Foley Catheter as a Tourniquet for Peripartum Hemorrhage Prevention in Patients with Placenta Accreta Spectrum—A Two Case Report and a Review of the Literature
Abstract
1. Introduction
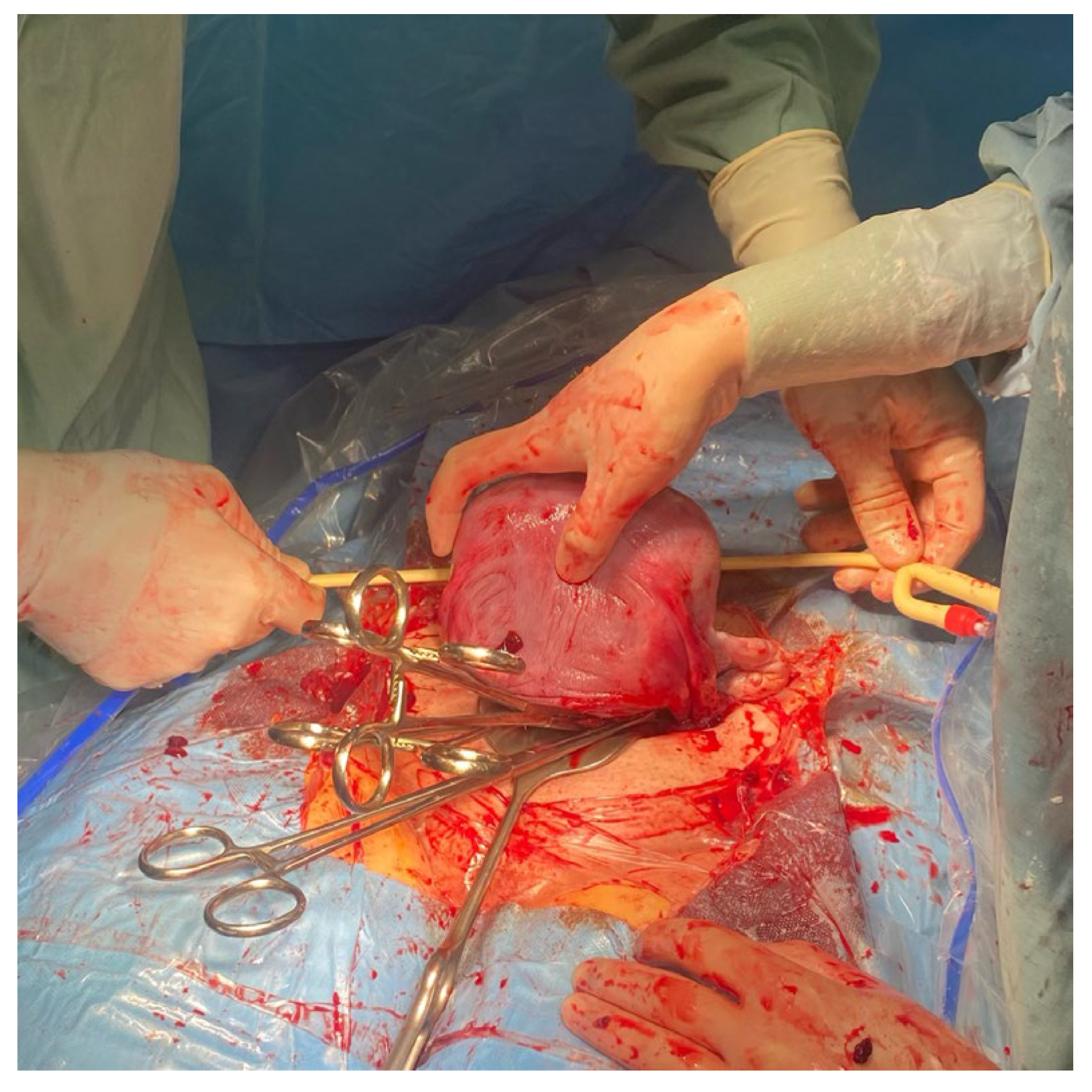
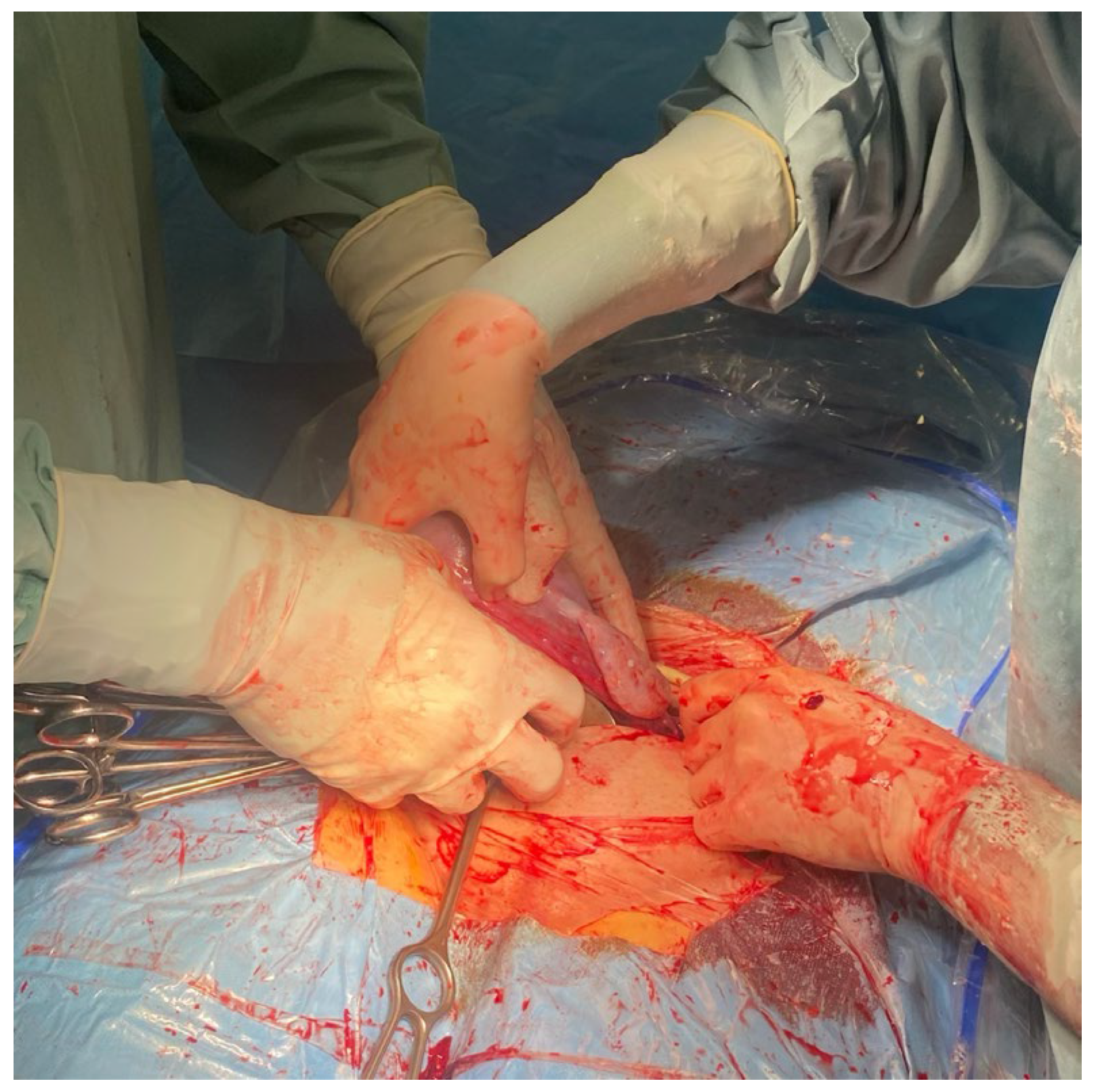
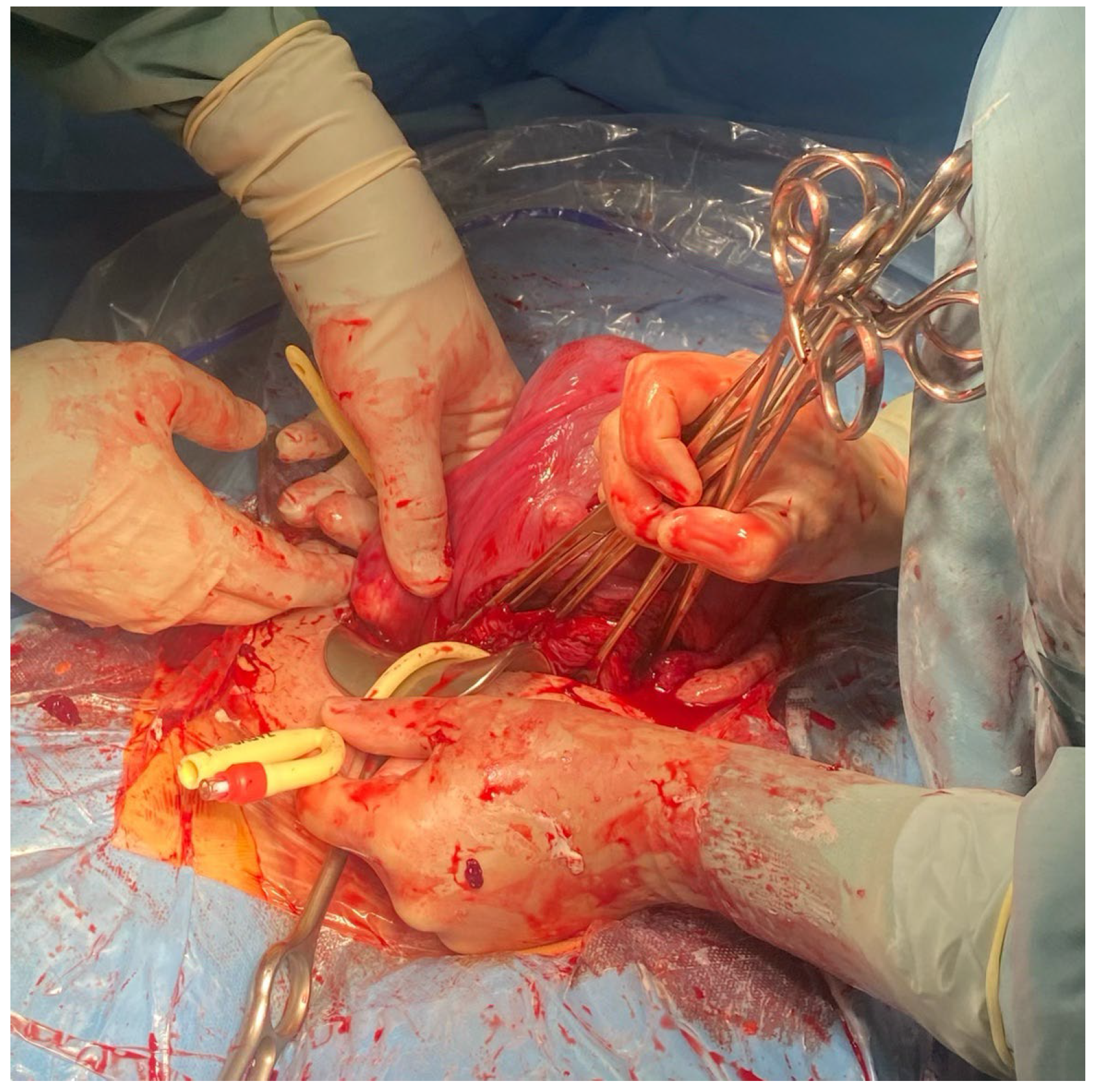
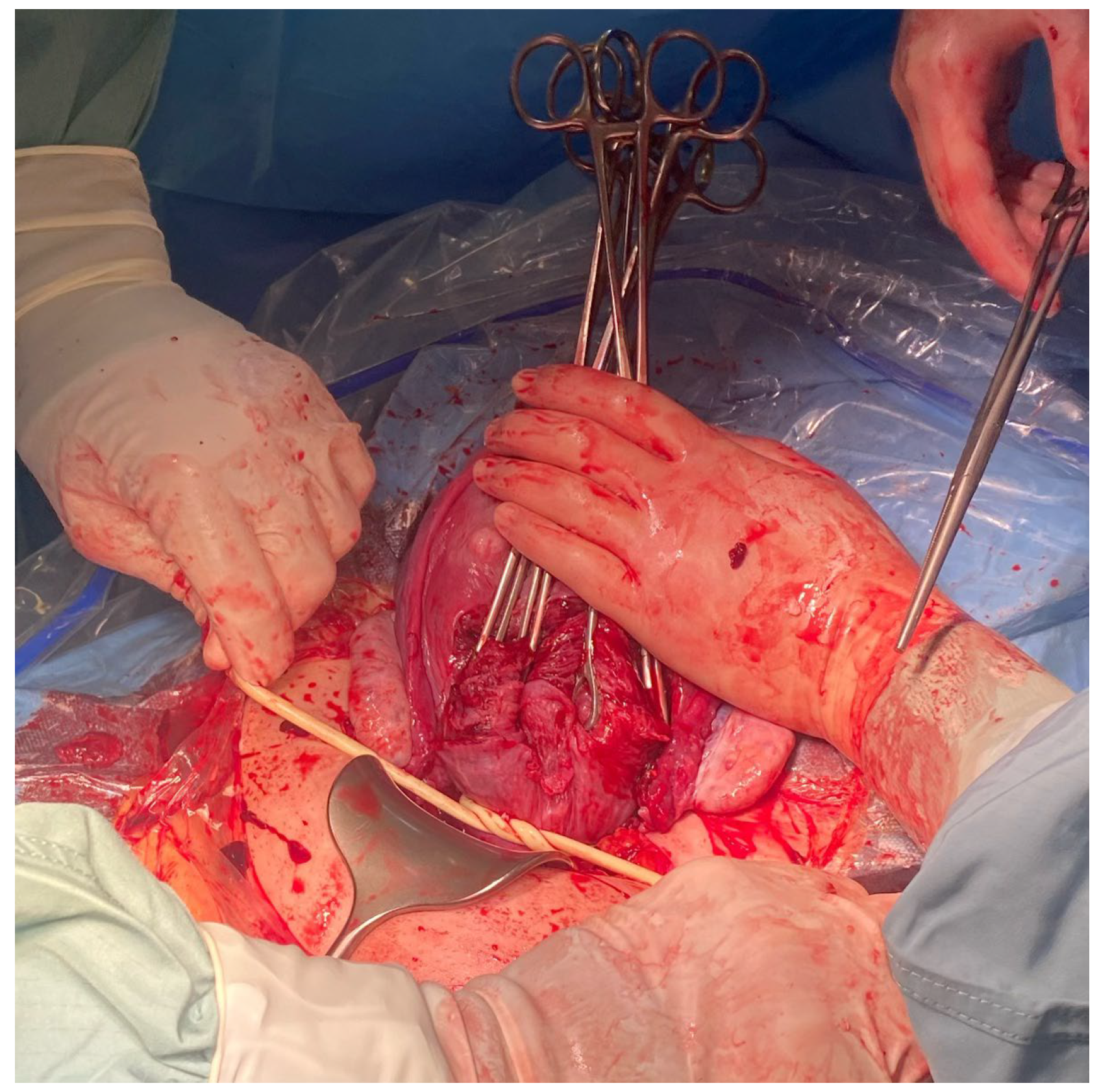
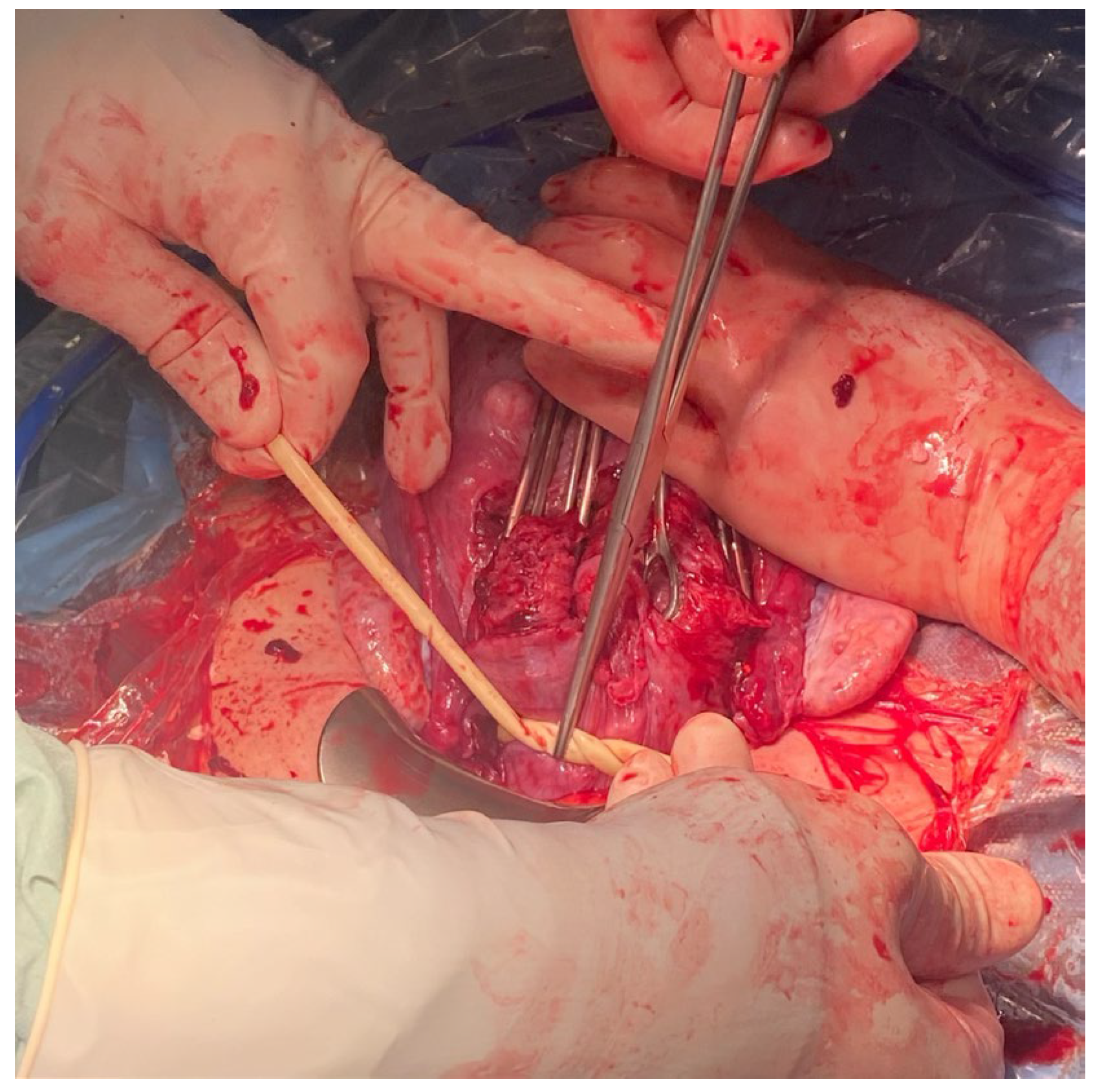
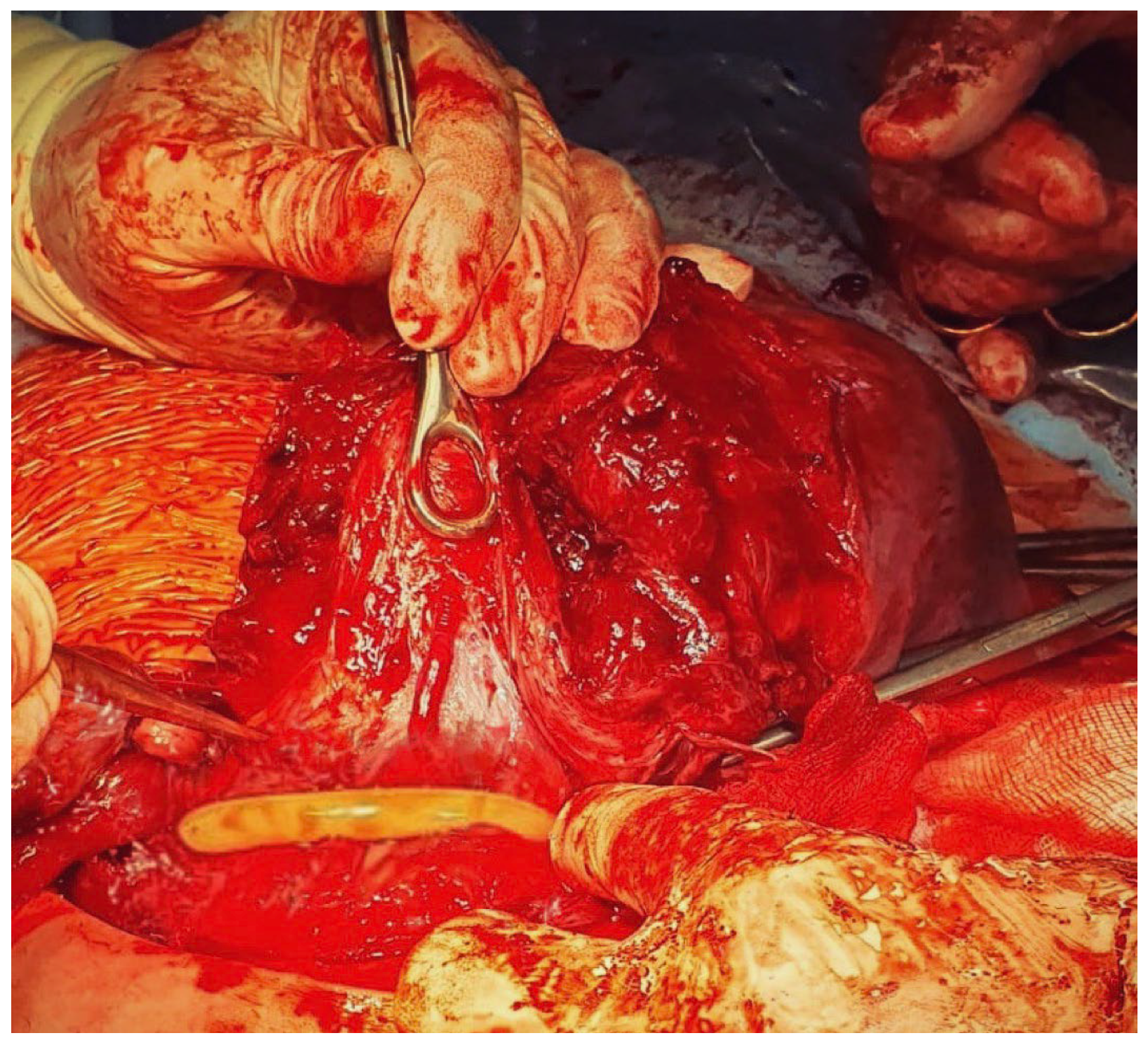
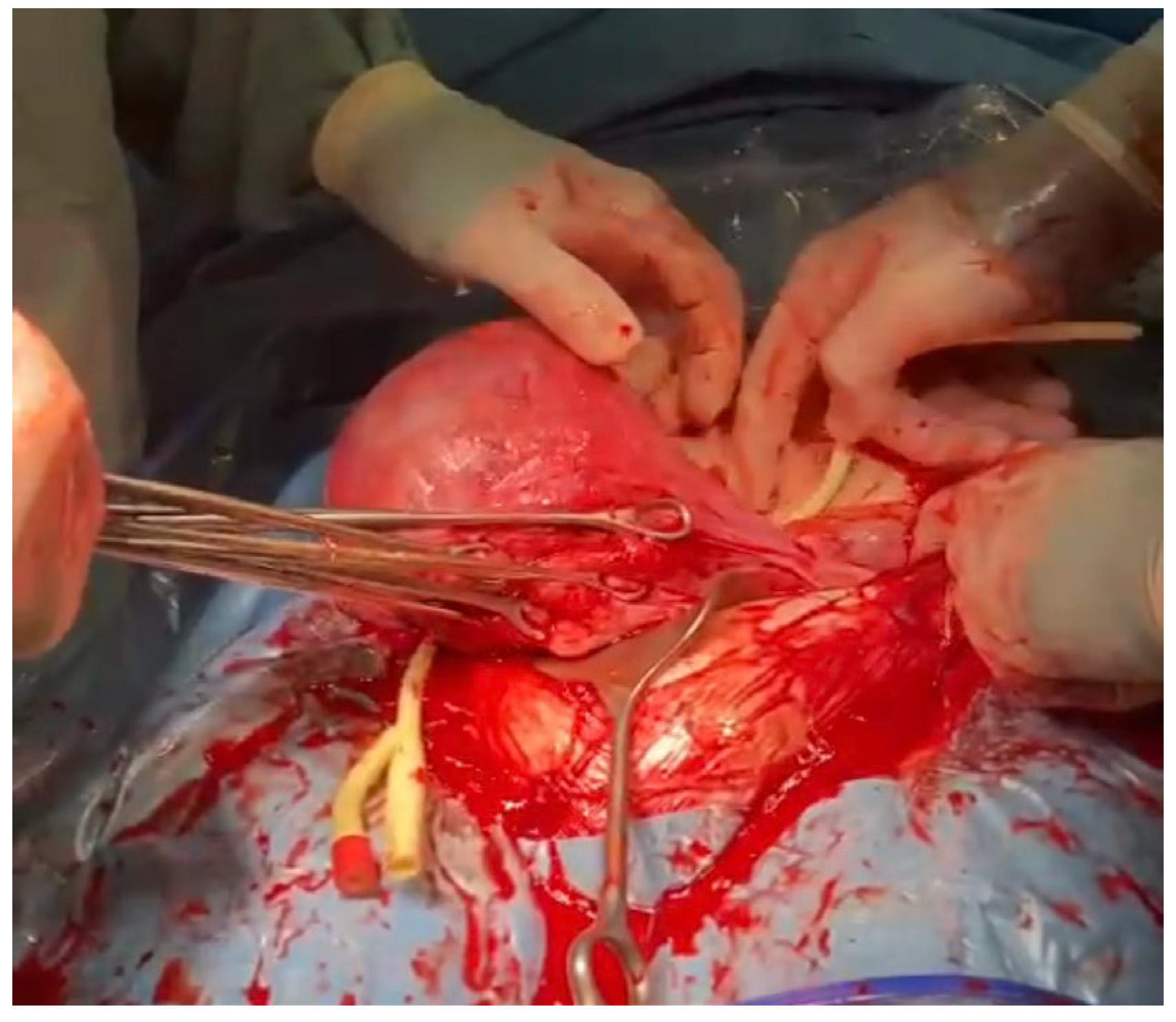
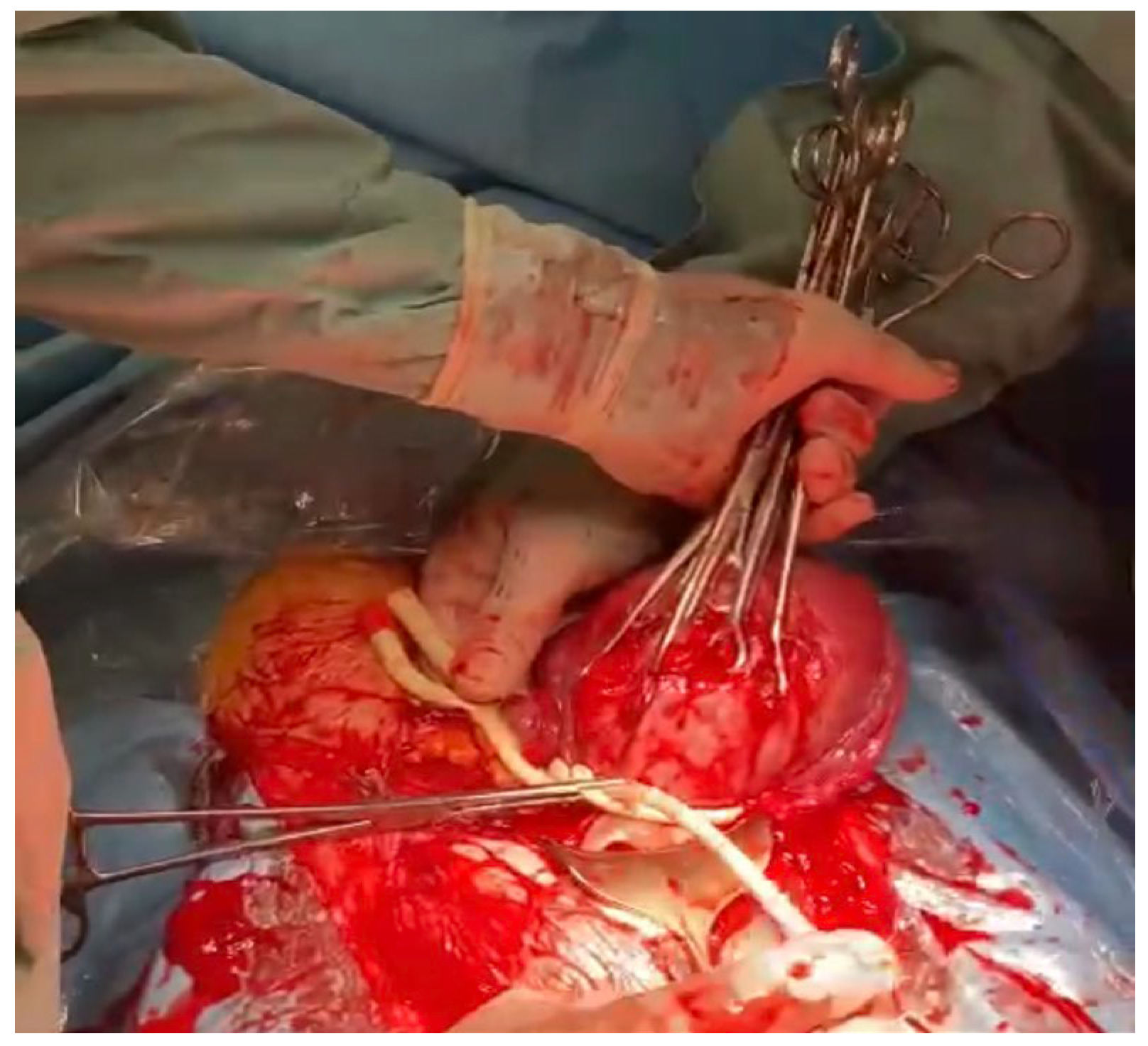
2. The Method
3. Case Reports
3.1. Patient 1
3.2. Patient 2
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
| DV | Ductus venosus |
| MRI | Magnetic resonance |
| PAS | Placenta Accreta Spectrum |
| UmA | Umbilical artery |
References
- Ikeda, T.; Sameshima, H.; Kawaguchi, H.; Yamauchi, N.; Ikenoue, T. Tourniquet technique prevents profuse blood loss in placenta accreta cesarean section. J. Obstet. Gynaecol. Res. 2005, 31, 27–31. [Google Scholar] [CrossRef]
- Envain, F.; Garabedian, C. Tourniquet: A simple intervention for hemorrhage during cesarean for placenta accreta. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 249, 110–112. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Zhang, X.; Liu, L.; Duan, S.; Pei, C.; Zhao, Y.; Liu, R.; Wang, W.; Jian, Y.; Liu, Y.; et al. Placenta Accreta Spectrum Outcomes Using Tourniquet and Forceps for Vascular Control. Front. Med. 2021, 8, 557678. [Google Scholar] [CrossRef] [PubMed]
- Meng, J.L.; Gong, W.Y.; Wang, S.; Ni, X.J.; Zuo, C.T.; Gu, Y.Z. Two-tourniquet sequential blocking as a simple intervention for hemorrhage during cesarean delivery for placenta previa accreta. Int. J. Gynaecol. Obstet. 2017, 138, 361–362. [Google Scholar] [CrossRef] [PubMed]
- Abdelaziz, A.T.; Ahmed, H.A.; Mohamed, Y.A.-R. A Novel Torniquet to reduce blood loss during surgical treatment of postpartum hemorrhage in cesarean section. Corpus ID: 212584557. J. Am. Sci. 2012, 8, 100–103. [Google Scholar]
- Altal, O.F.; Qudsieh, S.; Ben-Sadon, A.; Hatamleh, A.; Bataineh, A.; Halalsheh, O.; Amarin, Z. Cervical tourniquet during cesarean section to reduce bleeding in morbidly adherent placenta: A pilot study. Future Sci. OA 2022, 8, FSO789. [Google Scholar] [CrossRef] [PubMed]
- Oğlak, S.C.; Ölmez, F.; Tunç, Ş. Evaluation of Antepartum Factors for Predicting the Risk of Emergency Cesarean Delivery in Pregnancies Complicated With Placenta Previa. Ochsner. J. 2022, 22, 146–153. [Google Scholar] [CrossRef] [PubMed]
- Jauniaux, E.; Alfirevic, Z.; Bhide, A.G.; Belfort, M.A.; Burton, G.J.; Collins, S.L.; Dornan, S.; Jurkovic, D.; Kayem, G.; Kingdom, J.; et al. Placenta Praevia and Placenta Accreta: Diagnosis and Management: Green-top Guideline No. 27a. BJOG 2019, 126, e1–e48. [Google Scholar] [CrossRef] [PubMed]
- Jauniaux, E.; Collins, S.; Burton, G.J. Placenta accreta spectrum: Pathophysiology and evidence-based anatomy for prenatal ultrasound imaging. Am. J. Obstet. Gynecol. 2018, 218, 75–87. [Google Scholar] [CrossRef] [PubMed]
- Zimmer, M.; Sieroszewski, P.; Wielgoś, M.; Czajkowski, K.; Ropacka-Lesiak, M.; Huras, H.; Kalinka, J.; Paszkowski, T.; Oszukowski, P.; Cnota, W.; et al. Algorytm postępowania w przypadkach łożyska przodującego i/lub łożyska z nieprawidłową implantacją (PAS). Polskie Towarzystwo Ginekologów i Położników—2022, cz. I i II. Ginekol. Perinatol. Prakt. 2022, 7, 92–95. [Google Scholar]
- Kolås, T.; Øian, P.; Skjeldestad, F.E. Risks for peroperative excessive blood loss in cesarean delivery. Acta Obstet. Gynecol. Scand. 2010, 89, 658–663. [Google Scholar] [CrossRef] [PubMed]
- Buke, B.; Canverenler, E.; Akkaya, H.; Akercan, F. A Novel Atraumatic Tourniquet Technique for Excessive Bleeding during Cesarean Sections. Obstet. Gynecol. Int. 2017, 2017, 7171520. [Google Scholar] [CrossRef] [PubMed]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Staniczek, J.; Manasar-Dyrbuś, M.; Skowronek, K.; Winkowska, E.; Stojko, R. Foley Catheter as a Tourniquet for Peripartum Hemorrhage Prevention in Patients with Placenta Accreta Spectrum—A Two Case Report and a Review of the Literature. Medicina 2023, 59, 641. https://doi.org/10.3390/medicina59040641
Staniczek J, Manasar-Dyrbuś M, Skowronek K, Winkowska E, Stojko R. Foley Catheter as a Tourniquet for Peripartum Hemorrhage Prevention in Patients with Placenta Accreta Spectrum—A Two Case Report and a Review of the Literature. Medicina. 2023; 59(4):641. https://doi.org/10.3390/medicina59040641
Chicago/Turabian StyleStaniczek, Jakub, Maisa Manasar-Dyrbuś, Kaja Skowronek, Ewa Winkowska, and Rafał Stojko. 2023. "Foley Catheter as a Tourniquet for Peripartum Hemorrhage Prevention in Patients with Placenta Accreta Spectrum—A Two Case Report and a Review of the Literature" Medicina 59, no. 4: 641. https://doi.org/10.3390/medicina59040641
APA StyleStaniczek, J., Manasar-Dyrbuś, M., Skowronek, K., Winkowska, E., & Stojko, R. (2023). Foley Catheter as a Tourniquet for Peripartum Hemorrhage Prevention in Patients with Placenta Accreta Spectrum—A Two Case Report and a Review of the Literature. Medicina, 59(4), 641. https://doi.org/10.3390/medicina59040641






