Endosc. 1997, 45, 360–364. [Google Scholar] [CrossRef] [PubMed]
- Seven, G.; Irani, S.; Ross, A.S.; Gan, S.I.; Gluck, M.; Low, D.; Kozarek, R.A. Partially versus fully covered self-expanding metal stents for benign and malignant esophageal conditions: A single center experience. Surg. Endosc. 2013, 27, 2185–2192. [Google Scholar] [CrossRef] [PubMed]
- Thomas, S.; Siddiqui, A.A.; Taylor, L.J.; Parbhu, S.; Cao, C.; Loren, D.; Kowalski, T.; Adler, D.G. Fully-covered esophageal stent migration rates in benign and malignant disease: A multicenter retrospective study. Endosc. Int. Open 2019, 7, E751–E756. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.Y.; Tsauo, J.; Song, H.Y.; Kim, P.H.; Park, J.H. Self-Expandable Metallic Stent Placement for the Palliation of Esophageal Cancer. J. Korean Med. Sci. 2017, 32, 1062–1071. [Google Scholar] [CrossRef] [PubMed]
- Shim, C.S.; Cho, Y.D.; Moon, J.H.; Kim, J.O.; Cho, J.Y.; Kim, Y.S.; Lee, J.S.; Lee, M.S. Fixation of a modified covered esophageal stent: Its clinical usefulness for preventing stent migration. Endoscopy 2001, 33, 843–848. [Google Scholar] [CrossRef] [PubMed]
- Hussain, Z.; Diamantopoulos, A.; Krokidis, M.; Katsanos, K. Double-layered covered stent for the treatment of malignant oesophageal obstructions: Systematic review and meta-analysis. World J. Gastroenterol. 2016, 22, 7841–7850. [Google Scholar] [CrossRef] [PubMed]
- Shao, X.D.; Qi, X.S.; Guo, X.Z. Esophageal Stent for Refractory Variceal Bleeding: A Systemic Review and Meta-Analysis. BioMed Res. Int. 2016, 2016, 4054513. [Google Scholar] [CrossRef] [PubMed]
- Park, K.H.; Lew, D.; Samaan, J.; Patel, S.; Liu, Q.; Gaddam, S.; Gupta, K.; Jamil, L.H.; Lo, S.K. Comparison of no stent fixation, endoscopic suturing, and a novel over-the-scope clip for stent fixation in preventing migration of fully covered self-expanding metal stents: A retrospective comparative study (with video). Gastrointest. Endosc. 2022, 96, 771–779. [Google Scholar] [CrossRef] [PubMed]
- Vanbiervliet, G.; Filippi, J.; Karimdjee, B.S.; Venissac, N.; Iannelli, A.; Rahili, A.; Benizri, E.; Pop, D.; Staccini, P.; Tran, A.; et al. The role of clips in preventing migration of fully covered metallic esophageal stents: A pilot comparative study. Surg. Endosc. 2012, 26, 53–59. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).