Effect of Adding Kinesio Taping to Exercise Therapy in the Treatment of Patellofemoral Pain Syndrome
Abstract
:1. Introduction
2. Materials and Methods
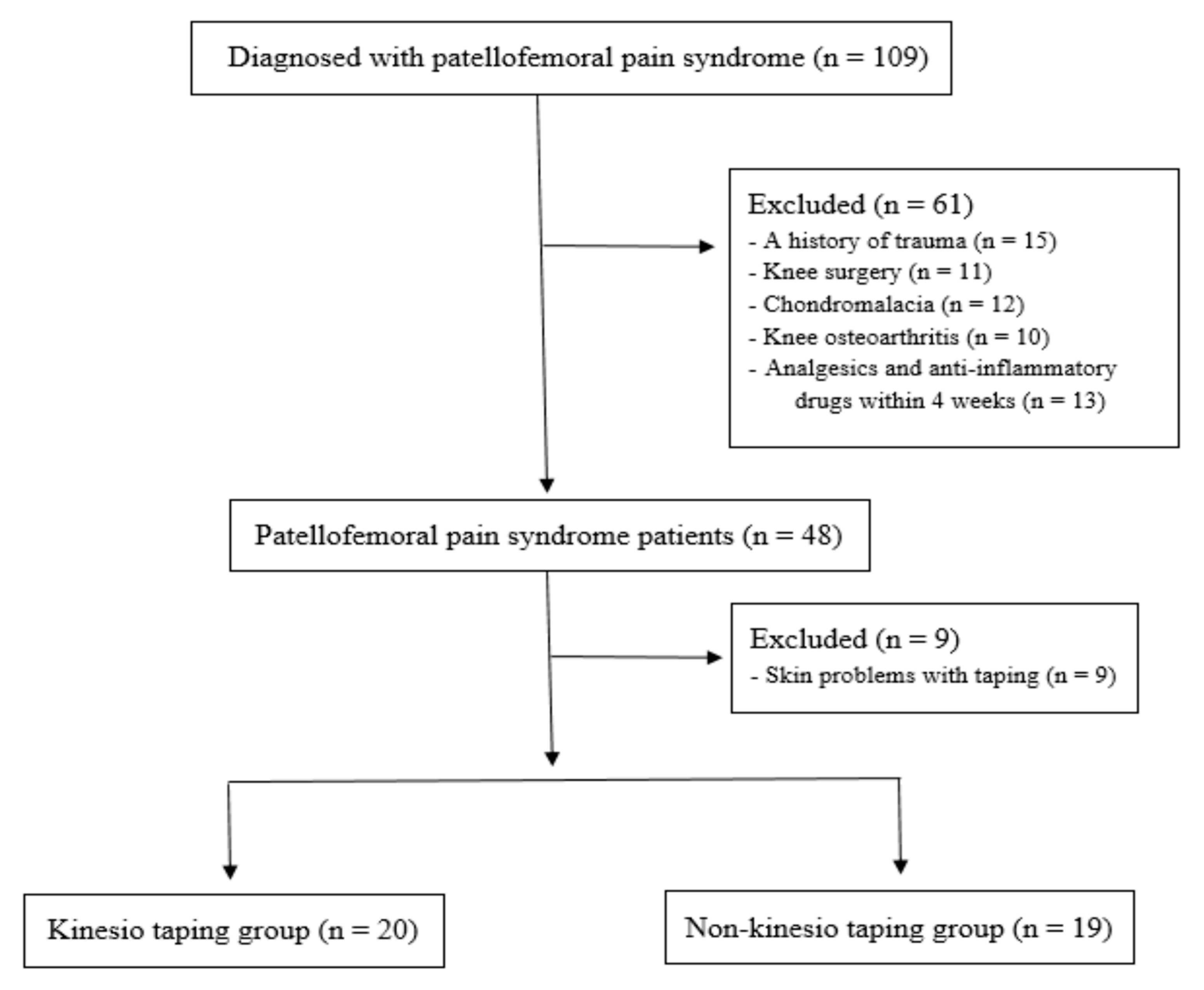
2.1. Study Design and Patient Enrollment
2.2. Evaluation Tests
2.2.1. Quadriceps Muscle Strength and Rate of Force Generation
2.2.2. Patient-Reported Outcomes: Pain and Function
2.3. Patellar Taping Intervention
2.4. Conservative Therapeutic Exercise
2.5. Statistical Analysis
3. Results
3.1. Comparison of Functional Outcomes in Each Group
3.2. Comparison of Functional Outcomes between Two Groups
4. Discussion
4.1. Effect of Adding KT on Quadriceps Muscle Strength
4.2. Effect of Additional KT on the Rate of Force Generation in Quadriceps Muscle
4.3. Effect of Additional KT on Patient-Reported Pain and Functional Performance (AKPS)
4.4. Clinical Implications
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Devereaux, M.D.; Lachmann, S.M. Patello-femoral arthralgia in athletes attending a Sports Injury Clinic. Br. J. Sport. Med. 1984, 18, 18–21. [Google Scholar] [CrossRef] [PubMed]
- Lankhorst, N.E.; Bierma-Zeinstra, S.M.; van Middelkoop, M. Factors associated with patellofemoral pain syndrome: A systematic review. Br. J. Sport. Med. 2013, 47, 193–206. [Google Scholar] [CrossRef] [PubMed]
- Willy, R.W.; Hoglund, L.T.; Barton, C.J.; Bolgla, L.A.; Scalzitti, D.A.; Logerstedt, D.S.; Lynch, A.D.; Snyder-Mackler, L.; McDonough, C.M. Patellofemoral Pain. J. Orthop. Sport. Phys. Ther. 2019, 49, cpg1–cpg95. [Google Scholar] [CrossRef] [PubMed]
- Crossley, K.; Bennell, K.; Green, S.; McConnell, J. A systematic review of physical interventions for patellofemoral pain syndrome. Clin. J. Sport Med. 2001, 11, 103–110. [Google Scholar] [CrossRef]
- Kellish, A.S.; Kellish, P.; Hakim, A.; Miskiel, S.; Shahi, A.; Kellish, A. What Is the Effect on Kinesio Taping on Pain and Gait in Patients with Patellofemoral Pain Syndrome? Cureus 2020, 12, e8982. [Google Scholar] [CrossRef]
- Akbaş, E.; Atay, A.O.; Yüksel, I. The effects of additional kinesio taping over exercise in the treatment of patellofemoral pain syndrome. Acta Orthop. Traumatol. Turc. 2011, 45, 335–341. [Google Scholar] [CrossRef]
- Stedge, H.L.; Kroskie, R.M.; Docherty, C.L. Kinesio taping and the circulation and endurance ratio of the gastrocnemius muscle. J. Athl. Train. 2012, 47, 635–642. [Google Scholar] [CrossRef] [PubMed]
- Logan, C.A.; Bhashyam, A.R.; Tisosky, A.J.; Haber, D.B.; Jorgensen, A.; Roy, A.; Provencher, M.T. Systematic Review of the Effect of Taping Techniques on Patellofemoral Pain Syndrome. Sport. Health 2017, 9, 456–461. [Google Scholar] [CrossRef]
- Kuru, T.; Yalıman, A.; Dereli, E.E. Comparison of efficiency of Kinesio® taping and electrical stimulation in patients with patellofemoral pain syndrome. Acta Orthop. Traumatol. Turc. 2012, 46, 385–392. [Google Scholar] [CrossRef]
- Günay, E.; Sarıkaya, S.; Özdolap, Ş.; Büyükuysal, Ç. Effectiveness of the kinesiotaping in the patellofemoral pain syndrome. Turk. J. Phys. Med. Rehabil. 2017, 63, 299–306. [Google Scholar] [CrossRef]
- Herrington, L. The effect of patellar taping on quadriceps peak torque and perceived pain: A preliminary study. Phys. Ther. Sport 2001, 2, 23–28. [Google Scholar] [CrossRef]
- Keet, J.H.; Gray, J.; Harley, Y.; Lambert, M.I. The effect of medial patellar taping on pain, strength and neuromuscular recruitment in subjects with and without patellofemoral pain. Physiotherapy 2007, 93, 45–52. [Google Scholar] [CrossRef]
- Aytar, A.; Ozunlu, N.; Surenkok, O.; Baltacı, G.; Oztop, P.; Karatas, M. Initial effects of kinesio® taping in patients with patellofemoral pain syndrome: A randomized, double-blind study. Isokinet. Exerc. Sci. 2011, 19, 135–142. [Google Scholar] [CrossRef]
- Gilleard, W.; McConnell, J.; Parsons, D. The effect of patellar taping on the onset of vastus medialis obliquus and vastus lateralis muscle activity in persons with patellofemoral pain. Phys. Ther. 1998, 78, 25–32. [Google Scholar] [CrossRef]
- Cowan, S.M.; Bennell, K.L.; Hodges, P.W. Therapeutic patellar taping changes the timing of vasti muscle activation in people with patellofemoral pain syndrome. Clin. J. Sport Med. 2002, 12, 339–347. [Google Scholar] [CrossRef]
- Callaghan, M.J.; Selfe, J. Patellar taping for patellofemoral pain syndrome in adults. Cochrane Database Syst. Rev. 2012, 4, Cd006717. [Google Scholar] [CrossRef]
- Gulati, A.; McElrath, C.; Wadhwa, V.; Shah, J.P.; Chhabra, A. Current clinical, radiological and treatment perspectives of patellofemoral pain syndrome. Br. J. Radiol. 2018, 91, 20170456. [Google Scholar] [CrossRef] [PubMed]
- Jibri, Z.; Jamieson, P.; Rakhra, K.S.; Sampaio, M.L.; Dervin, G. Patellar maltracking: An update on the diagnosis and treatment strategies. Insights Imaging 2019, 10, 65. [Google Scholar] [CrossRef]
- Lee, J.H.; Jang, K.M.; Kim, E.; Rhim, H.C.; Kim, H.D. Effects of Static and Dynamic Stretching with Strengthening Exercises in Patients with Patellofemoral Pain Who Have Inflexible Hamstrings: A Randomized Controlled Trial. Sport. Health 2021, 13, 49–56. [Google Scholar] [CrossRef]
- Van Cingel, R.E.; Kleinrensink, G.; Uitterlinden, E.J.; Rooijens, P.P.; Mulder, P.G.; Aufdemkampe, G.; Stoeckart, R. Repeated ankle sprains and delayed neuromuscular response: Acceleration time parameters. J. Orthop. Sport. Phys. Ther. 2006, 36, 72–79. [Google Scholar] [CrossRef]
- Wilkerson, G.B.; Nitz, A.J. Dynamic ankle stability: Mechanical and neuromuscular interrelationships. J. Sport Rehabil. 1994, 3, 43–57. [Google Scholar] [CrossRef]
- Chen, W.L.; Su, F.C.; Chou, Y.L. Significance of acceleration period in a dynamic strength testing study. J. Orthop. Sport. Phys. Ther. 1994, 19, 324–330. [Google Scholar] [CrossRef] [PubMed]
- Crossley, K.M.; Bennell, K.L.; Cowan, S.M.; Green, S. Analysis of outcome measures for persons with patellofemoral pain: Which are reliable and valid? Arch. Phys. Med. Rehabil. 2004, 85, 815–822. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Jang, K.M.; Kim, E.; Rhim, H.C.; Kim, H.D. Static and Dynamic Quadriceps Stretching Exercises in Patients with Patellofemoral Pain: A Randomized Controlled Trial. Sports Health 2021, 13, 482–489. [Google Scholar] [CrossRef]
- Kowall, M.G.; Kolk, G.; Nuber, G.W.; Cassisi, J.E.; Stern, S.H. Patellar taping in the treatment of patellofemoral pain. A prospective randomized study. Am. J. Sports Med. 1996, 24, 61–66. [Google Scholar] [CrossRef]
- Kaya, D.; Callaghan, M.J.; Ozkan, H.; Ozdag, F.; Atay, O.A.; Yuksel, I.; Doral, M.N. The effect of an exercise program in conjunction with short-period patellar taping on pain, electromyogram activity, and muscle strength in patellofemoral pain syndrome. Sport. Health 2010, 2, 410–416. [Google Scholar] [CrossRef]
- Mason, M.; Keays, S.L.; Newcombe, P.A. The effect of taping, quadriceps strengthening and stretching prescribed separately or combined on patellofemoral pain. Physiother. Res. Int. 2011, 16, 109–119. [Google Scholar] [CrossRef]
- Choi, I.R.; Lee, J.H. Effect of kinesiology tape application direction on quadriceps strength. Medicine 2018, 97, e11038. [Google Scholar] [CrossRef]
- Alexander, C.M.; McMullan, M.; Harrison, P.J. What is the effect of taping along or across a muscle on motoneurone excitability? A study using triceps surae. Man. Ther. 2008, 13, 57–62. [Google Scholar] [CrossRef]
- Christou, E.A. Patellar taping increases vastus medialis oblique activity in the presence of patellofemoral pain. J. Electromyogr. Kinesiol. 2004, 14, 495–504. [Google Scholar] [CrossRef]
- Irish, S.E.; Millward, A.J.; Wride, J.; Haas, B.M.; Shum, G.L. The effect of closed-kinetic chain exercises and open-kinetic chain exercise on the muscle activity of vastus medialis oblique and vastus lateralis. J. Strength Cond. Res. 2010, 24, 1256–1262. [Google Scholar] [CrossRef]
- Williams, S.; Whatman, C.; Hume, P.A.; Sheerin, K. Kinesio taping in treatment and prevention of sports injuries: A meta-analysis of the evidence for its effectiveness. Sport. Med. 2012, 42, 153–164. [Google Scholar] [CrossRef] [PubMed]
- Winters, M.; Holden, S.; Lura, C.B.; Welton, N.J.; Caldwell, D.M.; Vicenzino, B.T.; Weir, A.; Rathleff, M.S. Comparative effectiveness of treatments for patellofemoral pain: A living systematic review with network meta-analysis. Br. J. Sport. Med. 2020, 55, 369–377. [Google Scholar] [CrossRef] [PubMed]
- Maclachlan, L.R.; Collins, N.J.; Matthews, M.L.G.; Hodges, P.W.; Vicenzino, B. The psychological features of patellofemoral pain: A systematic review. Br. J. Sport. Med. 2017, 51, 732–742. [Google Scholar] [CrossRef] [PubMed]
- Selhorst, M.; Fernandez-Fernandez, A.; Schmitt, L.; Hoehn, J. Effect of a Psychologically Informed Intervention to Treat Adolescents with Patellofemoral Pain: A Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2021, 102, 1267–1273. [Google Scholar] [CrossRef] [PubMed]
- Priore, L.B.; Lack, S.; Garcia, C.; Azevedo, F.M.; de Oliveira Silva, D. Two Weeks of Wearing a Knee Brace Compared with Minimal Intervention on Kinesiophobia at 2 and 6 Weeks in People with Patellofemoral Pain: A Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2020, 101, 613–623. [Google Scholar] [CrossRef]

| Taping Group (n = 20) | Non-Taping Group (n = 19) | p-Value | |
|---|---|---|---|
| Sex (male/female) | 5/15 | 3/16 | 0.305 |
| Age (years) | 27.5 ± 5.4 | 27.3 ± 7.4 | 0.950 |
| Height (cm) | 167.5 ± 6.3 | 166.5 ± 7.8 | 0.658 |
| Weight (kg) | 62.6 ± 10.2 | 61.9 ± 6.9 | 0.804 |
| Body mass index (kg/m2) | 21.9 ± 2.3 | 22.2 ± 1.7 | 0.634 |
| Steps/day | 7829 ± 1511.7 | 8001 ± 1342.3 | 0.461 |
| Injured side (right/left) | 15/5 | 10/9 | |
| Sports and activity, n (low:high) | 9/11 | 7/12 |
| Taping Group | Non-Taping Group | MD (95% CI) | Cohen’s d | p Value | ||
|---|---|---|---|---|---|---|
| Quadriceps strength | Pretest | 87.3 ± 31.3 | 88.9 ± 37.8 | −1.6 (−23.4 to 20.2) | −0.04 | 0.884 |
| Posttest | 137.8 ± 52.2 | 162.9 ± 28.5 | −25.1 (−52.6 to 2.4) | −0.59 | 0.072 | |
| MD (95% CI) | −50.5 (−65.8 to −35.15) | −74.0 (−91.5 to −56.6) | ||||
| Cohen’s d | −1.17 | −2.21 | ||||
| p value | 0.001 | 0.001 | ||||
| Quadriceps AT | Pretest | 60.4 ± 16.1 | 70.5 ± 18.9 | −10.1 (−21.6 to 1.3) | −0.57 | 0.081 |
| Posttest | 48.7 ± 14.8 | 54.2 ± 13.0 | −5.5 (−14.6 to 3.6) | −0.39 | 0.227 | |
| MD (95% CI) | 11.7 (5.3 to 18.0) | 16.3 (9.3 to 23.4) | ||||
| Cohen’s d | 0.75 | 1.00 | ||||
| p value | 0.001 | 0.001 | ||||
| AKPS | Pretest | 52.5 ± 7.9 | 49.7 ± 6.6 | 2.7 (−1.9 to 7.5) | 0.38 | 0.244 |
| Posttest | 68.3 ± 9.3 | 69.9 ± 7.4 | −1.6 (−5.5 to 5.4) | −0.19 | 0.986 | |
| MD (95% CI) | −15.8 (−21.2 to −13.6) | −20.2 (−23.2 to −17.3) | ||||
| Cohen’s d | −1.83 | −2.88 | ||||
| p value | 0.001 | 0.001 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.H.; Rhim, H.C.; Jang, K.-M. Effect of Adding Kinesio Taping to Exercise Therapy in the Treatment of Patellofemoral Pain Syndrome. Medicina 2023, 59, 754. https://doi.org/10.3390/medicina59040754
Lee JH, Rhim HC, Jang K-M. Effect of Adding Kinesio Taping to Exercise Therapy in the Treatment of Patellofemoral Pain Syndrome. Medicina. 2023; 59(4):754. https://doi.org/10.3390/medicina59040754
Chicago/Turabian StyleLee, Jin Hyuck, Hye Chang Rhim, and Ki-Mo Jang. 2023. "Effect of Adding Kinesio Taping to Exercise Therapy in the Treatment of Patellofemoral Pain Syndrome" Medicina 59, no. 4: 754. https://doi.org/10.3390/medicina59040754
APA StyleLee, J. H., Rhim, H. C., & Jang, K.-M. (2023). Effect of Adding Kinesio Taping to Exercise Therapy in the Treatment of Patellofemoral Pain Syndrome. Medicina, 59(4), 754. https://doi.org/10.3390/medicina59040754








