Combined Free Flaps for Optimal Orthoplastic Lower Limb Reconstruction: A Retrospective Series
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Surgical Technique
3.2. Case Series
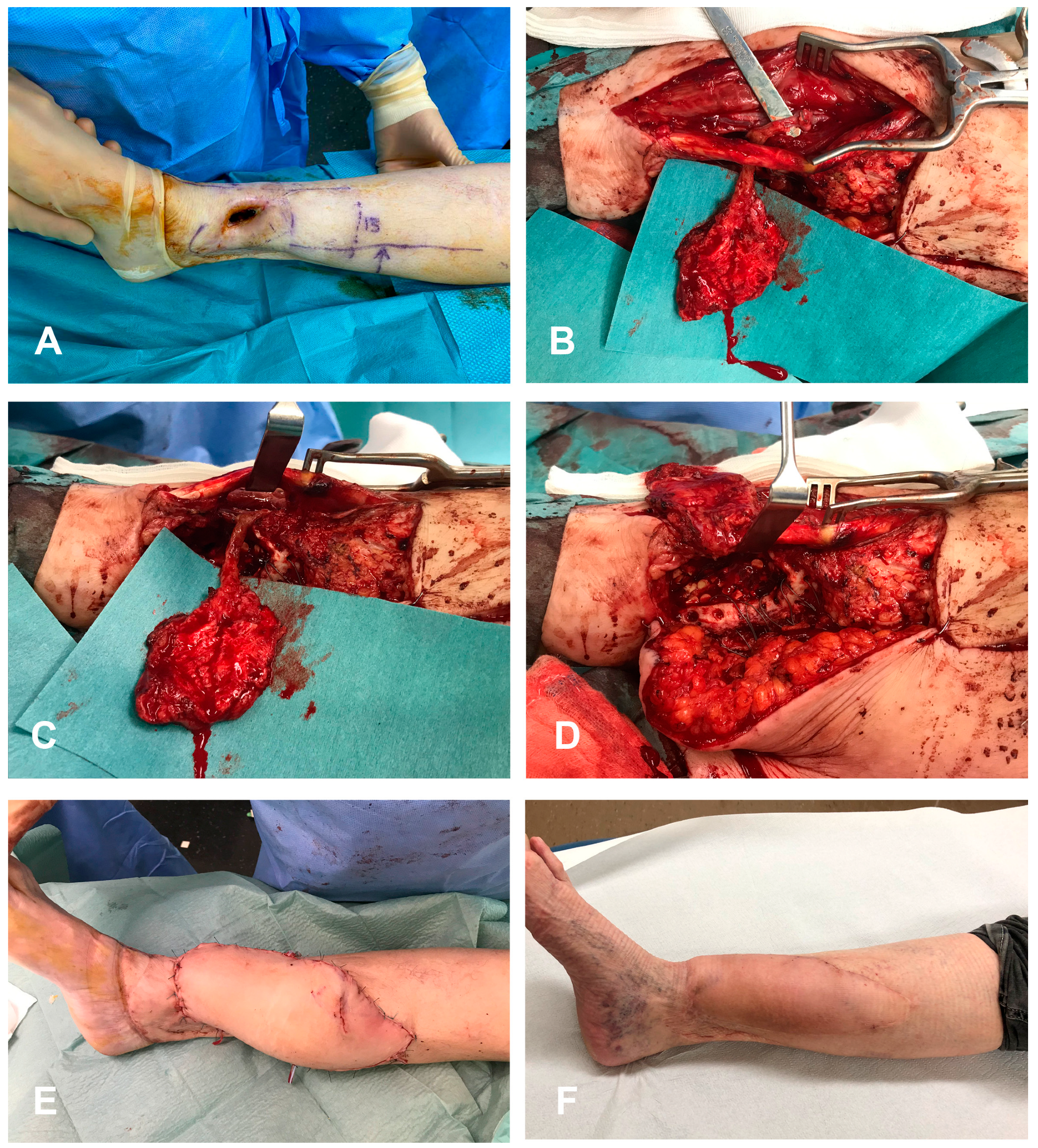
3.2.1. Case 1 (Patient No. 2)
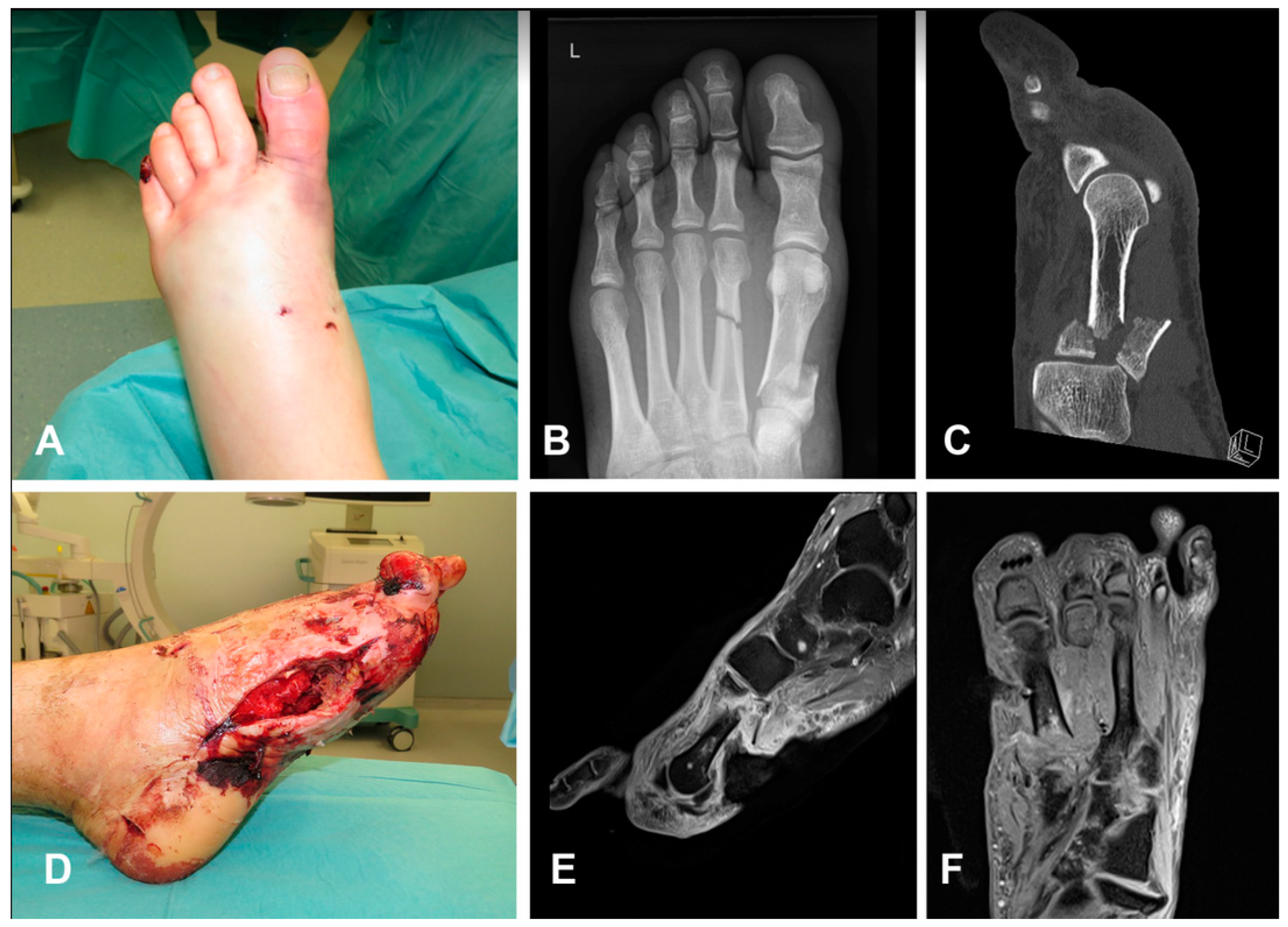
3.2.2. Case 2 (Patient No. 6)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gajendran, V.K.; Gajendran, V.K.; Malone, K.J. Management of complications with hand fractures. Hand Clin. 2015, 31, 165–177. [Google Scholar] [CrossRef] [PubMed]
- Choudry, U.H.; Bakri, K.; Moran, S.L.; Karacor, Z.; Shin, A.Y. The vascularized medial femoral condyle periosteal bone flap for the treatment of recalcitrant bony nonunions. Ann. Plast. Surg. 2008, 60, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Choudry, U.; Moran, S.; Karacor, Z. Soft-tissue coverage and outcome of gustilo grade IIIB midshaft tibia fractures: A 15-year experience. Plast. Reconstr. Surg. 2008, 122, 479–485. [Google Scholar] [CrossRef] [PubMed]
- Ring, D. Malunion and nonunion of the metacarpals and phalanges. Instr. Course Lect. 2006, 55, 121–128. [Google Scholar] [CrossRef]
- Ekegren, C.L.; Edwards, E.R.; de Steiger, R.; Gabbe, B.J. Incidence, Costs and Predictors of Non-Union, Delayed Union and Mal-Union Following Long Bone Fracture. Int. J. Environ. Res. Public Health 2018, 15, 2845. [Google Scholar] [CrossRef]
- Shimbo, K.; Shinomiya, R.; Sunagawa, T.; Adachi, N. Risk assessment in delayed free flap reconstruction for severe lower extremity trauma. Eur. J. Orthop. Surg. Traumatol. 2022. [Google Scholar] [CrossRef]
- Sapino, G.; Guiller, D.; Osinga, R.; Martineau, J.; De Santis, G.; Steinmetz, S.; di Summa, P.G. Muscle-only versus chimeric musculocutaneous gastrocnemius pedicled flap in complex orthoplastic reconstructions of the knee region: A retrospective study. J. Plast. Reconstr. Aesthet. Surg. 2023, 77, 298–308. [Google Scholar] [CrossRef]
- Muller, S.L.C.; Morgenstern, M.; Kuehl, R.; Muri, T.; Kalbermatten, D.F.; Clauss, M.; Schaefer, D.J.; Sendi, P.; Osinga, R. Soft-tissue reconstruction in lower-leg fracture-related infections: An orthoplastic outcome and risk factor analysis. Injury 2021, 52, 3489–3497. [Google Scholar] [CrossRef]
- Yazar, S.; Lin, C.H.; Wei, F.C. One-stage reconstruction of composite bone and soft-tissue defects in traumatic lower extremities. Plast. Reconstr. Surg. 2004, 114, 1457–1466. [Google Scholar] [CrossRef]
- Kazmers, N.H.; Rozell, J.C.; Rumball, K.M.; Kozin, S.H.; Zlotolow, D.A.; Levin, L.S. Medial Femoral Condyle Microvascular Bone Transfer as a Treatment for Capitate Avascular Necrosis: Surgical Technique and Case Report. J. Hand Surg. Am. 2017, 42, 841.e1–841.e6. [Google Scholar] [CrossRef]
- di Summa, P.G.; Sapino, G.; Cherubino, M.; De Santis, G.; Durand, S.; Zaugg, P.; Bauquis, O.; Raffoul, W. Reconstruction of complex soft tissue defects including tendons with anterolateral thigh flap extended to fascia lata: Long term recovery and functional outcomes. Microsurgery 2019, 39, 405–415. [Google Scholar] [CrossRef]
- Hertel, R.; Masquelet, A.C. The reverse flow medial knee osteoperiosteal flap for skeletal reconstruction of the leg. Description and anatomical basis. Surg. Radiol. Anat. 1989, 11, 257–262. [Google Scholar] [CrossRef]
- Camilli, J.A.; Penteado, C.V. Bone formation by vascularized periosteal and osteoperiosteal grafts. An experimental study in rats. Arch. Orthop. Trauma Surg. 1994, 114, 18–24. [Google Scholar] [CrossRef]
- Ortak, T.; Ozdemir, R.; Uysal, A.; Ulusoy, M.G.; Sungur, N.; Sahin, B.; Kocer, U.; Sensoz, O. Osteogenic capacities of periost grafts, periost flaps and prefabricated periosteal flaps: Experimental study. J. Craniofac. Surg. 2005, 16, 594–600. [Google Scholar] [CrossRef]
- Gallardo-Calero, I.; Barrera-Ochoa, S.; Manzanares, M.C.; Sallent, A.; Vicente, M.; Lopez-Fernandez, A.; De Albert, M.; Aguirre, M.; Soldado, F.; Velez, R. Vascularized Periosteal Flaps Accelerate Osteointegration and Revascularization of Allografts in Rats. Clin. Orthop. Relat. Res. 2019, 477, 741–755. [Google Scholar] [CrossRef]
- Vegas, M.R.; Delgado, P.; Roger, I.; Carosini, R. Vascularized periosteal transfer from the medial femoral condyle: Is it compulsory to include the cortical bone? J. Trauma Acute Care Surg. 2012, 72, 1040–1045. [Google Scholar] [CrossRef]
- Masquelet, A.C.; Begue, T. The concept of induced membrane for reconstruction of long bone defects. Orthop. Clin. N. Am. 2010, 41, 27–37. [Google Scholar] [CrossRef]
- Masquelet, A.C.; Fitoussi, F.; Begue, T.; Muller, G.P. Reconstruction of the long bones by the induced membrane and spongy autograft. Ann. Chir. Plast. Esthet. 2000, 45, 346–353. [Google Scholar]
- Christen, T.; Krahenbuhl, S.M.; Muller, C.T.; Durand, S. Periosteal medial femoral condyle free flap for metacarpal nonunion. Microsurgery 2022, 42, 226–230. [Google Scholar] [CrossRef]
- Thompson, E.M.; Matsiko, A.; Farrell, E.; Kelly, D.J.; O’Brien, F.J. Recapitulating endochondral ossification: A promising route to in vivo bone regeneration. J. Tissue Eng. Regen. Med. 2015, 9, 889–902. [Google Scholar] [CrossRef]
- Soldado, F.; Knorr, J.; Haddad, S.; Corona, P.S.; Barrera-Ochoa, S.; Collado, D.; Mascarenhas, V.V.; de Gauzy, J.S. Vascularized tibial periosteal graft in complex cases of bone nonunion in children. Microsurgery 2015, 35, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Soldado, F.; Barrera-Ochoa, S.; Bergua-Domingo, J.M.; Domenech, P.; Corona, P.S.; Knorr, J. Bone nonunion management in children with a vascularized tibial periosteal graft. Microsurgery 2020, 40, 760–765. [Google Scholar] [CrossRef] [PubMed]
- Mehio, G.; Morsy, M.; Cayci, C.; Sabbagh, M.D.; Shin, A.Y.; Bishop, A.T.; Moran, S.L.; Carlsen, B.T. Donor-Site Morbidity and Functional Status following Medial Femoral Condyle Flap Harvest. Plast. Reconstr. Surg. 2018, 142, 734e–741e. [Google Scholar] [CrossRef] [PubMed]
- Weitgasser, L.; Cotofana, S.; Winkler, M.; Buerger, H.; Jamnig, D.; Anderhuber, F.; Gaggl, A. Detailed vascular anatomy of the medial femoral condyle and the significance of its use as a free flap. J. Plast. Reconstr. Aesthet. Surg. 2016, 69, 1683–1689. [Google Scholar] [CrossRef]
- Ziegler, T.; Kamolz, L.P.; Vasilyeva, A.; Schintler, M.; Neuwirth, M.; Parvizi, D. Descending genicular artery. Branching patterns and measuring parameters: A systematic review and meta-analysis of several anatomical studies. J. Plast. Reconstr. Aesthet. Surg. 2018, 71, 967–975. [Google Scholar] [CrossRef]

| Pt | Anatomic Region | Initial Accident | Active Problem | Bone Defect | Bone Flap | Skin Flap | Skin Flap Size (cm) | Flap Anastomosis | Bone Fixation | Complications | Follow-Up (Months) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Ankle | Open fracture | Framework infection and acute OM | Monocortical 4 cm | Periosteal MFC flap | SFAP flap | 15 × 6 | Single flaps | Periosteal coverage of the bone gap | Secondary arthodesis | 18 |
| 2 | Ankle | Chronic OM | Bone gap following debridement | Monocortical 6 cm | Periosteal MFC flap | DIEP flap | 29 × 13 | Single flaps | Periosteal coverage the bone gap | None | 12 |
| 3 | Foot | Chronic OM | Bone gap following debridement | Monocortical 3 cm | Periosteal MFC flap | ALT flap | 20 × 6 | Sequential flaps | Periosteal coverage the bone gap | Arterial Thrombosis and reanastomosis | 8 |
| 4 | Leg | Open fracture | Bone and skin gap | Monocortical 4 cm | Bone MFC flap | ALT flap | 21 × 7 | Sequential flaps | Plate and screws | None | 10 |
| 5 | Leg | Open fracture | Bone and skin gap | Circulare 1.5 cm | Bone MFC flap | ALT flap | 15 × 6 | Sequential flaps | Plate and k-wire | None | 6 |
| 6 | Foot | Chronic OM | Bone and skin gap | Circulare 1.5 cm | Bone MFC flap | ALT flap | 25 × 8 | Sequential flaps | Plate | None | 23 |
| 7 | Foot | Open fracture | Bone and skin gap | Monocortical 4 cm | Bone MFC flap | ALT flap | 26 × 8 | Sequential flaps | Screws | None | 6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
di Summa, P.G.; Sapino, G.; Wagner, D.; Maruccia, M.; Guillier, D.; Burger, H. Combined Free Flaps for Optimal Orthoplastic Lower Limb Reconstruction: A Retrospective Series. Medicina 2023, 59, 859. https://doi.org/10.3390/medicina59050859
di Summa PG, Sapino G, Wagner D, Maruccia M, Guillier D, Burger H. Combined Free Flaps for Optimal Orthoplastic Lower Limb Reconstruction: A Retrospective Series. Medicina. 2023; 59(5):859. https://doi.org/10.3390/medicina59050859
Chicago/Turabian Styledi Summa, Pietro G., Gianluca Sapino, Daniel Wagner, Michele Maruccia, David Guillier, and Heinz Burger. 2023. "Combined Free Flaps for Optimal Orthoplastic Lower Limb Reconstruction: A Retrospective Series" Medicina 59, no. 5: 859. https://doi.org/10.3390/medicina59050859
APA Styledi Summa, P. G., Sapino, G., Wagner, D., Maruccia, M., Guillier, D., & Burger, H. (2023). Combined Free Flaps for Optimal Orthoplastic Lower Limb Reconstruction: A Retrospective Series. Medicina, 59(5), 859. https://doi.org/10.3390/medicina59050859








