The Mid-Upper Arm Circumference as a Substitute for Body Mass Index in the Assessment of Nutritional Status among Pregnant Women: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
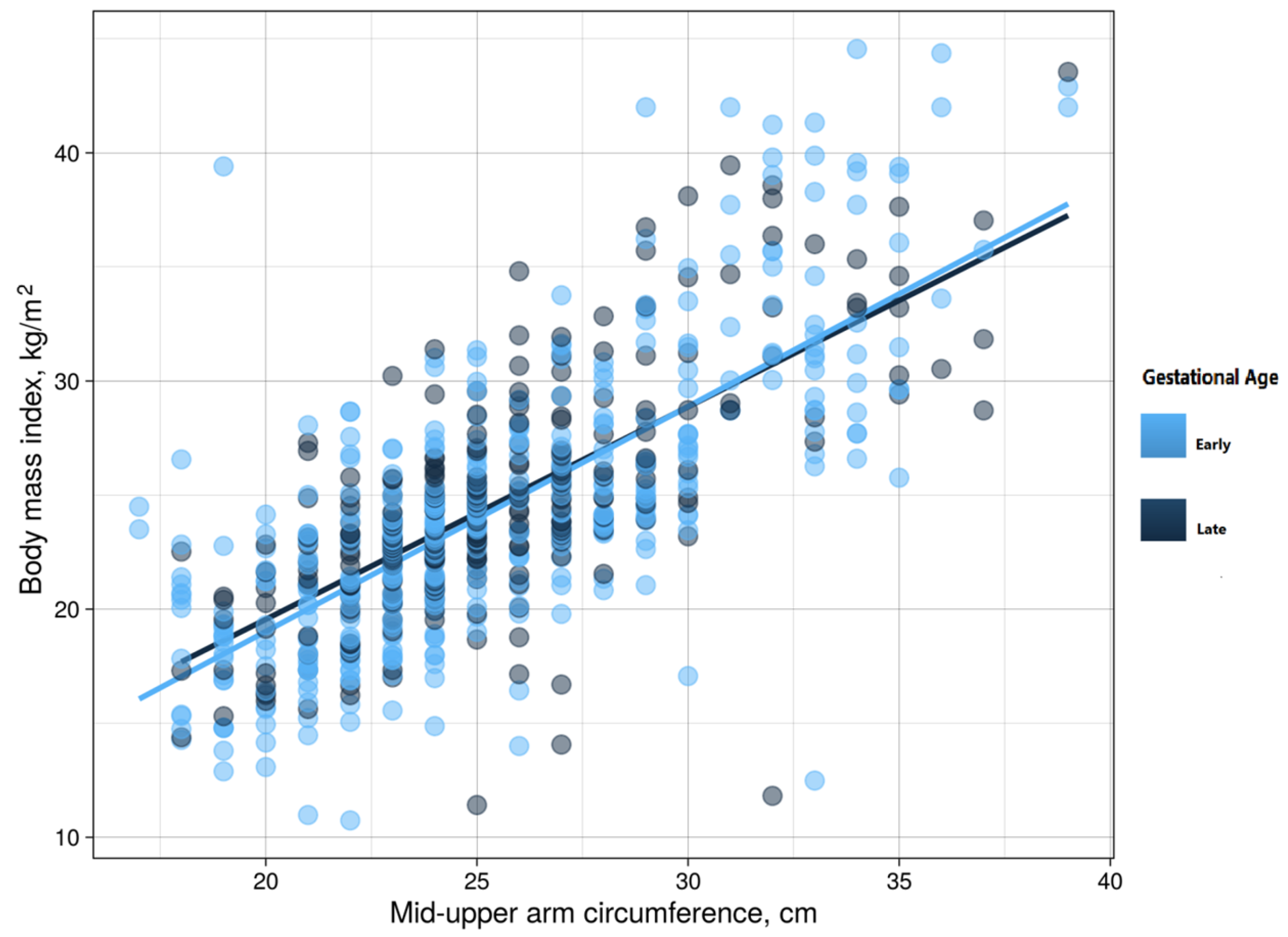
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Black, R.E.; Allen, L.H.; Bhutta, Z.A.; Caulfield, L.E.; De Onis, M.; Ezzati, M.; Mathers, C.; Rivera, J.; Maternal and Child Undernutrition Study Group. Maternal and child undernutrition: Global and regional exposures and health consequences. Lancet 2008, 371, 243–260. [Google Scholar] [CrossRef]
- WHO. Recommendations on Interventions to Improve Preterm Birth Outcomes; World Health Organization: Geneva, Switzerland, 2015; ISBN 9789241508988. [Google Scholar]
- Miele, M.J.; Souza, R.T.; Calderon, I.M.; Feitosa, F.E.; Leite, D.F.; Rocha Filho, E.A.; Vettorazzi, J.; Mayrink, J.; Fernandes, K.G.; Vieira, M.C.; et al. Maternal Nutrition Status Associated with Pregnancy-Related Adverse Outcomes. Nutrients 2021, 13, 2398. [Google Scholar] [CrossRef]
- Bailey, K.V.; Ferro-Luzzi, A. Use of body mass index of adults in assessing individual and community nutritional status. Bull. World Health Organ. 1995, 73, 673–680. [Google Scholar] [PubMed]
- Nuttall, F.Q. Body Mass Index. Nutr. Today 2015, 50, 117–128. [Google Scholar] [CrossRef]
- Musa, I.R.; Omar, S.M.; Adam, I. Mid-upper arm circumference as a substitute for body mass index in the assessment of nutritional status among adults in eastern Sudan. BMC Public Health 2022, 22, 2056. [Google Scholar] [CrossRef]
- Kesari, A.; Noel, J.Y. Nutritional Assessment; StatPearls: Orlando, FL, USA, 2022. [Google Scholar]
- Sultana, T.; Karim, M.N.; Ahmed, T.; Hossain, M.I. Assessment of Under Nutrition of Bangladeshi Adults Using Anthropometry: Can Body Mass Index Be Replaced by Mid-Upper-Arm-Circumference? PLoS ONE 2015, 10, e0121456. [Google Scholar] [CrossRef]
- Eleraky, L.; Issa, R.; Maciel, S.; Mbwana, H.; Rybak, C.; Frank, J.; Stuetz, W. High Prevalence of Overweight and Its Association with Mid-Upper Arm Circumference among Female and Male Farmers in Tanzania and Mozambique. Int. J. Environ. Res. Public Health 2021, 18, 9128. [Google Scholar] [CrossRef]
- Fakier, A.; ChB, M.; Petro, G.; Fawcus, S. Mid-upper arm circumference: A surrogate for body mass index in pregnant women. S. Afr. Med. J. 2017, 107, 606–610. [Google Scholar] [CrossRef]
- Miele, M.J.; Souza, R.T.; Calderon, I.; Feitosa, F.; Leite, D.F.; Filho, E.R.; Vettorazzi, J.; Mayrink, J.; Fernandes, K.G.; Vieira, M.C.; et al. Proposal of MUAC as a fast tool to monitor pregnancy nutritional status: Results from a cohort study in Brazil. BMJ Open 2021, 11, e047463. [Google Scholar] [CrossRef]
- Rayis, D.A.; Abbaker, A.O.; Salih, Y.; Diab, T.E.; Adam, I. Epidemiology of underweight and overweight-obesity among term pregnant Sudanese women. BMC Res. Notes 2010, 3, 327. [Google Scholar] [CrossRef]
- Hassan, B.; Rayis, D.A.; Ahmed, A.B.A.; Alhabardi, N.; Adam, I. Prevalence and associated factors of undernutrition among pregnant Sudanese women. Trans. R. Soc. Trop. Med. Hyg. 2021, 116, 352–358. [Google Scholar] [CrossRef]
- Rayis, D.A.; Abbaker, A.O.; Salih, Y.; Adam, I. Obesity and pregnancy outcome in Khartoum, Sudan. Int. J. Gynecol. Obstet. 2011, 113, 160–161. [Google Scholar] [CrossRef]
- Bilal, J.A.; Rayis, D.A.; AlEed, A.; Al-Nafeesah, A.; Adam, I. Maternal Undernutrition and Low Birth Weight in a Tertiary Hospital in Sudan: A Cross-Sectional Study. Front. Pediatr. 2022, 10, 927518. [Google Scholar] [CrossRef]
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. Ann. Intern. Med. 2007, 147, 1500–1524. [Google Scholar] [CrossRef]
- Bujang, M.A.; Baharum, N. Sample Size Guideline for Correlation Analysis. World J. Soc. Sci. Res. 2016, 3, 37–46. [Google Scholar] [CrossRef]
- Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation. Available online: https://apps.who.int/iris/handle/10665/42330 (accessed on 25 May 2022).
- Hughes, G. Youden’s Index and the Weight of Evidence Revisited. Methods Inf. Med. 2015, 54, 576–577. [Google Scholar] [CrossRef]
- Cooley, S.M.; Donnelly, J.C.; Walsh, T.; Durnea, U.; Collins, C.; Rodeck, C.H.; Hindmarsh, P.C.; Geary, M.P. The relationship between body mass index and mid-arm circumference in a pregnant population. J. Obstet. Gynaecol. 2011, 31, 594–596. [Google Scholar] [CrossRef]
- Khadivzadeh, T. Mid upper arm and calf circumferences as indicators of nutritional status in women of reproductive age. East. Mediterr. Health J. 2002, 8, 612–618. [Google Scholar] [CrossRef]
- Kumar, P.; Sareen, N.; Agrawal, S.; Kathuria, N.; Yadav, S.; Sethi, V. Screening Maternal Acute Malnutrition Using Adult Mid-Upper Arm Circumference in Resource-Poor Settings. Indian J. Community Med. 2018, 43, 132–134. [Google Scholar] [CrossRef]
- Assefa, N.; Berhane, Y.; Worku, A. Wealth Status, Mid Upper Arm Circumference (MUAC) and Antenatal Care (ANC) Are Determinants for Low Birth Weight in Kersa, Ethiopia. PLoS ONE 2012, 7, e39957. [Google Scholar] [CrossRef]
- Sethi, V.; Parhi, R.N.; Dar, S.; Agrawal, S. Feasibility and diagnostic accuracy of using armband mid-upper arm circumference as a simple screening tool for maternal wasting in rural India. Rural Remote Health 2017, 17, 4221. [Google Scholar] [CrossRef] [PubMed]

| Variables | Total (n = 688) | Women in Early Pregnancy (n = 437) | Women in Late Pregnancy (n = 251) | p-Value |
|---|---|---|---|---|
| Age, years | 26.0 (15.0–37.0) | 26.0 (20.0–31.0) | 26.0(21.0–30.0) | 0.574 |
| Parity | 3 (0–6) | 3 (1–4) | 3 (1–4) | 0.875 |
| Body mass index, kg/m2 | 23.8 (17.7–29.9) | 23.6 (20.5–27.1) | 24.0(21.5–26.9) | 0.157 |
| Mid-upper arm circumference, cm | 25.0 (19.0–31.0) | 24.0 (22.0–28.0) | 25.0(23.0–27.0) | 0.393 |
| Gestational age, weeks | 17.0 (8.0–26.0) | 13.0 (10.0–17.0) | 23.0(21.0–30.0) | <0.001 |
| Variables | Early Pregnancy | Late Pregnancy | |
|---|---|---|---|
| Underweight | The area under the receiver operating characteristic curve | 0.83 | 0.81 |
| Cut-off | 24.0 cm | 23.0 cm | |
| Sensitivity | 71.0 | 85.0 | |
| Specificity | 86.0 | 72.0 | |
| Positive predictive value | 97.0 | 96.0 | |
| Negative predictive value | 34.0 | 34.0 | |
| Youden’s index | 0.57 | 0.57 | |
| Obesity | The area under the receiver operating characteristic curve | 0.90 | 0.88 |
| Cut-off | 29.0 cm | 28.0 cm | |
| Sensitivity | 80.0 | 76.0 | |
| Specificity | 87.0 | 86.0 | |
| Positive predictive value | 51.0 | 47.0 | |
| Negative predictive value | 96.0 | 95.0 | |
| Youden’s index | 0.67 | 0.61 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salih, Y.; Omar, S.M.; AlHabardi, N.; Adam, I. The Mid-Upper Arm Circumference as a Substitute for Body Mass Index in the Assessment of Nutritional Status among Pregnant Women: A Cross-Sectional Study. Medicina 2023, 59, 1001. https://doi.org/10.3390/medicina59061001
Salih Y, Omar SM, AlHabardi N, Adam I. The Mid-Upper Arm Circumference as a Substitute for Body Mass Index in the Assessment of Nutritional Status among Pregnant Women: A Cross-Sectional Study. Medicina. 2023; 59(6):1001. https://doi.org/10.3390/medicina59061001
Chicago/Turabian StyleSalih, Yasir, Saeed M. Omar, Nadiah AlHabardi, and Ishag Adam. 2023. "The Mid-Upper Arm Circumference as a Substitute for Body Mass Index in the Assessment of Nutritional Status among Pregnant Women: A Cross-Sectional Study" Medicina 59, no. 6: 1001. https://doi.org/10.3390/medicina59061001
APA StyleSalih, Y., Omar, S. M., AlHabardi, N., & Adam, I. (2023). The Mid-Upper Arm Circumference as a Substitute for Body Mass Index in the Assessment of Nutritional Status among Pregnant Women: A Cross-Sectional Study. Medicina, 59(6), 1001. https://doi.org/10.3390/medicina59061001






