Management of Pyometra Using a Novel Image-Guided Percutaneous Technique: A Case Report
Abstract
1. Introduction
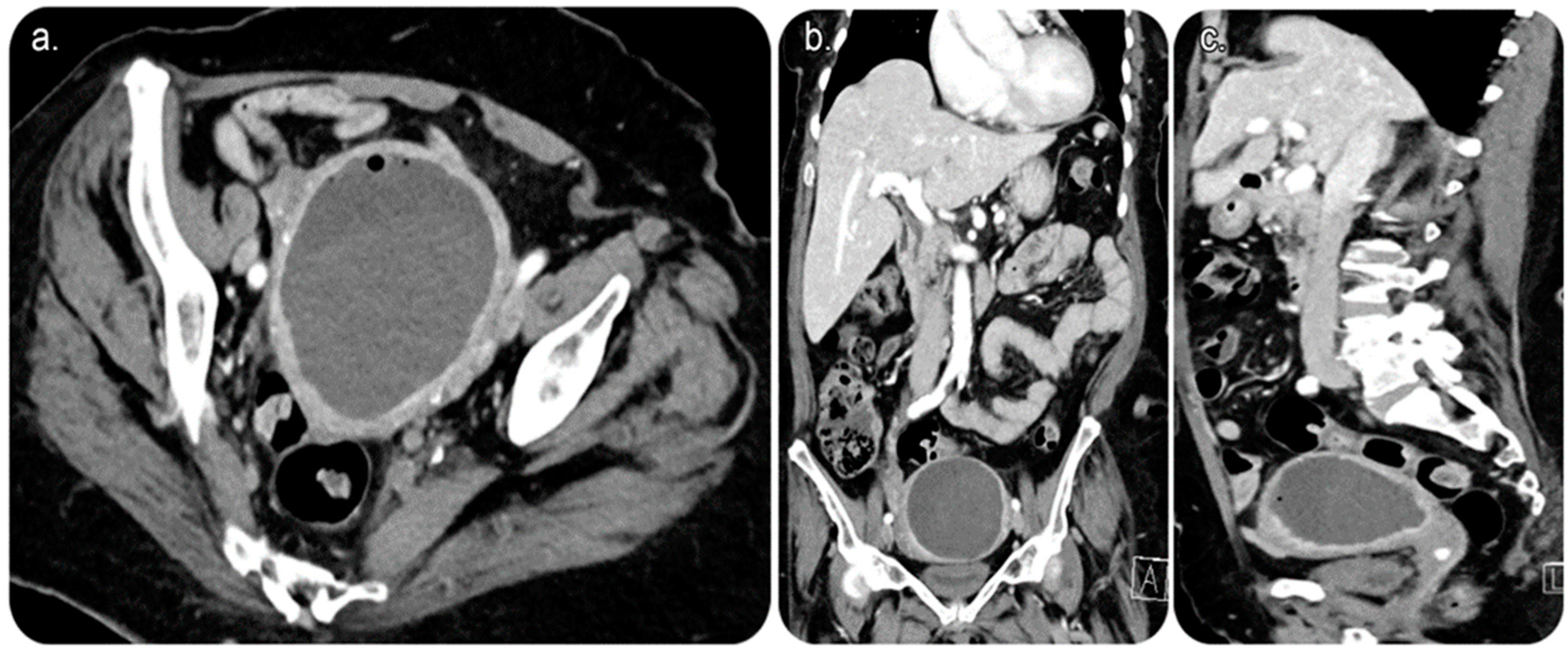
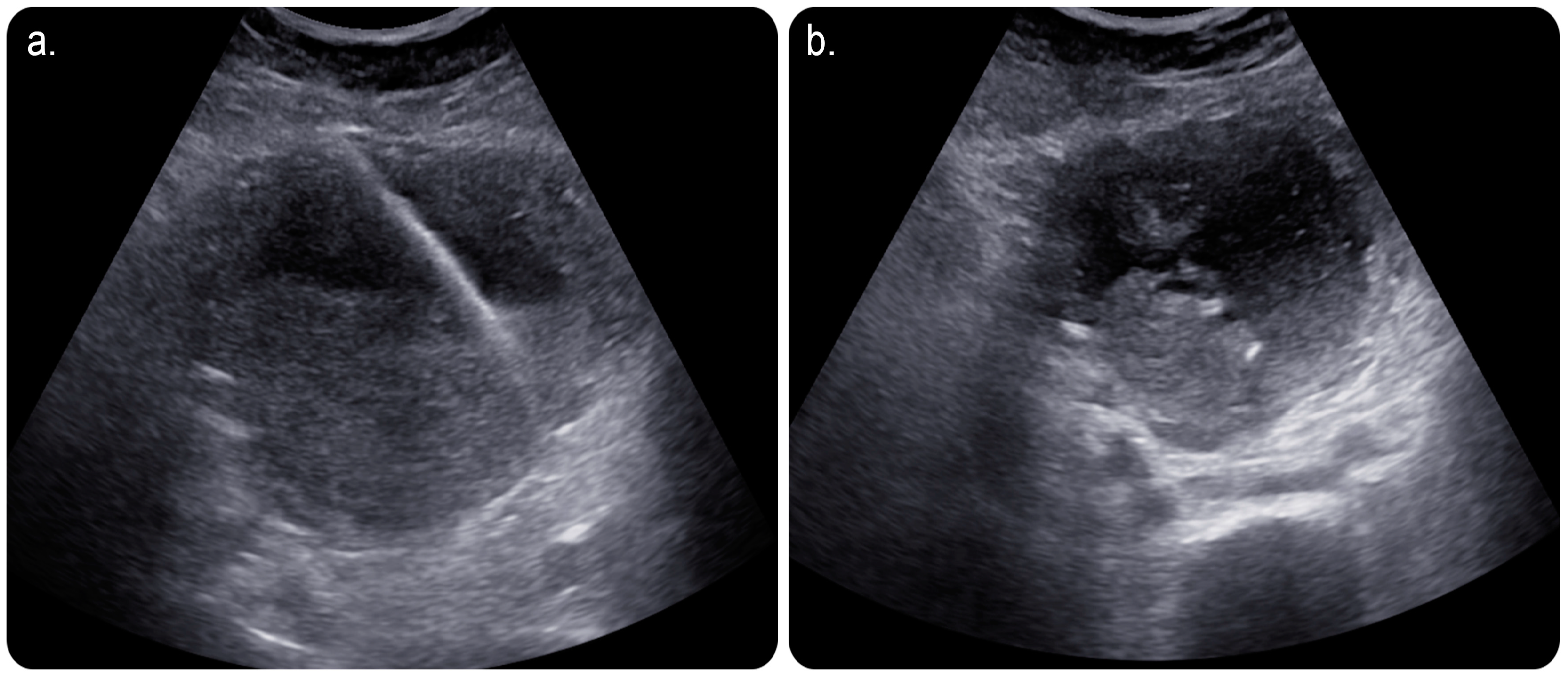
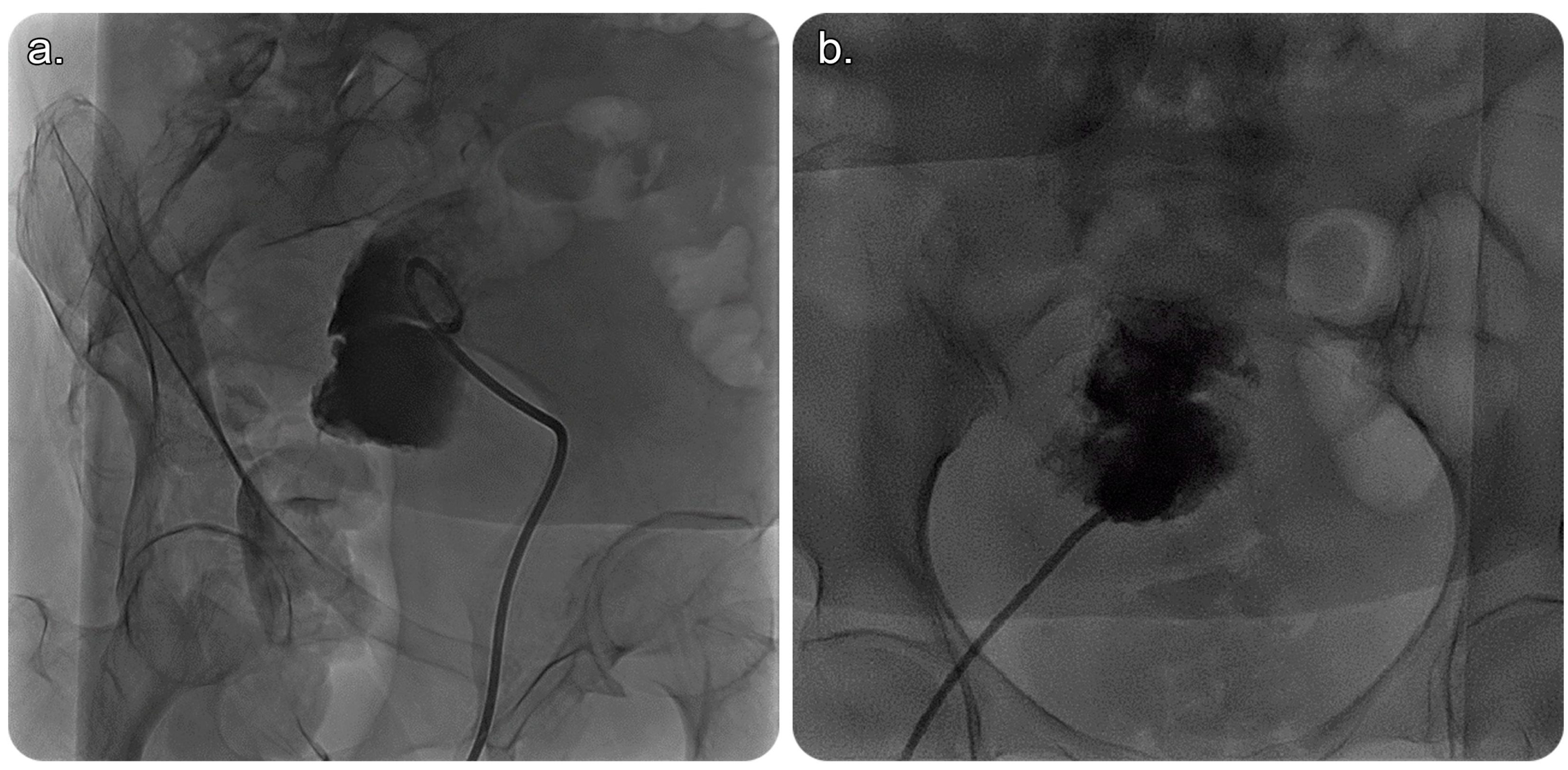
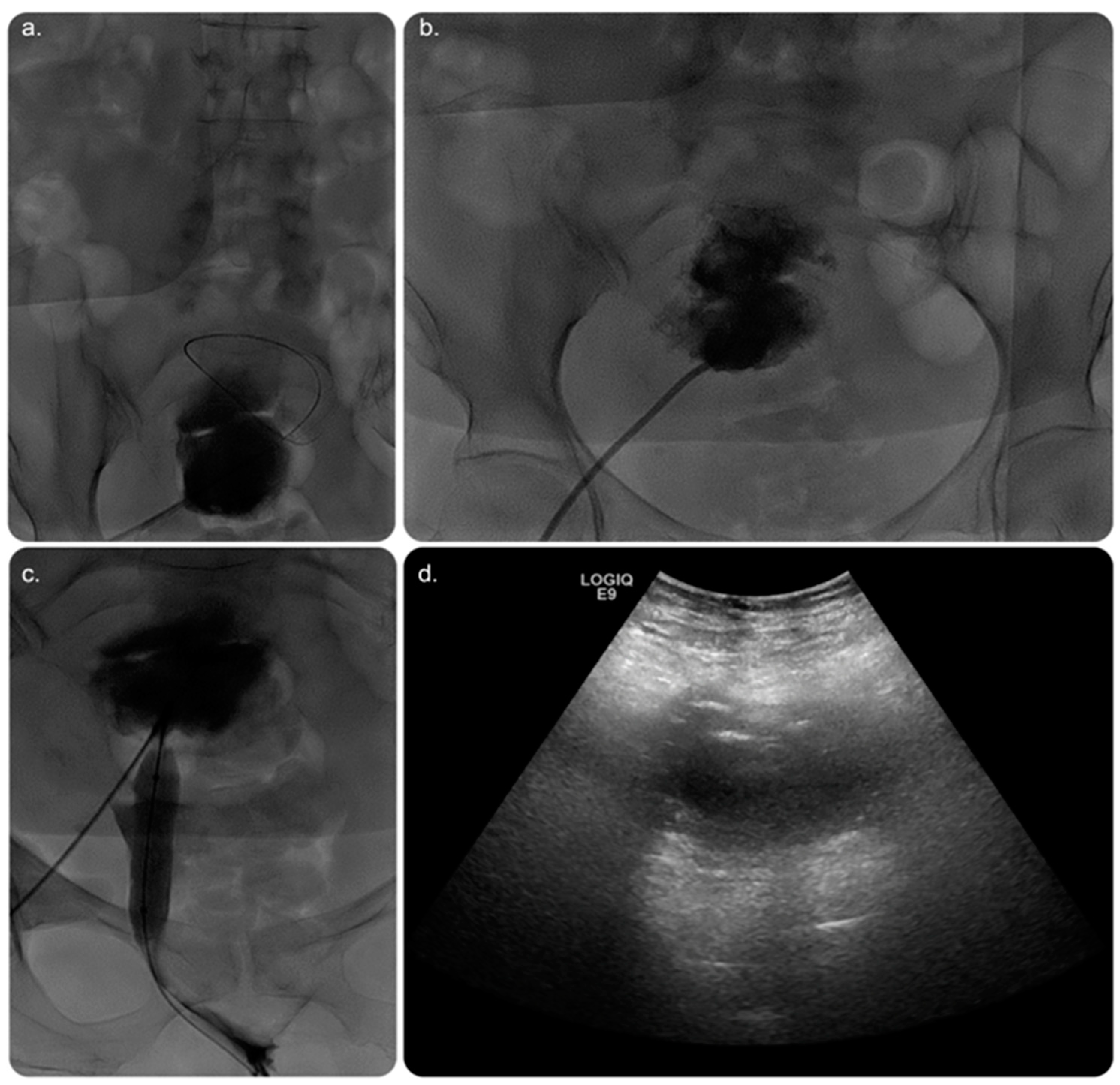
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Li, Z.; Li, L. The incidence and predictors of gynecologic malignancies among postmenopausal patients with endometrial fluid collection. Arch. Gynecol. Obstet. 2019, 299, 1071–1076. [Google Scholar] [CrossRef] [PubMed]
- Takeuchi, M.; Matsuzaki, K.; Uehara, H.; Yoshida, S.; Nishitani, H.; Shimazu, H. Pathologies of the uterine endometrial cavity: Usual and unusual manifestations and pitfalls on magnetic resonance imaging. Eur. Radiol. 2005, 15, 2244–2255. [Google Scholar] [CrossRef]
- Chan, L.Y.; Lau, T.K.; Wong, S.F.; Yuen, P.M. Pyometra. What is its clinical significance? J. Reprod. Med. 2001, 46, 952–956. [Google Scholar] [CrossRef]
- Browne, I.L. Spontaneous perforation of pyometra—Is hysterectomy required in the emergent setting? A case report and literature review. J. Surg. Case Rep. 2022, 2022, rjac388. [Google Scholar] [CrossRef] [PubMed]
- Yazawa, H.; Imaizumi, K. Generalized peritonitis secondary to spontaneously perforated pyometra in elderly women: Two cases with different clinical courses and surgical approaches and review of the literature. Fukushima J. Med. Sci. 2020, 66, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Malvadkar, S.M.; Malvadkar, M.S.; Domkundwar, S.V.; Mohd, S. Spontaneous rupture of pyometra causing peritonitis in elderly female diagnosed on dynamic transvaginal ultrasound. Case Rep. Radiol. 2016, 2016, 1738521. [Google Scholar] [CrossRef] [PubMed]
- Sawabe, M.; Takubo, K.; Esaki, Y.; Hatano, N.; Noro, T.; Nokubi, M. Occasional Review: Spontaneous Uterine Perforation as a Serious Complication of Pyometra in Elderly Females. Aust. N. Z. J. Obstet. Gynaecol. 1995, 35, 87–91. [Google Scholar] [CrossRef]
- Sala, A.; Restaino, S.; De Carlo, C.; Comand, M.; Frigo, A.; Rivero, S.M.; Zanetti, E.; Driul, L. Postoperative Streptococcus constellatus bacteremia in a 75-year-old patient with pyometra: A case report. Am. J. Case Rep. 2021, 22, e931167-1. [Google Scholar] [CrossRef]
- Huang, Y.; Tian, Q. Postmenopausal spontaneous rupture of pyometra: A case report. Medicine 2018, 97, e13659. [Google Scholar] [CrossRef]
- Hashmi, M.; Ravi, G.; Khan, A. Spontaneous perforation of uterus presenting with pneumoperitoneum. Eur. J. Mol. Clin. Med. 2023, 10, 1605–1610. Available online: https://ejmcm.com/article_22669.html (accessed on 1 March 2023).
- Goldstein, S.R. Postmenopausal endometrial fluid collections revisited: Look at the doughnut rather than the hole. Obstet. Gynecol. 1994, 83, 738–740. [Google Scholar] [PubMed]
- Álvarez-Sarrado, L.; Puente-Luján, M.J.; González-Ballano, I.; Martínez-Suñer, S.; Ortega-Marcilla, S.; Rodríguez-Solanilla, B. Treatment with ultrasound-guided percutaneous drainage of complicated post-cesarean vesicouterine hematomas. Experience in 4 cases. Ginecol. Y Obstet. De México 2020, 88, 542–548. [Google Scholar] [CrossRef]
- Chang, S.; Sekhon, L.; Lee, J.A.; Gounko, D.; Grunfeld, L.; Copperman, A. Management of fluid accumulation within the endometrial cavity during a frozen embryo transfer cycle. Fertil. Steril. 2018, 109, e17–e18. [Google Scholar] [CrossRef]
- Zreik, T.; Dickey, K.; Keefe, D.; Glickman, M.; Olive, D. Fluoroscopically guided cervical dilatation in patients with infertility. J. Am. Assoc. Gynecol. Laparosc. 1996, 3 (Suppl. S4), S56. [Google Scholar] [CrossRef]
- Dickey, K.W.; Zreik, T.G.; Hsia, H.C.; Eschelman, D.J.; Keefe, D.L.; Olive, D.L.; Pollak, J.S.; Rosenblatt, M.; Glickman, M.G. Transvaginal uterine cervical dilation with fluoroscopic guidance: Preliminary results in patients with infertility. Radiology 1996, 200, 497–503. [Google Scholar] [CrossRef]
- Wood, M.A.; Kerrigan, K.L.; Burns, M.K.; Glenn, T.L.; Ludwin, A.; Christianson, M.S.; Bhagavath, B.; Lindheim, S.R. Overcoming the challenging cervix: Identification and techniques to access the uterine cavity. Obstet. Gynecol. Surv. 2018, 73, 641–649. [Google Scholar] [CrossRef]
- Tay, W.M.I.; Subramanian, M.; Chinchure, D.; Kok, S.X.S. Clinics in diagnostic imaging (199). Singap. Med. J. 2019, 60, 487. [Google Scholar] [CrossRef]
- Sherid, M.; Samo, S.; Sulaiman, S.; Husein, H.; Sifuentes, H.; Sridhar, S. Liver abscess and bacteremia caused by Lactobacillus: Role of probiotics? Case report and review of the literature. BMC Gastroenterol. 2016, 16, 138. [Google Scholar] [CrossRef]
- Mukai, S.; Isono, H.; Kondo, K.; Ihara, K.; Isono, M.; Ogawa, H. A Case of Pyometra Caused by Achromobacter xylosoxidans and γ-Streptococcus in an Elderly Frail Woman. Cureus 2022, 14, e32016. [Google Scholar] [CrossRef]
- Zahedi, R.; Uppal, S.; Mendiratta-Lala, M.; Higgins, E.J.; Nettles, A.N.; Maturen, K.E. Percutaneous image-guided pelvic procedures in women with gynecologic cancers: Utilization, complications, and impact on patient management. Abdom. Radiol. 2016, 41, 2460–2465. [Google Scholar] [CrossRef]
- Matsumoto, R.; Kuramoto, S.; Muronoi, T.; Oka, K.; Shimojyo, Y.; Kidani, A.; Hira, E.; Watanabe, H. Damage control surgery for spontaneous perforation of pyometra with septic shock: A case report. Acute Med. Surg. 2021, 8, e657. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Sharydah, A.M.; AlMulhim, A.A.; Al Shikmubarak, I.A.; Alhussaini, A.A.; Alehaideb, R.S.; Salman, R. Management of Pyometra Using a Novel Image-Guided Percutaneous Technique: A Case Report. Medicina 2023, 59, 689. https://doi.org/10.3390/medicina59040689
Al-Sharydah AM, AlMulhim AA, Al Shikmubarak IA, Alhussaini AA, Alehaideb RS, Salman R. Management of Pyometra Using a Novel Image-Guided Percutaneous Technique: A Case Report. Medicina. 2023; 59(4):689. https://doi.org/10.3390/medicina59040689
Chicago/Turabian StyleAl-Sharydah, Abdulaziz Mohammad, Abdulaziz Abdullah AlMulhim, Ibrahim Abdulhakim Al Shikmubarak, Abdulmohsen Ahmed Alhussaini, Raghad Sulaiman Alehaideb, and Refaat Salman. 2023. "Management of Pyometra Using a Novel Image-Guided Percutaneous Technique: A Case Report" Medicina 59, no. 4: 689. https://doi.org/10.3390/medicina59040689
APA StyleAl-Sharydah, A. M., AlMulhim, A. A., Al Shikmubarak, I. A., Alhussaini, A. A., Alehaideb, R. S., & Salman, R. (2023). Management of Pyometra Using a Novel Image-Guided Percutaneous Technique: A Case Report. Medicina, 59(4), 689. https://doi.org/10.3390/medicina59040689





