Anatomical Variants of Internal Carotid Artery—Results from a Retrospective Study
Abstract
:1. Introduction
2. Materials and Methods
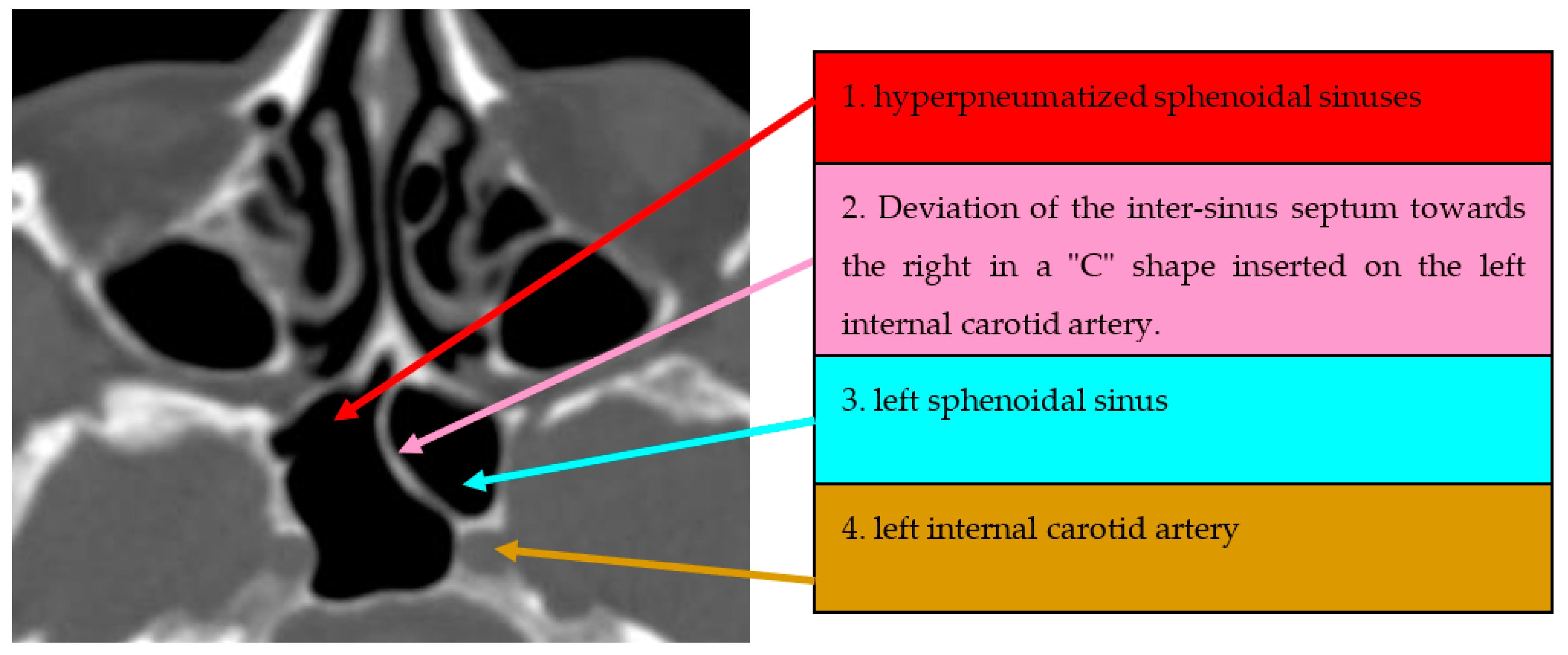
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mokhasanavisu, V.J.P.; Singh, R.; Balakrishnan, R.; Kadavigere, R. Ethnic Variation of Sinonasal Anatomy on CT Scan and Volumetric Analysis. Indian J. Otolaryngol. Head Neck Surg. 2019, 71 (Suppl. S3), 2157–2164. [Google Scholar] [CrossRef] [PubMed]
- Al-Abri, R.; Bhargava, D.; Al-Bassam, W.; Al-Badaai, Y.; Sawhney, S. Clinically significant anatomical variants of the paranasal sinuses. Oman Med. J. 2014, 29, 110–113. [Google Scholar] [CrossRef] [PubMed]
- Homsi, M.T.; Gaffey, M.M. Sinus Endoscopic Surgery; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Thejas, S.R.; Prashanth, N.; Yogesh, T.; Nilavan, S.; Raj, M.R.; Vipanchi, S. Symptomatic assessment in patients undergoing full-house functional endoscopic sinus surgery for pansinusitis using nonpowered instruments through the Sinonasal Outcome Test-22 Questionnaire in the rural population. MRIMS J. Health Sci. 2023; ahead of print. [Google Scholar]
- Lien, C.F.; Weng, H.H.; Chang, Y.C.; Lin, Y.C.; Wang, W.H. Computed tomographic analysis of frontal recess anatomy and its effect on the development of frontal sinusitis. Laryngoscope 2010, 120, 2521–2527. [Google Scholar] [CrossRef] [PubMed]
- Keast, A.; Yelavich, S.; Dawes, P.; Lyons, B. Anatomical variations of the paranasal sinuses in Polynesian and New Zealand European computerized tomography scans. Otolaryngol. Head Neck Surg. 2008, 139, 216–221. [Google Scholar] [CrossRef]
- Haussen, D.C.; Jadhav, A.; Rebello, L.C.; Belagaje, S.; Anderson, A.; Jovin, T.; Aghaebrahim, A.; Gulati, D.; Wells, B.; Frankel, M.; et al. Internal Carotid Artery S-Shaped Curve as a Marker of Fibromuscular Dysplasia in Dissection-Related Acute Ischemic Stroke. Interv. Neurol. 2016, 5, 185–192. [Google Scholar] [CrossRef]
- Kang, Y.J.; Cho, J.H.; Kim, D.H.; Kim, S.W. Relationships of sphenoid sinus pneumatization with internal carotid artery characteristics. PLoS ONE 2022, 17, e0273545. [Google Scholar] [CrossRef]
- Badran, K.; Tarifi, A.; Shatarat, A.; Badran, D. Sphenoid sinus pneumatization: The good, the bad, and the beautiful. Eur. Arch. Otorhinolaryngol. 2022, 279, 4435–4441. [Google Scholar] [CrossRef]
- Famurewa, O.C.; Ibitoye, B.O.; Ameye, S.A.; Asaleye, C.M.; Ayoola, O.O.; Onigbinde, O.S. Sphenoid Sinus Pneumatization, Septation, and the Internal Carotid Artery: A Computed Tomography Study. Niger. Med. J. 2018, 59, 7–13. [Google Scholar] [CrossRef]
- Sumaily, I.; Alarifi, I.; Alahmari, A.; Aloulah, M.; Alsaleh, S. Sphenoid Sinus Involvement in Chronic Rhinosinusitis Without Polyps. Allergy Rhinol. 2020, 11, 2152656720934472. [Google Scholar] [CrossRef]
- Jaworek-Troć, J.; Ochwat, K.; Walocha, J.A.; Zamojska, I.; Lipski, M.; Żytkowski, A.; Chrzan, R.; Zawiliński, J.; Ghosh, S.K.; Zarzecki, M.P. Prevalence of the Onodi cell in the Polish adult population: An anatomical computed tomography study. Folia Morphol. 2023. [Google Scholar] [CrossRef]
- Dal Secchi, M.M.; Dolci, R.L.L.; Teixeira, R.; Lazarini, P.R. An Analysis of Anatomic Variations of the Sphenoid Sinus and Its Relationship to the Internal Carotid Artery. Int. Arch. Otorhinolaryngol. 2018, 22, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Lum, S.G.; Gendeh, B.S.; Husain, S.; Gendeh, H.S.; Ismail, M.R.; Toh, C.J.; Izaham, A.; Tan, H.J. Internal carotid artery injury during endonasal sinus surgery: Our experience and review of the literature. Acta Otorhinolaryngol. Ital. 2019, 39, 130–136. [Google Scholar] [CrossRef] [PubMed]
- Aibar-Durán, J.; Muñoz-Hernández, F.; Asencio-Cortés, C.; Montserrat-Gili, J.; Gras-Cabrerizo, J.R.; Mirapeix, R.M. Intracavernous Branches of the Internal Carotid Artery Through an Endoscopic Endonasal Approach: Anatomical Study and Review of the Literature. World Neurosurg 2021, 151, e332–e342. [Google Scholar] [CrossRef] [PubMed]
- Dziedzic, T.; Koczyk, K.; Gotlib, T.; Kunert, P.; Maj, E.; Marchel, A. Sphenoid sinus septations and their interconnections with parasphenoidal internal carotid artery protuberance: Radioanatomical study with literature review. Wideochirurgia Inne Tech. Maloinwazyjne 2020, 15, 227–233. [Google Scholar] [CrossRef] [PubMed]
- Ngubane, N.P.; Lazarus, L.; Rennie, C.O.; Satyapal, K.S. The Septation of the Sphenoidal Air Sinus. A Cadaveric Study. Int. J. Morphol. 2018, 36, 1413–1422. [Google Scholar] [CrossRef]
- Refaat, R.; Basha, M.A.A. The impact of sphenoid sinus pneumatization type on the protrusion and dehiscence of the adjacent neurovascular structures: A prospective MDCT imaging study. Acad. Radiol. 2020, 27, e132–e139. [Google Scholar] [CrossRef]
- Rereddy, S.K.; Johnson, D.M.; Wise, S.K. Markers of Increased Aeration in the Paranasal Sinuses and Along the Skull Base: Association between Anatomic Variants. Am. J. Rhinol. Allergy 2014, 28, 477–482. [Google Scholar] [CrossRef]
- Abdullah, B.; Arasaratnam, S.; Kumar, G.; Gopala, K. The sphenoid sinuses: Computed tomographic assessment of septation, relationship to the internal carotid arteries and sidewall thickness in the Malaysian population. J. HK Coll. Radiol. 2001, 4, 185–188. [Google Scholar]
- Lantos, J.E.; Pearlman, A.N.; Gupta, A.; Chazen, J.L.; Zimmerman, R.D.; Shatzkes, D.R.; Phillips, C.D. Protrusion of the Infraorbital Nerve into the Maxillary Sinus on CT: Prevalence, Proposed Grading Method, and Suggested Clinical Implications. AJNR Am. J. Neuroradiol. 2016, 37, 349–353. [Google Scholar] [CrossRef]
- Nitinavakarn, B.; Thanaviratananich, S.; Sangsilp, N. Anatomical variations of the lateral nasal wall and paranasal sinuses: A CT study for endoscopic sinus surgery (ESS) in Thai patients. J. Med. Assoc. Thai. 2005, 88, 763–768. [Google Scholar]
- Fernandez-Miranda, J.C.; Prevedello, D.M.; Madhok, R.; Morera, V.; Barges-Coll, J.; Reineman, K.; Snyderman, C.H.; Gardner, P.; Carrau, R.; Kassam, A.B. Sphenoid septations and their relationship with internal carotid arteries: Anatomical and radiological study. Laryngoscope 2009, 119, 1893–1896. [Google Scholar] [CrossRef]
- Gibelli, D.; Cellina, M.; Gibelli, S.; Cappella, A.; Oliva, A.G.; Termine, G.; Sforza, C. Relationship between sphenoid sinus volume and accessory septations: A 3D assessment of risky anatomical variants for endoscopic surgery. Anat. Rec. 2020, 303, 1300–1304. [Google Scholar] [CrossRef]
- Reittner, P.; Doerfler, O.; Goritsching, T.; Tillich, M.; Koele, W.; Stammberger, H.; Szolar, D.H. Magnetic resonance imaging patterns of the development of the sphenoid sinus: A review of 800 patients. Rhinology 2001, 39, 121–124. [Google Scholar]
- Mehendale, N.H.; Marple, B.F.; Nussenbaum, B. Management of sphenoid sinus cerebrospinal fluid rhinorrhea: Making use of an extended approach to the sphenoid sinus. Otolaryngol. Head Neck Surg 2002, 126, 147–153. [Google Scholar] [CrossRef]
- Unal, B.; Bademci, G.; Bilgili, Y.K.; Batay, F.; Avci, E. Risky anatomic variations of sphenoid sinus for surgery. Surg. Radiol. Anat. 2006, 28, 195–201. [Google Scholar] [CrossRef]
- Sasagawa, Y.; Tachibana, O.; Doai, M.; Hayashi, Y.; Tonami, H.; Iizuka, H.; Nakada, M. Carotid artery protrusion and dehiscence in patients with acromegaly. Pituitary 2016, 19, 482–487. [Google Scholar] [CrossRef]
- Tomovic, S.; Esmaeili, A.; Chan, N.J.; Shukla, P.A.; Choudhry, O.J.; Liu, J.K.; Eloy, J.A. High-resolution computed tomography analysis of variations of the sphenoid sinus. J. Neurol. Surg. Part B Skull Base 2013, 74, 82–90. [Google Scholar] [CrossRef]
- Raseman, J.; Guryildirim, M.; Beer-Furlan, A.; Jhaveri, M.; Tajudeen, B.A.; Byrne, R.W.; Batra, P.S. Preoperative Computed Tomography Imaging of the Sphenoid Sinus: Striving Towards Safe Transsphenoidal Surgery. J. Neurol. Surg. Part B Skull Base 2020, 81, 251–262. [Google Scholar] [CrossRef]
- Schutt, C.; Dissanaike, S.; Marchbanks, J. Case Report: Inadvertent Carotid Artery Injury during Myringotomy as a Result of Carotid Artery Dehiscence. Ear Nose Throat J. 2013, 92, E35–E37. [Google Scholar] [CrossRef]
- Moeller, C.W.; Welch, K.C. Prevention and management of complications in sphenoidotomy. Otolaryngol. Clin. N. Am. 2010, 43, 839–854. [Google Scholar] [CrossRef]
- Fadda, G.L.; Petrelli, A.; Urbanelli, A.; Castelnuovo, P.; Bignami, M.; Crosetti, E.; Succo, G.; Cavallo, G. Risky anatomical variations of sphenoid sinus and surrounding structures in endoscopic sinus surgery. Head Face Med. 2022, 18, 29. [Google Scholar] [CrossRef] [PubMed]
- Gardner, P.A.; Snyderman, C.H.; Wang, E.W.; Fernandez-Miranda, J.C. 36—Complications of Endoscopic Endonasal Skull Base Surgery. In Complications in Neurosurgery; Nanda, A., Ed.; Elsevier: London, UK, 2019; pp. 207–212. [Google Scholar] [CrossRef]
- Weidenbecher, M.; Huk, W.J.; Iro, H. Internal carotid artery injury during functional endoscopic sinus surgery and its management. Eur. Arch. Otorhinolaryngol. 2005, 262, 640–645. [Google Scholar] [CrossRef] [PubMed]




| Demographic Characteristics | ICA at Distance from SS | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Yes (n = 81) | No (n = 69) | p Value | Bilateral (n = 36) | Unilateral (n = 45) | p Value | Left (n = 30) | Right (n = 15) | p Value | |
| Age, years (mean and standard deviation) | 53.75 ± 18.87 | 53.20 ± 14.93 | 0.84 | 52.11 ± 18.79 | 55.07 ± 19.05 | 0.73 | 60.27 ± 15.87 | 64.67 ± 21.71 | 0.31 |
| Gender (n/%) | Male = 34 (42%) Female = 47 (58%) | Male = 34 (49.3%) Female = 35 (50.7%) | 0.37 | Male = 16 (44.4%) Female = 20 (55.6%) | Male = 18 (40.0%) Female = 27 (60%) | 0.61 | Male = 13 (43.3%) Female = 17 (56.7%) | Male = 5 (33.3%) Female = 10 (66.7%) | 0.56 |
| Medium (n/%) | Urban = 36 (44.4%) Rural = 45 (55.6%) | Urban = 32 (46.4%) Rural = 37 (53.6%) | 0.81 | Urban = 17 (47.2%) Rural = 19 (52.8%) | Urban = 19 (42.2%) Rural = 26 (57.8%) | 0.87 | Urban = 10 (33.3%) Rural = 20 (66.7%) | Urban = 9 (60%) Rural = 6 (40%) | 0.21 |
| Demographic Characteristics | Procident ICA | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Yes (n = 87) | No (n = 63) | p Value | Bilateral (n = 48) | Unilateral (n = 42) | p Value | Left (n = 21) | Right (n = 21) | p Value | |
| Age, years (mean and standard deviation) | 60.90 ± 15.85 | 56.25 ± 17.43 | 0.10 | 62.46 ± 15.46 | 59.57 ± 16.08 | 0.13 | 60.27 ± 15.87 | 64.67 ± 21.71 | 0.31 |
| Gender (n/%) | Male = 36 (41.4%) Female = 51 (58.6%) | Male = 30 (47.6%) Female = 33 (52.4%) | 0.44 | Male = 18 (37.5%) Female = 30 (62.5%) | Male = 20 (47.6%) Female = 22 (52.4%) | 0.54 | Male = 9 (42.9%) Female = 12 (57.1%) | Male = 11 (52.4%) Female = 10 (47.6%) | 0.70 |
| Medium (n/%) | Urban = 36 (41.4%) Rural = 51 (58.6%) | Urban = 28 (44.4%) Rural = 35 (55.6%) | 0.70 | Urban = 14 (29.2%) Rural = 34 (70.8%) | Urban = 23 (54.8%) Rural = 19 (45.2%) | 0.05 | Urban = 15 (71.4%) Rural = 6 (28.6%) | Urban = 8 (38.1%) Rural = 13 (61.9%) | 0.016 |
| Demographic Characteristics | Dehiscent ICA | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Yes (n = 78) | No (n = 72) | p Value | Bilateral (n = 24) | Unilateral (n = 54) | p Value | Left (n = 27) | Right (n = 27) | p Value | |
| Age, years (mean and standard deviation) | 54.83 ± 16.50 | 54.97 ± 14.77 | 0.95 | 50.79 ± 18.80 | 56.63 ± 15.22 | 0.31 | 53.11 ± 15.54 | 60.15 ± 14.31 | 0.15 |
| Gender (n/%) | Male = 29 (37.2%) Female = 49 (62.8%) | Male = 28 (38.9%) Female = 44 (61.1%) | 0.82 | Male = 8 (33.3%) Female = 16 (66.7%) | Male = 21 (38.9%) Female = 33 (61.1%) | 0.87 | Male = 10 (37%) Female = 17 (63%) | Male = 11 (40.7%) Female = 16 (59.3%) | 0.94 |
| Medium (n/%) | Urban = 40 (51.3%) Rural = 38 (48.7%) | Urban = 33 (45.8%) Rural = 39 (54.2%) | 0.50 | Urban = 13 (54.2%) Rural = 11 (45.8%) | Urban = 27 (50%) Rural = 27 (50%) | 0.75 | Urban = 14 (51.9%) Rural = 13 (48.1%) | Urban = 13 (48.1%) Rural = 14 (51.9%) | 0.93 |
| Demographic Characteristics | Intrasinusal Septa with Posterior Insertion on Internal Carotid Artery | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Yes (n = 88) | No (n = 62) | p Value | Bilateral (n = 27) | Unilateral (n = 66) | p Value | Left (n = 42) | Right (n = 24) | p Value | |
| Age, years (mean and standard deviation) | 57.09 ± 14.53 | 55.84 ± 15.33 | 0.12 | 55.85 ± 13.32 | 56.92 ± 14.98 | 0.08 | 53.11 ± 15.54 | 57.64 ± 14.23 | 0.19 |
| Gender (n/%) | Male = 23 (26.1%) Female = 65 (73.89%) | Male = 19 (30.6%) Female = 43 (69.4%) | 0.54 | Male = 7 (25.9%) Female = 20 (74.1%) | Male = 18 (27.3%) Female = 48 (72.7%) | 0.91 | Male = 12 (28.6%) Female = 30 (71.4%) | Male = 6 (25%) Female = 18 (75%) | 0.93 |
| Medium (n/%) | Urban = 53 (60.2%) Rural = 35 (39.8%) | Urban = 34 (54.8%) Rural = 28 (45.2%) | 0.51 | Urban = 20 (74.1%) Rural = 7 (25.9%) | Urban = 38 (57.6%) Rural = 28 (42.4%) | 0.13 | Urban = 23 (54.8%) Rural = 19 (45.2%) | Urban = 15 (62.5%) Rural = 9 (37.5%) | 0.82 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cobzeanu, B.M.; Baldea, V.; Costan, V.V.; Cobzeanu, M.D.; Palade, O.D.; Gheorghe, L.; Radulescu, L.; Severin, F.; Lupascu Ursulescu, C.; Bandol, G.; et al. Anatomical Variants of Internal Carotid Artery—Results from a Retrospective Study. Medicina 2023, 59, 1057. https://doi.org/10.3390/medicina59061057
Cobzeanu BM, Baldea V, Costan VV, Cobzeanu MD, Palade OD, Gheorghe L, Radulescu L, Severin F, Lupascu Ursulescu C, Bandol G, et al. Anatomical Variants of Internal Carotid Artery—Results from a Retrospective Study. Medicina. 2023; 59(6):1057. https://doi.org/10.3390/medicina59061057
Chicago/Turabian StyleCobzeanu, Bogdan Mihail, Vasilica Baldea, Victor Vlad Costan, Mihail Dan Cobzeanu, Octavian Dragos Palade, Liliana Gheorghe, Luminita Radulescu, Florentina Severin, Corina Lupascu Ursulescu, Geanina Bandol, and et al. 2023. "Anatomical Variants of Internal Carotid Artery—Results from a Retrospective Study" Medicina 59, no. 6: 1057. https://doi.org/10.3390/medicina59061057
APA StyleCobzeanu, B. M., Baldea, V., Costan, V. V., Cobzeanu, M. D., Palade, O. D., Gheorghe, L., Radulescu, L., Severin, F., Lupascu Ursulescu, C., Bandol, G., Martu, C., Rosu, A. M., & Cobzeanu, M. L. (2023). Anatomical Variants of Internal Carotid Artery—Results from a Retrospective Study. Medicina, 59(6), 1057. https://doi.org/10.3390/medicina59061057








