Fluoride Exposure and ADHD: A Systematic Review of Epidemiological Studies
Abstract
:1. Introduction
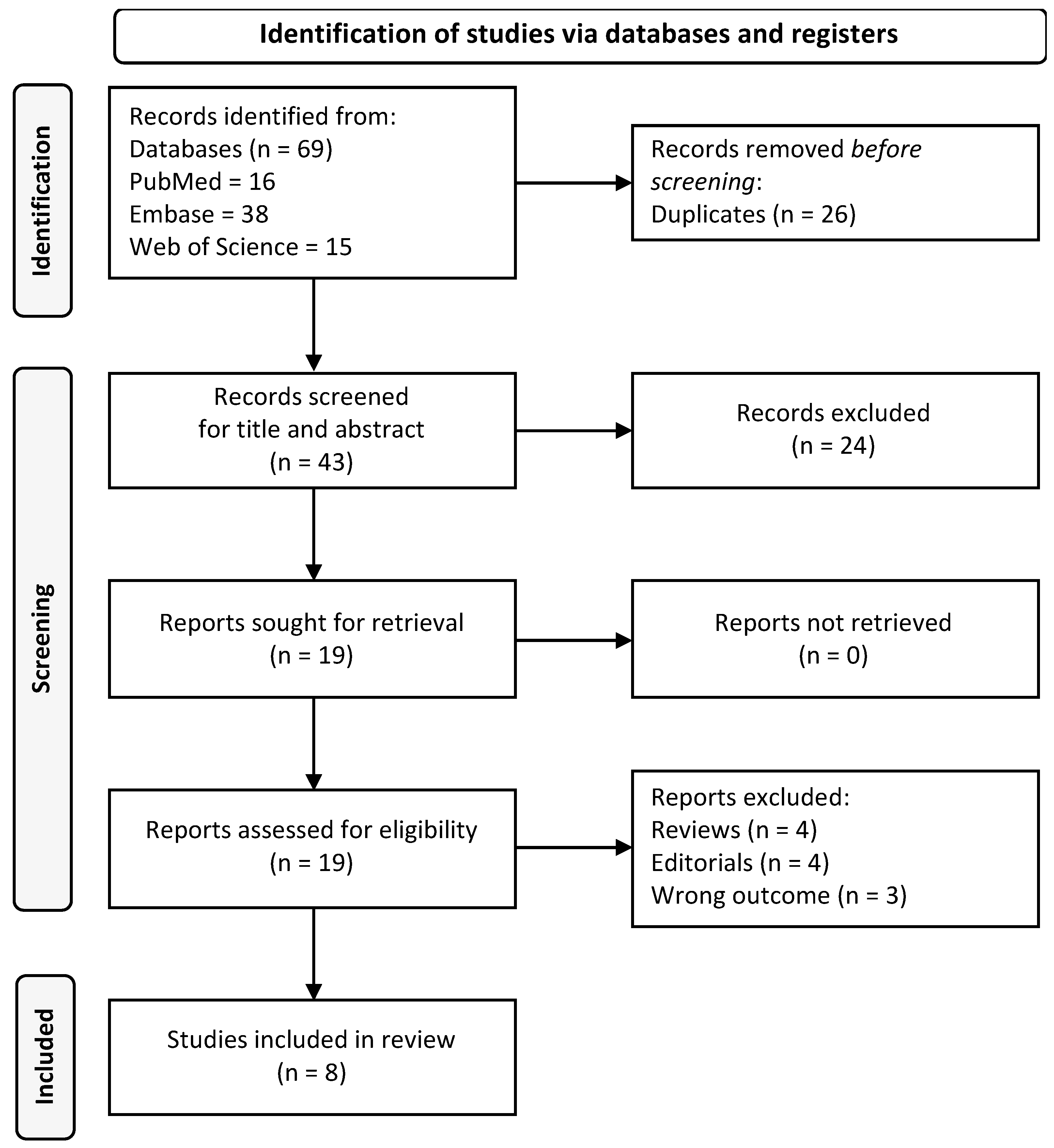
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Thapar, A.; Cooper, M. Attention deficit hyperactivity disorder. Lancet 2016, 387, 1240–1250. [Google Scholar] [CrossRef] [PubMed]
- Pichot, P. DSM-III: The 3d edition of the Diagnostic and Statistical Manual of Mental Disorders from the American Psychiatric Association. Rev. Neurol. 1986, 142, 489–499. [Google Scholar] [PubMed]
- Lange, K.W.; Reichl, S.; Lange, K.M.; Tucha, L.; Tucha, O. The history of attention deficit hyperactivity disorder. Atten. Deficit Hyperact. Disord. 2010, 2, 241–255. [Google Scholar] [CrossRef] [PubMed]
- Barkley, R.A.; Peters, H. The earliest reference to ADHD in the medical literature? Melchior Adam Weikard’s description in 1775 of “attention deficit” (Mangel der Aufmerksamkeit, Attentio Volubilis). J. Atten. Disord. 2012, 16, 623–630. [Google Scholar] [CrossRef]
- Vahia, V.N. Diagnostic and statistical manual of mental disorders 5: A quick glance. Indian J. Psychiatry 2013, 55, 220–223. [Google Scholar] [CrossRef]
- Faraone, S.V.; Biederman, J.; Mick, E. The age-dependent decline of attention deficit hyperactivity disorder: A meta-analysis of follow-up studies. Psychol. Med. 2006, 36, 159–165. [Google Scholar] [CrossRef]
- Di Lorenzo, R.; Balducci, J.; Poppi, C.; Arcolin, E.; Cutino, A.; Ferri, P.; D’Amico, R.; Filippini, T. Children and adolescents with ADHD followed up to adulthood: A systematic review of long-term outcomes. Acta Neuropsychiatr. 2021, 33, 283–298. [Google Scholar] [CrossRef]
- Polanczyk, G.V.; Willcutt, E.G.; Salum, G.A.; Kieling, C.; Rohde, L.A. ADHD prevalence estimates across three decades: An updated systematic review and meta-regression analysis. Int. J. Epidemiol. 2014, 43, 434–442. [Google Scholar] [CrossRef]
- Polanczyk, G.V.; Salum, G.A.; Sugaya, L.S.; Caye, A.; Rohde, L.A. Annual research review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J. Child Psychol. Psychiatry 2015, 56, 345–365. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence. Attention Deficit Hyperactivity Disorder: Diagnosis and Management; NICE guideline NG87; National Institute for Health and Care Excellence: London, UK, 2019. [Google Scholar]
- Posner, J.; Polanczyk, G.V.; Sonuga-Barke, E. Attention-deficit hyperactivity disorder. Lancet 2020, 395, 450–462. [Google Scholar] [CrossRef]
- Faraone, S.V.; Larsson, H. Genetics of attention deficit hyperactivity disorder. Mol. Psychiatry 2019, 24, 562–575. [Google Scholar] [CrossRef] [PubMed]
- Shaw, P.; Eckstrand, K.; Sharp, W.; Blumenthal, J.; Lerch, J.P.; Greenstein, D.; Clasen, L.; Evans, A.; Giedd, J.; Rapoport, J.L. Attention-deficit/hyperactivity disorder is characterized by a delay in cortical maturation. Proc. Natl. Acad. Sci. USA 2007, 104, 19649–19654. [Google Scholar] [CrossRef] [PubMed]
- Volkow, N.D.; Wang, G.J.; Tomasi, D.; Kollins, S.H.; Wigal, T.L.; Newcorn, J.H.; Telang, F.W.; Fowler, J.S.; Logan, J.; Wong, C.T.; et al. Methylphenidate-elicited dopamine increases in ventral striatum are associated with long-term symptom improvement in adults with attention deficit hyperactivity disorder. J. Neurosci. 2012, 32, 841–849. [Google Scholar] [CrossRef] [PubMed]
- Cortese, S. The neurobiology and genetics of Attention-Deficit/Hyperactivity Disorder (ADHD): What every clinician should know. Eur. J. Paediatr. Neurol. 2012, 16, 422–433. [Google Scholar] [CrossRef]
- Chen, Y. Organophosphate-induced brain damage: Mechanisms, neuropsychiatric and neurological consequences, and potential therapeutic strategies. Neurotoxicology 2012, 33, 391–400. [Google Scholar] [CrossRef] [PubMed]
- Wilens, T.E.; Decker, M.W. Neuronal nicotinic receptor agonists for the treatment of attention-deficit/hyperactivity disorder: Focus on cognition. Biochem. Pharmacol. 2007, 74, 1212–1223. [Google Scholar] [CrossRef]
- Potter, A.S.; Schaubhut, G.; Shipman, M. Targeting the nicotinic cholinergic system to treat attention-deficit/hyperactivity disorder: Rationale and progress to date. CNS Drugs 2014, 28, 1103–1113. [Google Scholar] [CrossRef]
- Forns, J.; Stigum, H.; Hoyer, B.B.; Sioen, I.; Sovcikova, E.; Nowack, N.; Lopez-Espinosa, M.J.; Guxens, M.; Ibarluzea, J.; Torrent, M.; et al. Prenatal and postnatal exposure to persistent organic pollutants and attention-deficit and hyperactivity disorder: A pooled analysis of seven European birth cohort studies. Int. J. Epidemiol. 2018, 47, 1082–1097. [Google Scholar] [CrossRef]
- Grandjean, P.; Landrigan, P.J. Neurobehavioural effects of developmental toxicity. Lancet Neurol. 2014, 13, 330–338. [Google Scholar] [CrossRef]
- Costa, L.G.; Cole, T.B.; Dao, K.; Chang, Y.C.; Coburn, J.; Garrick, J.M. Effects of air pollution on the nervous system and its possible role in neurodevelopmental and neurodegenerative disorders. Pharmacol. Ther. 2020, 210, 107523. [Google Scholar] [CrossRef]
- Banerjee, T.D.; Middleton, F.; Faraone, S.V. Environmental risk factors for attention-deficit hyperactivity disorder. Acta Paediatr. 2007, 96, 1269–1274. [Google Scholar] [CrossRef]
- Huang, S.; Hu, H.; Sanchez, B.N.; Peterson, K.E.; Ettinger, A.S.; Lamadrid-Figueroa, H.; Schnaas, L.; Mercado-Garcia, A.; Wright, R.O.; Basu, N.; et al. Childhood Blood Lead Levels and Symptoms of Attention Deficit Hyperactivity Disorder (ADHD): A Cross-Sectional Study of Mexican Children. Environ. Health Perspect. 2016, 124, 868–874. [Google Scholar] [CrossRef] [PubMed]
- Fuertes, E.; Standl, M.; Forns, J.; Berdel, D.; Garcia-Aymerich, J.; Markevych, I.; Schulte-Koerne, G.; Sugiri, D.; Schikowski, T.; Tiesler, C.M.; et al. Traffic-related air pollution and hyperactivity/inattention, dyslexia and dyscalculia in adolescents of the German GINIplus and LISAplus birth cohorts. Environ. Int. 2016, 97, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Perera, F.P.; Wheelock, K.; Wang, Y.; Tang, D.; Margolis, A.E.; Badia, G.; Cowell, W.; Miller, R.L.; Rauh, V.; Wang, S.; et al. Combined effects of prenatal exposure to polycyclic aromatic hydrocarbons and material hardship on child ADHD behavior problems. Environ. Res. 2018, 160, 506–513. [Google Scholar] [CrossRef] [PubMed]
- Robberecht, H.; Verlaet, A.A.J.; Breynaert, A.; De Bruyne, T.; Hermans, N. Magnesium, Iron, Zinc, Copper and Selenium Status in Attention-Deficit/Hyperactivity Disorder (ADHD). Molecules 2020, 25, 4440. [Google Scholar] [CrossRef]
- Farmus, L.; Till, C.; Green, R.; Hornung, R.; Martinez Mier, E.A.; Ayotte, P.; Muckle, G.; Lanphear, B.P.; Flora, D.B. Critical windows of fluoride neurotoxicity in Canadian children. Environ. Res. 2021, 200, 111315. [Google Scholar] [CrossRef] [PubMed]
- Grandjean, P. Developmental fluoride neurotoxicity: An updated review. Environ. Health 2019, 18, 110. [Google Scholar] [CrossRef]
- NHS-National Health System. Available online: https://www.nhs.uk/ (accessed on 31 March 2023).
- CDC-Center for Disease Control and Prevention. Available online: https://www.cdc.gov/ (accessed on 31 March 2023).
- Veneri, F.; Vinceti, M.; Generali, L.; Giannone, M.E.; Mazzoleni, E.; Birnbaum, L.S.; Consolo, U.; Filippini, T. Fluoride exposure and cognitive neurodevelopment: Systematic review and dose-response meta-analysis. Environ. Res. 2023, 221, 115239. [Google Scholar] [CrossRef]
- Grandjean, P.; Hu, H.; Till, C.; Green, R.; Bashash, M.; Flora, D.; Tellez-Rojo, M.M.; Song, P.X.K.; Lanphear, B.; Budtz-Jorgensen, E. A Benchmark Dose Analysis for Maternal Pregnancy Urine-Fluoride and IQ in Children. Risk Anal. 2022, 42, 439–449. [Google Scholar] [CrossRef]
- National Toxicology Program, Draft NTP Monograph on the Systematic Review of Fluoride Exposure and Neurodevelopmental and Cognitive Health Effects. 2020. Available online: https://fluoridealert.org/wp-content/uploads/ntp.revised-monograph.9-16-2020.pdf (accessed on 31 March 2023).
- Dec, K.; Lukomska, A.; Maciejewska, D.; Jakubczyk, K.; Baranowska-Bosiacka, I.; Chlubek, D.; Wasik, A.; Gutowska, I. The Influence of Fluorine on the Disturbances of Homeostasis in the Central Nervous System. Biol. Trace Elem. Res. 2017, 177, 224–234. [Google Scholar] [CrossRef]
- Miranda, G.H.N.; Alvarenga, M.O.P.; Ferreira, M.K.M.; Puty, B.; Bittencourt, L.O.; Fagundes, N.C.F.; Pessan, J.P.; Buzalaf, M.A.R.; Lima, R.R. A systematic review and meta-analysis of the association between fluoride exposure and neurological disorders. Sci. Rep. 2021, 11, 22659. [Google Scholar] [CrossRef] [PubMed]
- National Research Council. Fluoride in Drinking Water. A Scientific Review of EPA’s Standards. Available online: https://nap.nationalacademies.org/download/11571 (accessed on 31 March 2023).
- Peckham, S.; Lowery, D.; Spencer, S. Are fluoride levels in drinking water associated with hypothyroidism prevalence in England? A large observational study of GP practice data and fluoride levels in drinking water. J. Epidemiol. Community Health 2015, 69, 619–624. [Google Scholar] [CrossRef] [PubMed]
- Prezioso, G.; Giannini, C.; Chiarelli, F. Effect of Thyroid Hormones on Neurons and Neurodevelopment. Horm. Res. Paediatr. 2018, 90, 73–81. [Google Scholar] [CrossRef]
- Lee, A.C.; Yeung, L.K.; Barense, M.D. The hippocampus and visual perception. Front. Hum. Neurosci. 2012, 6, 91. [Google Scholar] [CrossRef] [PubMed]
- Levie, D.; Korevaar, T.I.M.; Bath, S.C.; Dalmau-Bueno, A.; Murcia, M.; Espada, M.; Dineva, M.; Ibarluzea, J.M.; Sunyer, J.; Tiemeier, H.; et al. Thyroid Function in Early Pregnancy, Child IQ, and Autistic Traits: A Meta-Analysis of Individual Participant Data. J. Clin. Endocrinol. Metab. 2018, 103, 2967–2979. [Google Scholar] [CrossRef]
- Strunecka, A.; Strunecky, O. Chronic Fluoride Exposure and the Risk of Autism Spectrum Disorder. Int. J. Environ. Res. Public Health 2019, 16, 3431. [Google Scholar] [CrossRef]
- Riddell, J.K.; Malin, A.J.; Flora, D.; McCague, H.; Till, C. Association of water fluoride and urinary fluoride concentrations with attention deficit hyperactivity disorder in Canadian youth. Environ. Int. 2019, 133, 105190. [Google Scholar] [CrossRef]
- Bashash, M.; Marchand, M.; Hu, H.; Till, C.; Martinez-Mier, E.A.; Sanchez, B.N.; Basu, N.; Peterson, K.E.; Green, R.; Schnaas, L.; et al. Prenatal fluoride exposure and attention deficit hyperactivity disorder (ADHD) symptoms in children at 6-12 years of age in Mexico City. Environ. Int. 2018, 121, 658–666. [Google Scholar] [CrossRef]
- Malin, A.J.; Till, C. Exposure to fluoridated water and attention deficit hyperactivity disorder prevalence among children and adolescents in the United States: An ecological association. Environ. Health 2015, 14, 17. [Google Scholar] [CrossRef]
- Perrott, K.W. Fluoridation and attention deficit hyperactivity disorder-a critique of Malin and Till (2015). Br. Dent. J. 2018, 223, 819–822. [Google Scholar] [CrossRef]
- Adkins, E.A.; Yolton, K.; Strawn, J.R.; Lippert, F.; Ryan, P.H.; Brunst, K.J. Fluoride exposure during early adolescence and its association with internalizing symptoms. Environ. Res. 2022, 204, 112296. [Google Scholar] [CrossRef]
- Wang, A.; Duan, L.; Huang, H.; Ma, J.; Zhang, Y.; Ma, Q.; Guo, Y.; Li, Z.; Cheng, X.; Zhu, J.; et al. Association between fluoride exposure and behavioural outcomes of school-age children: A pilot study in China. Int. J. Environ. Health Res. 2022, 32, 232–241. [Google Scholar] [CrossRef]
- Barberio, A.M.; Quinonez, C.; Hosein, F.S.; McLaren, L. Fluoride exposure and reported learning disability diagnosis among Canadian children: Implications for community water fluoridation. Can. J. Public Health 2017, 108, e229–e239. [Google Scholar] [CrossRef] [PubMed]
- Khairkar, P.; Palicarp, S.M.; Kamble, A.; Alladi, S.; Thomas, S.; Bommadi, R.; Mohanty, S.; Reddy, R.; Jothula, K.Y.; Anupama, K.; et al. Outcome of Systemic Fluoride Effects on Developmental Neurocognitions and Psychopathology in Adolescent Children. Indian J. Pediatr. 2021, 88, 1264. [Google Scholar] [CrossRef] [PubMed]
- Huber, R.S.; Kim, T.S.; Kim, N.; Kuykendall, M.D.; Sherwood, S.N.; Renshaw, P.F.; Kondo, D.G. Association Between Altitude and Regional Variation of ADHD in Youth. J. Atten. Disord. 2018, 22, 1299–1306. [Google Scholar] [CrossRef]
- Yolton, K.; Cornelius, M.; Ornoy, A.; McGough, J.; Makris, S.; Schantz, S. Exposure to neurotoxicants and the development of attention deficit hyperactivity disorder and its related behaviors in childhood. Neurotoxicol. Teratol. 2014, 44, 30–45. [Google Scholar] [CrossRef] [PubMed]
- Carrieri, M.; Trevisan, A.; Bartolucci, G.B. Adjustment to concentration-dilution of spot urine samples: Correlation between specific gravity and creatinine. Int. Arch. Occup. Environ. Health 2001, 74, 63–67. [Google Scholar] [CrossRef]
- Wang, W.; Du, C.; Lin, L.; Chen, W.; Tan, L.; Shen, J.; Pearce, E.N.; Zhang, Y.; Gao, M.; Bian, J.; et al. Anthropometry-based 24-h urinary creatinine excretion reference for Chinese children. PLoS ONE 2018, 13, e0197672. [Google Scholar] [CrossRef]
- Mayes, S.D.; Calhoun, S.L.; Crowell, E.W. Learning disabilities and ADHD: Overlapping spectrumn disorders. J. Learn. Disabil. 2000, 33, 417–424. [Google Scholar] [CrossRef]
- Pham, A.V.; Riviere, A. Specific Learning Disorders and ADHD: Current Issues in Diagnosis Across Clinical and Educational Settings. Curr. Psychiatry Rep. 2015, 17, 38. [Google Scholar] [CrossRef]
- Roth, T.L. Epigenetics of neurobiology and behavior during development and adulthood. Dev. Psychobiol. 2012, 54, 590–597. [Google Scholar] [CrossRef] [PubMed]
- Till, C.; Green, R.; Flora, D.; Hornung, R.; Martinez-Mier, E.A.; Blazer, M.; Farmus, L.; Ayotte, P.; Muckle, G.; Lanphear, B. Fluoride exposure from infant formula and child IQ in a Canadian birth cohort. Environ. Int. 2020, 134, 105315. [Google Scholar] [CrossRef] [PubMed]
- Till, C.; Green, R.; Lanphear, B. Association Between Maternal Fluoride Exposure and Child IQ-Reply. JAMA Pediatr. 2020, 174, 216–217. [Google Scholar] [CrossRef] [PubMed]
| Database | Search Strategy |
|---|---|
| PubMed | ((fluoride) AND ((ADHD) OR (attention deficit hyperactivity disorder)) |
| Embase | (‘fluoride’/exp OR fluoride) AND (‘adhd’/exp OR adhd OR ‘attention deficit hyperactivity disorder’/exp OR ‘attention deficit hyperactivity disorder’ OR ((‘attention’/exp OR attention) AND deficit AND (‘hyperactivity’/exp OR hyperactivity) AND (‘disorder’/exp OR disorder))) |
| Web of Science | fluoride AND ADHD |
| Reference | Country | Study Type | Aim of the Study | Population | Number of Samples | Fluoride Exposure Method | Average Fluoride Levels | ADHD Assessment | Main Findings | Adjustment Factors |
|---|---|---|---|---|---|---|---|---|---|---|
| Bashash et al., 2018 [43] | Mexico | Cohort study (ELEMENT project) | To assess the relation between prenatal exposure to fluoride and ADHD | Mother-child pairs | 210 | Maternal Urinary fluoride adjusted for creatinine (MUFcr) | The overall mean level of MUFcr averaged across all trimesters was 0.85 mg/L, with an Interquartile Range (IQR) of 0.46 mg/L | CRS-R or CPT-II or DSM-IV Hyperactivity-Impulsivity scale, DSM-IV ADHD scale, DSM-IV Inattention scale | Association between MUFcr and CRS-R for DSM-IV Inattention and Cognitive problems and inattention, not hyperactivity or impulse control | Smoking, maternal education, child sex, HOME score, exposure to other contaminants |
| Malin and Till 2015 [44]; Perrott 2018 [45] | USA | Cross-sectional ecological survey [National Survey of Children’s Health (2003, 2007, 2011)] | To examine the relation between exposure to fluoridated water and ADHD prevalence among children and adolescents | Children aged 4–17 | 2003: 79,264 2007: 73,123 2011: 76,015 | Centers for Disease Control and Prevention (CDC) website provide data on the number of people receiving fluoridated water from public water supplies in each of America’s 50 states | - | Parent reported health care provider-diagnosed ADHD | Prevalence of ADHD increased from 7.8% in 2003 to 11% in 2011. Water fluoridation prevalence was positively associated with ADHD. The association between water fluoride exposure and ADHD incidence disappears once elevation is included in the multiple regression analysis. | Socioeconomic status in the first report and mean state elevation, median household income, smoking prevalence 2013, water fluoridation in 1992, obese youth average 2003–2004, longitude, home ownership, per capita personal income 2009, low birth rate 2005, bachelor’s degree 2000, age over 65 in the fully adjusted model |
| Riddell et al., 2019 [42] | Canada | Cross-sectional survey [Canadian Health Measures Survey (Cycles 2 and 3)] | To examine the relation between urinary and tap water fluoride concentration and attention-related outcomes | Children aged 6–17 | 1877 UF 1722 Community Water Fluoridation (CWF) status 980 tap water sample | Urinary fluoridation (UF), city fluoridation status, tap water fluoride | The mean urinary fluoride adjusted for specific gravity (UFSG) concentration was 0.61 mg/L among the 1877 youths from Cycles 2 and 3 | ADHD diagnosis SDQ Hyperactivity-inattention subscale | Children exposed to higher tap water fluoride levels had a higher risk of receiving an ADHD diagnosis. UF levels were not associated with ADHD or symptom-related | Sex, age, ethnicity, BMI, level of parental education, household income, cigarette smoke exposure, blood lead level |
| Adkins et al., 2022 [46] | USA | Cross-sectional study [CCAAPS] | To examine the association between UF and internalizing symptoms among adolescents, also evaluating sex differences | Adolescents | 334 | UF | UF concentrations at Age-12 visit was 0.88 (0.36) mg/L | Parent reported BASC-2 scale | UF concentration are positively associated with internalizing behaviors, particularly somatization. | Race, sex, age, total family income at age-12 visit, maternal depression, serum cotinine, PRQ relational frustration |
| Wang et al., 2022 [47] | China | Cross-sectional study | To investigate the relation between fluoride exposure and behavioral outcomes among children | Primary schools’ children | 325 | UF | The mean ± SD levels of UF was 1.54 ± 0.89 mg/L | CPRS-48 (ADHD Index) | UF associated with psychosomatic problems, no correlation with ADHD | Age, BMI, urinary creatinine, sex, parents migrated |
| Barberio et al., 2017 [48] | Canada | Cross-sectional survey [Canadian Health Measures Survey] | To examine the association between fluoride exposure and learning disabilities. | Children aged 3–12 | Cycle 2 = 1120 Cycle 3 = 1101 | UF, creatinine-adjusted urinary fluoride, gravity-adjusted urinary fluoride, tap water sample | UFSG Cycle 2 fluoride subsample: 37.78 µmol/L Cycle 2 constrained fluoride subsample = 43.46 µmol/L Cycle 3 fluoride subsample: 34.25 µmol/L Cycle 3 constrained fluoride subsample: 40.71 µmol/L | Response to items of the survey | No association between UF and learning disabilities and ADHD diagnosis. | Sex, age, household education, household income adequacy |
| Khairkar et al., 2021 [49] | India | Case–control study (Letter to editor) | To analyze the outcome of spectral severity of water fluoride levels in adolescents on their neurocognitive and neuropsychiatric disorders | Adolescents aged 11–15 | 150 | Level of fluoride in community water | - | Not specified | Significant association between fluoride exposure and ADHD, disruptive behaviors, defiant disorder and scholastic arithmetic skill disorders | Not specified |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fiore, G.; Veneri, F.; Di Lorenzo, R.; Generali, L.; Vinceti, M.; Filippini, T. Fluoride Exposure and ADHD: A Systematic Review of Epidemiological Studies. Medicina 2023, 59, 797. https://doi.org/10.3390/medicina59040797
Fiore G, Veneri F, Di Lorenzo R, Generali L, Vinceti M, Filippini T. Fluoride Exposure and ADHD: A Systematic Review of Epidemiological Studies. Medicina. 2023; 59(4):797. https://doi.org/10.3390/medicina59040797
Chicago/Turabian StyleFiore, Gianluca, Federica Veneri, Rosaria Di Lorenzo, Luigi Generali, Marco Vinceti, and Tommaso Filippini. 2023. "Fluoride Exposure and ADHD: A Systematic Review of Epidemiological Studies" Medicina 59, no. 4: 797. https://doi.org/10.3390/medicina59040797
APA StyleFiore, G., Veneri, F., Di Lorenzo, R., Generali, L., Vinceti, M., & Filippini, T. (2023). Fluoride Exposure and ADHD: A Systematic Review of Epidemiological Studies. Medicina, 59(4), 797. https://doi.org/10.3390/medicina59040797









