Immediate Effects of Sprinter-Pattern Exercise on the Lordotic Curve and Abdominal Muscle Activity in Individuals with Hyperlordosis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants and Ethics
2.2.1. Inclusion Criteria
- Adults aged 20–50 years;
- Chronic back pain for more than 3 months;
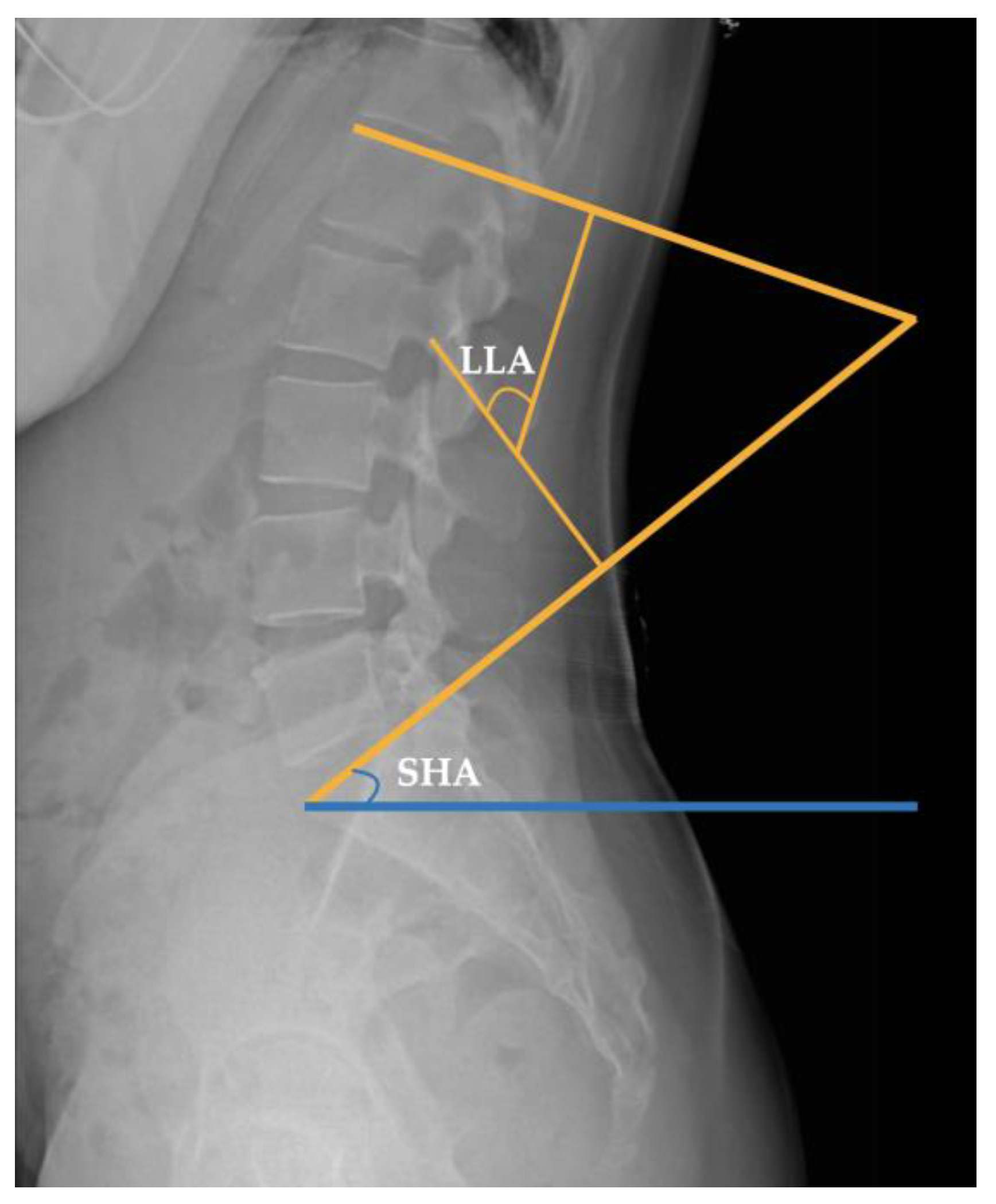
- Lumbar lordotic angle (LLA) > 50°;
- Sacrohorizontal angle (SHA) > 40°.
2.2.2. Exclusion Criteria
- Orthopedic malformations or neurosurgical diseases;
- Disc degeneration or other conditions that may affect the interpretation of results (severe fibromyalgia and rheumatoid arthritis, in combination with other treatments);
- Surgery or pregnancy within 30 d;
- Breastfeeding;
- Wearing a hyperlordosis treatment device;
- Participation in similar studies.
2.3. Sample Size
2.4. Randomization and Blinding
2.5. Intervention
2.5.1. Sprinter-Pattern Exercise
2.5.2. Crunch Exercise
2.6. Outcomes
2.6.1. Lordotic Curve
- Lumbar Lordotic Angle
- 2.
- Sacrohorizontal Angle
2.6.2. Abdominal Muscle Activity
2.7. Data Analysis
3. Results
3.1. General Characteristics
3.2. Changes in the Lumbar Lordotic Angle by Exercise Method
3.3. Changes in Sacrohorizontal Angle by Exercise Method
3.4. Changes in Muscle Activity by Exercise Method
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lee, J.; Moon, S.; So, Y. Effects of the Lumbar Stabilization Exercise on Scoliosis, Local Muscle Area, VAS and Muscle Function in Female University Students. Exerc. Sci. 2011, 20, 61–70. [Google Scholar]
- Fatemi, R.; Javid, M.; Najafabadi, E.M. Effects of William Training on Lumbosacral Muscles Function, Lumbar Curve and Pain. J. Back. Musculoskelet. Rehabil. 2015, 28, 591–597. [Google Scholar] [CrossRef]
- Kendall, F.P.; McCreary, E.K.; Provance, P.G.; Rodgers, M.M.; Romani, W.A. Muscles: Testing and Function with Posture and Pain; Lippincott Williams & Wilkins: Baltimore, MD, USA, 2005; Volume 5. [Google Scholar]
- Muscolino, J.E. Kinesiology-E-Book: The Skeletal System and Muscle Function; Elsevier Health Sciences: Philadelphia, PA, USA, 2014. [Google Scholar]
- Neumann, D.A. Kinesiology of the Musculoskeletal System-e-Book: Foundations for Rehabilitation; Elsevier Health Sciences: Philadelphia, PA, USA, 2016. [Google Scholar]
- Rone-Adams, S.A.; Shamus, E.; Hileman, M. Physical Therapists’ Evaluation of the Trunk Flexors in Patients with Low Back Pain. Internet J. Allied Health Sci. Pr. 2004, 2, 3. [Google Scholar] [CrossRef]
- Workman, J.C.; Docherty, D.; Parfrey, K.C.; Behm, D.G. Influence of Pelvis Position on the Activation of Abdominal and Hip Flexor Muscles. J. Strength. Cond. Res. 2008, 22, 1563–1569. [Google Scholar] [CrossRef] [PubMed]
- Rodacki, C.L.N.; Rodacki, A.L.F.; Ugrinowitsch, C.; Zielinski, D.; da Costa, R.B. Spinal Unloading after Abdominal Exercises. Clin. Biomech. 2008, 23, 8–14. [Google Scholar] [CrossRef]
- Shin, M.G. The Effect of Abdominal Muscle Contraction on Center of Gravity Moving and Lumbar Lordosis: In Low Back Pain Patients with Pelvic Anterior Shift; Kyonggi University: Suwon, Republic of Korea, 2010. [Google Scholar]
- Rahmani, N.; Mohseni-Bandpei, M.A.; Salavati, M.; Vameghi, R.; Abdollahi, I. Comparative Study of Abdominal Muscle Thickness on Ultrasonography in Healthy Adolescents and Patients with Low Back Pain. J. Ultrasound Med. 2018, 37, 905–912. [Google Scholar] [CrossRef]
- Childs, J.D.; Teyhen, D.S.; Casey, P.R.; McCoy-Singh, K.A.; Feldtmann, A.W.; Wright, A.C.; Dugan, J.L.; Wu, S.S.; George, S.Z. Effects of Traditional Sit-Up Training versus Core Stabilization Exercises on Short-Term Musculoskeletal Injuries in US Army Soldiers: A Cluster Randomized trial. Phys. Ther. 2010, 90, 1404–1412. [Google Scholar] [CrossRef]
- McGill, S. Core Training: Evidence Translating to Better Performance and Injury Prevention. Strength. Cond. J. 2010, 32, 33–46. [Google Scholar] [CrossRef]
- Kim, S.-Y.; Kang, M.-H.; Kim, E.-R.; Jung, I.-G.; Seo, E.-Y.; Oh, J.-S. Comparison of EMG Activity on Abdominal Muscles during Plank Exercise with Unilateral and Bilateral Additional Isometric Hip Adduction. J. Electromyogr. Kinesiol. 2016, 30, 9–14. [Google Scholar] [CrossRef]
- Dietz, B. Let’s Sprint, Let’s Skate; Springer Science & Business Media: Berlin, Germany, 2009. [Google Scholar]
- Lee, H.J.; Kim, S.Y. Comparison of the Effects of Abdominal Draw-in and Expansion Maneuvers on Trunk Stabilization in Patients with Low Back Pain and Lumbar Spine Instability. Phys. Ther. Korea 2015, 22, 37–48. [Google Scholar] [CrossRef]
- França, F.R.; Burke, T.N.; Caffaro, R.R.; Ramos, L.A.; Marques, A.P. Effects of Muscular Stretching and Segmental Stabilization on Functional Disability and Pain in Patients with Chronic Low Back Pain: A Randomized, Controlled Trial. J. Manip. Physiol. Ther. 2012, 35, 279–285. [Google Scholar] [CrossRef]
- Grenier, S.G.; McGill, S.M. Quantification of Lumbar Stability by Using 2 Different Abdominal Activation Strategies. Arch. Phys. Med. Rehabil. 2007, 88, 54–62. [Google Scholar] [CrossRef] [PubMed]
- Shortz, S.K.; Haas, M. Relationship Between Radiographic Lumbosacral Spine Mensuration and Chronic Low Back Pain Intensity: A Cross-Sectional Study. J. Chiropr. Med. 2018, 17, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Javid, M.; Najafabadi, E.; Motlagh, K.; Fatemi, R. The Effects of 8 Weeks Corrective Training on Lumbar Angle and Flexibility of Lumbosacral Muscles in Females with Hyperlordosis; William’s Intervention. Int. J. Res. Stud. Biosci. 2014, 2, 116–125. [Google Scholar]
- Lee, W.-J.; Park, S.; Park, J.-W. Inf Luence of Trunk Stabilization Exercise upon the Lumbar Stabilization and Foot Pressure in Patients with Back Pain. J. Korean Phys. Ther. 2014, 26, 21–26. [Google Scholar]
- Shirazi, S.A.; Haghighi, F.M.; Alavi, S.M.; Nezhad, F.F.; Emami, F. Is Application of Kinesio Tape to Treat Hyperlordosis More Effective on Abdominal Muscles or Hamstrings? J. Res. Med. Sci. 2018, 23, 9. [Google Scholar] [CrossRef]
- Carvalho, C.; Caetano, J.M.; Cunha, L.; Rebouta, P.; Kaptchuk, T.J.; Kirsch, I. Open-Label Placebo Treatment in Chronic Low Back Pain: A Randomized Controlled Trial. Pain 2016, 157, 2766. [Google Scholar] [CrossRef]
- van Vugt, V.A.; van der Wouden, J.C.; Essery, R.; Yardley, L.; Twisk, J.W.R.; van der Horst, H.E.; Maarsingh, O.R. Internet Based Vestibular Rehabilitation with and without Physiotherapy Support for Adults Aged 50 and Older with a Chronic Vestibular Syndrome in General Practice: Three Armed Randomised Controlled Trial. BMJ 2019, 367, l5922. [Google Scholar] [CrossRef]
- Zhou, J.; Ning, X.; Fathallah, F. Differences in Lumbopelvic Rhythm between Trunk Flexion and Extension. Clin. Biomech. 2016, 32, 274–279. [Google Scholar] [CrossRef]
- Nelson, G.A.; Bent-Forsythe, D.A.; Roopchand-Martin, S.C. Electromyographic Activity of the Rectus Abdominis during a Traditional Crunch and the Basic Jackknife Exercise with the Ab Lounge™. J. Strength. Cond. Res. 2012, 26, 1584–1588. [Google Scholar] [CrossRef]
- Marks, M.; Stanford, C.; Newton, P. Which Lateral Radiographic Positioning Technique Provides the Most Reliable and Functional Representation of a Patient’s Sagittal Balance? Spine 2009, 34, 949–954. [Google Scholar] [CrossRef]
- Penha, P.J.; Casarotto, R.A.; Sacco, I.C.N.; Marques, A.P.; João, S.M.A. Qualitative Postural Analysis among Boys and Girls of Seven to Ten Years of Age. Braz. J. Phys. Ther. 2008, 12, 386–391. [Google Scholar] [CrossRef]
- Vrtovec, T.; Pernus, F.; Likar, B. A Review of Methods for Quantitative Evaluation of Spinal Curvature. Eur. Spine J. 2009, 18, 593–607. [Google Scholar] [CrossRef]
- Flint, J.; Linneman, T.; Pederson, R.; Storstad, M. EMG Analysis of Latissimus Dorsi, Erector Spinae and Middle Trapezius Muscle Activity during Spinal Rotation: A Pilot Study. Phys. Ther. Sch. Proj. 2015, 571. Available online: https://commons.und.edu/pt-grad/571 (accessed on 8 November 2023).
- Schuller, S.; Charles, Y.P.; Steib, J.P. Sagittal Spinopelvic Alignment and Body Mass Index in Patients with Degenerative Spondylolisthesis. Eur. Spine J. 2011, 20, 713–719. [Google Scholar] [CrossRef]
- Morvan, G.; Mathieu, P.; Vuillemin, V.; Guerini, H.; Bossard, P.; Zeitoun, F.; Wybier, M. Standardized Way for Imaging of the Sagittal Spinal Balance. Eur. Spine J. 2011, 20 (Suppl. 5), 602–608. [Google Scholar] [CrossRef]
- Rajnics, P.; Templier, A.; Skalli, W.; Lavaste, F.; Illés, T. The Association of Sagittal Spinal and Pelvic Parameters in Asymptomatic Persons and Patients with Isthmic Spondylolisthesis. J. Spinal Disord. Tech. 2002, 15, 24–30. [Google Scholar] [CrossRef]
- Evcik, D.; Yücel, A. Lumbar Lordosis in Acute and Chronic Low Back Pain Patients. Rheumatol. Int. 2003, 23, 163–165. [Google Scholar] [CrossRef]
- Criswell, E. Cram’s Introduction to Surface Electromyography; Jones & Bartlett Publishers: Sudbury, MA, USA, 2010. [Google Scholar]
- Dankaerts, W.; O’Sullivan, P.B.; Burnett, A.F.; Straker, L.M.; Danneels, L.A. Reliability of EMG Measurements for Trunk Muscles During Maximal and Sub-Maximal Voluntary Isometric Contractions in Healthy Controls and CLBP Patients. J. Electromyogr. Kinesiol. 2004, 14, 333–342. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Academic Press: New York, NY, USA, 2013. [Google Scholar]
- Olmedo-Buenrostro, B.A.; Trujillo-Hernández, B.; Pérez-Vargas, F.D.; Díaz-Giner, V.R.; Delgado-Enciso, I.; Muñiz-Murguía, J.; Huerta, M.; Trujillo, X.; Mora-Brambila, A.B.; Vásquez, C. Comparison of Three Therapeutic Exercises Protocols to Lumbar Hyperlordosis Improvement in Asyntomatic Youths. Rev. Investig. Clin. 2010, 62, 568–576. [Google Scholar]
- Arun, B.; Suganya, M.; Ashok, A. Myofascial Release Therapy in Addition to the Posterior Pelvic Tilting in Hyperlordosis Individuals. Indones. J. Health Sci. 2019, 3, 71–77. [Google Scholar]
- Jensen, K.K.; Kjaer, M.; Jorgensen, L.N. Abdominal Muscle Function and Incisional Hernia: A Systematic Review. Hernia 2014, 18, 481–486. [Google Scholar] [CrossRef]
- Nikita, A.; Richer, P. Quick Reference Evidence Based Muscle Manual; Professional Health System: Hong Kong, China, 2008. [Google Scholar]
- Been, E.; Kalichman, L. Lumbar lordosis. Spine J. 2014, 14, 87–97. [Google Scholar] [CrossRef]
- Drysdale, C.L.; Earl, J.E.; Hertel, J. Surface Electromyographic Activity of the Abdominal Muscles during Pelvic-Tilt and Abdominal-Hollowing Exercises. J. Athl. Train. 2004, 39, 32. [Google Scholar]
- Shields, R.K.; Heiss, D.G. An Electromyographic Comparison of Abdominal Muscle Synergies during Curl and Double Straight Leg Lowering Exercises with Control of the Pelvic Position. Spine 1997, 22, 1873–1879. [Google Scholar] [CrossRef]
- Urquhart, D.M.; Hodges, P.W.; Allen, T.J.; Story, I.H. Abdominal Muscle Recruitment during a Range of Voluntary Exercises. Man. Ther. 2005, 10, 144–153. [Google Scholar] [CrossRef]
- Contreras, B.; Schoenfeld, B. To Crunch or Not to Crunch: An Evidence-Based Examination of Spinal Flexion Exercises, Their Potential Risks, and Their Applicability to Program Design. Strength. Cond. J. 2011, 33, 8–18. [Google Scholar] [CrossRef]
- Souza, G.M.; Baker, L.L.; Powers, C.M. Electromyographic Activity of Selected Trunk Muscles during Dynamic Spine Stabilization Exercises. Arch. Phys. Med. Rehabil. 2001, 82, 1551–1557. [Google Scholar] [CrossRef]
- Escamilla, R.F.; Lewis, C.; Bell, D.; Bramblet, G.; Daffron, J.; Lambert, S.; Pecson, A.; Imamura, R.; Paulos, L.; Andrews, J.R. Core Muscle Activation During Swiss Ball and Traditional Abdominal Exercises. J. Orthop. Sports Phys. Ther. 2010, 40, 265–276. [Google Scholar] [CrossRef]
- Escamilla, R.F.; Babb, E.; DeWitt, R.; Jew, P.; Kelleher, P.; Burnham, T.; Busch, J.; D’Anna, K.; Mowbray, R.; Imamura, R.T. Electromyographic analysis of Traditional and Nontraditional Abdominal Exercises: Implications for Rehabilitation and Training. Phys. Ther. 2006, 86, 656–671. [Google Scholar] [CrossRef]
- Escamilla, R.F.; Lewis, C.; Pecson, A.; Imamura, R.; Andrews, J.R. Muscle Activation among Supine, Prone, and Side Position Exercises with and without a Swiss Ball. Sports Health 2016, 8, 372–379. [Google Scholar] [CrossRef]
- Aruin, A.S.; Latash, M.L. Directional Specificity of Postural Muscles in Feed-Forward Postural Reactions during Fast Voluntary Arm Movements. Exp. Brain Res. 1995, 103, 323–332. [Google Scholar] [CrossRef]
- Hodges, P.; Cresswell, A.; Thorstensson, A. Preparatory Trunk Motion Accompanies Rapid upper Limb Movement. Exp. Brain Res. 1999, 124, 69–79. [Google Scholar] [CrossRef]
- Lee, D.; Kang, M.; Kim, J.; Kim, Y.; Park, J.; Oh, J. Effects of Non-Paretic Arm Exercises Using a Tubing Band on Abdominal Muscle Activity in Stroke Patients. NeuroRehabilitation 2013, 33, 605–610. [Google Scholar] [CrossRef]
- Pereira, I.L.R.; Queiroz, B.; Loss, J.; Amorim, C.; Sacco, I.C.N. Trunk Muscle Emg During Intermediate Pilates Mat Exercises in Beginner Healthy and Chronic Low Back Pain Individuals. J. Manip. Physiol. Ther. 2017, 40, 350–357. [Google Scholar] [CrossRef]
- Meakin, J.R.; Fulford, J.; Seymour, R.; Welsman, J.R.; Knapp, K.M. The Relationship between Sagittal Curvature and Extensor Muscle Volume in the Lumbar Spine. J. Anat. 2013, 222, 608–614. [Google Scholar] [CrossRef]
- Richardson, C.; Toppenberg, R.; Jull, G. An Initial Evaluation of Eight Abdominal Exercises for Their Ability to Provide Stabilisation for the Lumbar Spine. Aust. J. Physiother. 1990, 36, 6–11. [Google Scholar] [CrossRef]
- Norris, C.M. Abdominal Muscle Training in Sport. Br. J. Sports Med. 1993, 27, 19–27. [Google Scholar] [CrossRef]
- Richardson, C.A.; Jull, G.A. Muscle Control–Pain Control. What Exercises Would You Prescribe? Manu. Ther. 1995, 1, 2–10. [Google Scholar] [CrossRef]
- McPherson, S.L.; Watson, T. Training of Transversus Abdominis Activation in the Supine Position with Ultrasound Biofeedback Translated to Increased Transversus Abdominis Activation during Upright Loaded Functional Tasks. PMR 2014, 6, 612–623. [Google Scholar] [CrossRef]



| Abdominal Muscles | Attachment Site |
|---|---|
| Rectus abdominis | A point approximately 2 cm lateral to and above the umbilicus, parallel to the muscle fibers. |
| External oblique | A point above the anterior superior iliac spine on the lateral surface of the rectus abdominis. |
| Internal oblique | The midpoint between the border of the inguinal ligament and outer corner of the rectus abdominis and the triangle formed by the anterior superior iliac spine and the umbilicus. |
| SPE (n = 20) | CE (n = 20) | p | |
|---|---|---|---|
| Sex (male/female) | 9/11 | 11/9 | 0.539 |
| Age (years) | 34.40 ± 7.18 | 34.25 ± 6.96 | 0.413 |
| Height (cm) | 168.80 ± 7.19 | 169.40 ± 7.37 | 0.625 |
| Weight (kg) | 61.35 ± 10.00 | 61.97 ± 9.11 | 0.839 |
| Body mass index (kg/m2) | 21.34 ± 1.75 | 21.32 ± 1.42 | 0.968 |
| Variables | SPE (n = 20) | CE (n = 20) | Between-Group Differences ‡ |
|---|---|---|---|
| Lumbar lordotic angle (°) | |||
| Baseline (A) | 56.24 ± 2.57 | 55.49 ± 3.11 | |
| Immediate (B) | 51.63 ± 2.21 | 53.25 ± 2.79 | −1.62 [−3.02, −0.22] † |
| Change from A to B | 4.62 ± 1.31 | 2.24 ± 1.18 | |
| Change from A to B ‡ | 1.876 [4.05, 5.19] *** | 0.739 [1.72, 2.76] *** | 1.851 [1.58, 3.18] *** |
| Sacrohorizontal angle (°) | |||
| Baseline (A) | 42.78 ± 1.50 | 41.98 ± 1.18 | |
| Immediate (B) | 39.48 ± 1.97 | 40.17 ± 1.42 | −0.69 [−1.68, 0.30] † |
| Change from A to B | 3.30 ± 1.60 | 1.81 ± 1.17 | |
| Change from A to B ‡ | 1.831 [2.60, 4.01] *** | 1.352 [1.30, 2.32] *** | 1.031 [0.59, 2.40] ** |
| Muscle activation (%) | |||
| Rectus abdominis | 155.90 ± 38.17 | 179.03 ± 49.71 | −23.12 [−48.47, 2.23] † |
| External oblique | 75.96 ± 21.00 | 62.90 ± 17.20 | 13.06 [1.44, 24.68] †,* |
| Internal oblique | 165.76 ± 46.96 | 132.08 ± 39.87 | 33.68 [4.34, 63.02] †,* |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.; Kim, H.; Jung, J.; Lee, S. Immediate Effects of Sprinter-Pattern Exercise on the Lordotic Curve and Abdominal Muscle Activity in Individuals with Hyperlordosis. Medicina 2023, 59, 2177. https://doi.org/10.3390/medicina59122177
Lee S, Kim H, Jung J, Lee S. Immediate Effects of Sprinter-Pattern Exercise on the Lordotic Curve and Abdominal Muscle Activity in Individuals with Hyperlordosis. Medicina. 2023; 59(12):2177. https://doi.org/10.3390/medicina59122177
Chicago/Turabian StyleLee, Sangbong, Hyunjoong Kim, Jihye Jung, and Seungwon Lee. 2023. "Immediate Effects of Sprinter-Pattern Exercise on the Lordotic Curve and Abdominal Muscle Activity in Individuals with Hyperlordosis" Medicina 59, no. 12: 2177. https://doi.org/10.3390/medicina59122177
APA StyleLee, S., Kim, H., Jung, J., & Lee, S. (2023). Immediate Effects of Sprinter-Pattern Exercise on the Lordotic Curve and Abdominal Muscle Activity in Individuals with Hyperlordosis. Medicina, 59(12), 2177. https://doi.org/10.3390/medicina59122177








