Cenobamate (YKP3089) and Drug-Resistant Epilepsy: A Review of the Literature
Abstract
1. Introduction
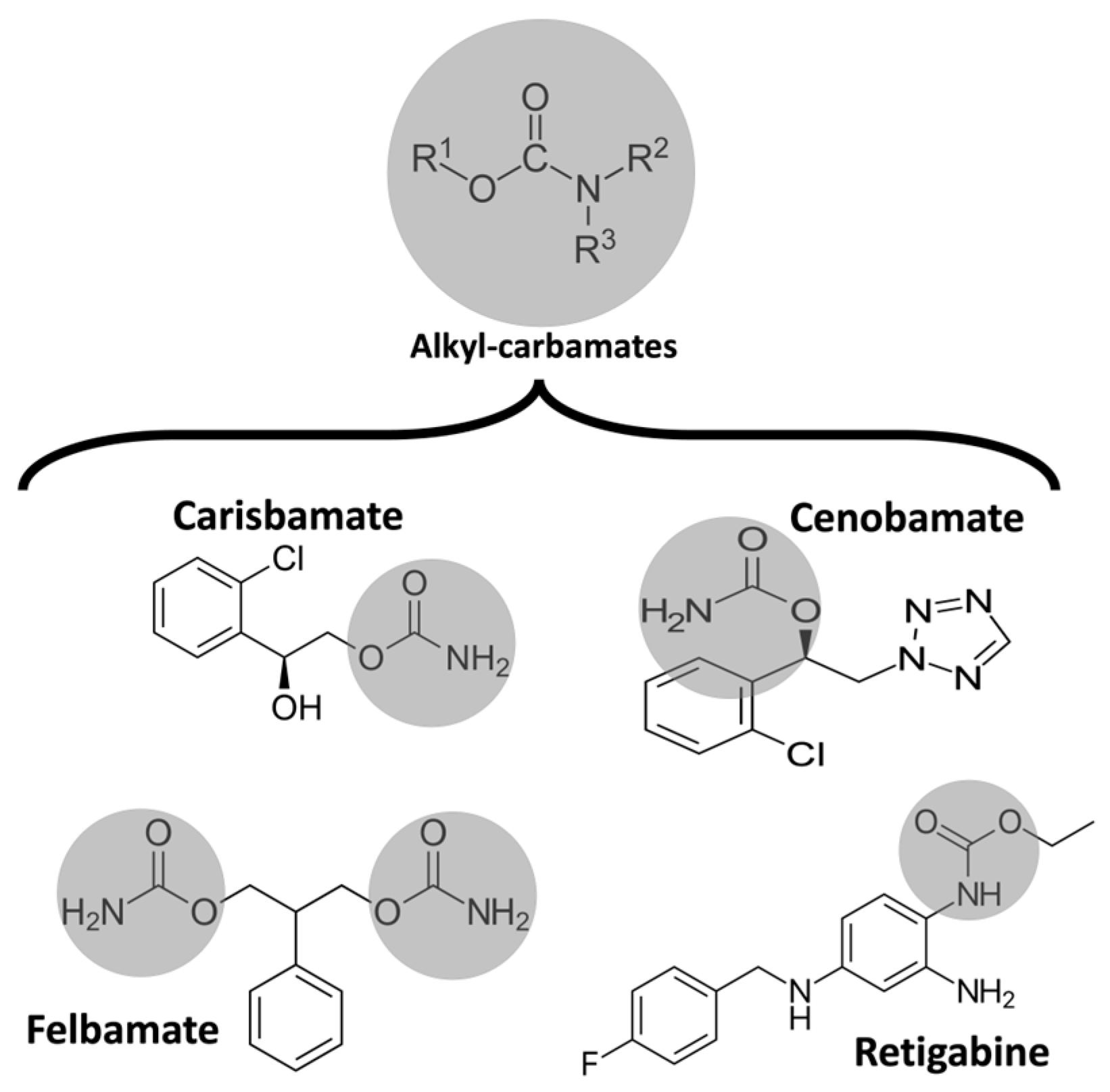
2. Historical Aspects of Cenobamate
3. Pharmacology and Mechanism of Action
4. Clinical Trials
5. Discussion
5.1. Efficacy of Cenobamate
5.2. Cost-Effectiveness of Cenobamate
5.3. Neuroprotective Potential of Cenobamate
5.4. Cognition and Cenobamate
5.5. Electrocardiographic Abnormalities Associated with Cenobamate
5.6. Hepatotoxicity Secondary to Cenobamate
5.7. Cenobamate-Induced Movement Disorders
5.8. Pregnancy and Lactation
5.9. Potential for Abuse and Suicidality Risk
6. Expert Recommendations
7. Future Perspectives
8. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- GBD 2016 Epilepsy Collaborators. Global, regional, and national burden of epilepsy, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 357–375. [Google Scholar] [CrossRef] [PubMed]
- Zack, M.M.; Kobau, R. National and State Estimates of the Numbers of Adults and Children with Active Epilepsy—United States, 2015. MMWR Morb. Mortal. Wkly. Rep. 2017, 66, 821–825. [Google Scholar] [CrossRef] [PubMed]
- Beghi, E.; Giussani, G.; Costa, C.; DiFrancesco, J.C.; Dhakar, M.; Leppik, I.; Kwan, P.; Akamatsu, N.; Cretin, B.; O’Dwyer, R.; et al. The epidemiology of epilepsy in older adults: A narrative review by the ILAE Task Force on Epilepsy in the Elderly. Epilepsia 2023, 64, 586–601. [Google Scholar] [CrossRef]
- Begley, C.E.; Durgin, T.L. The direct cost of epilepsy in the United States: A systematic review of estimates. Epilepsia 2015, 56, 1376–1387. [Google Scholar] [CrossRef]
- Guery, D.; Rheims, S. Clinical Management of Drug Resistant Epilepsy: A Review on Current Strategies. Neuropsychiatr. Dis. Treat. 2021, 17, 2229–2242. [Google Scholar] [CrossRef] [PubMed]
- Pong, A.W.; Ross, J.; Tyrlikova, I.; Giermek, A.J.; Kohli, M.P.; Khan, Y.A.; Salgado, R.D.; Klein, P. Epilepsy: Expert opinion on emerging drugs in phase 2/3 clinical trials. Expert Opin. Emerg. Drugs 2022, 27, 75–90. [Google Scholar] [CrossRef]
- Chen, Z.; Brodie, M.J.; Liew, D.; Kwan, P. Treatment Outcomes in Patients With Newly Diagnosed Epilepsy Treated With Established and New Antiepileptic Drugs: A 30-Year Longitudinal Cohort Study. JAMA Neurol. 2018, 75, 279–286. [Google Scholar] [CrossRef]
- Kwan, P.; Brodie, M.J. Early identification of refractory epilepsy. N. Engl. J. Med. 2000, 342, 314–319. [Google Scholar] [CrossRef]
- Kwan, P.; Arzimanoglou, A.; Berg, A.T.; Brodie, M.J.; Hauser, W.A.; Mathern, G.; Moshé, S.L.; Perucca, E.; Wiebe, S.; French, J. Definition of drug resistant epilepsy: Consensus proposal by the ad hoc Task Force of the ILAE Commission on Therapeutic Strategies. Epilepsia 2010, 51, 1069–1077. [Google Scholar] [CrossRef]
- Mesraoua, B.; Deleu, D.; Hassan, A.H.; Gayane, M.; Lubna, A.; Ali, M.A.; Tomson, T.; Khalil, B.A.; Cross, J.H.; Asadi-Pooya, A.A. Dramatic outcomes in epilepsy: Depression, suicide, injuries, and mortality. Curr. Med. Res. Opin. 2020, 36, 1473–1480. [Google Scholar] [CrossRef]
- Specchio, N.; Curatolo, P. Developmental and epileptic encephalopathies: What we do and do not know. Brain 2021, 144, 32–43. [Google Scholar] [CrossRef]
- Morrell, M.J. Stigma and epilepsy. Epilepsy Behav. 2002, 3, 21–25. [Google Scholar] [CrossRef] [PubMed]
- Kanner, A.M. Depression and epilepsy: A new perspective on two closely related disorders. Epilepsy Curr. 2006, 6, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Kanner, A.M.; Bicchi, M.M. Antiseizure Medications for Adults with Epilepsy: A Review. JAMA 2022, 327, 1269–1281. [Google Scholar] [CrossRef] [PubMed]
- French, J.A. Cenobamate for focal seizures—A game changer? Nat. Rev. Neurol. 2020, 16, 133–134. [Google Scholar] [CrossRef] [PubMed]
- Perucca, E.; Brodie, M.J.; Kwan, P.; Tomson, T. 30 years of second-generation antiseizure medications: Impact and future perspectives. Lancet Neurol. 2020, 19, 544–556. [Google Scholar] [CrossRef] [PubMed]
- Ungar, A.; Ceccofiglio, A.; Pescini, F.; Mussi, C.; Tava, G.; Rafanelli, M.; Langellotto, A.; Marchionni, N.; Dijk, J.G.; Galizia, G.; et al. Syncope and Epilepsy coexist in ‘possible’ and ‘drug-resistant’ epilepsy (Overlap between Epilepsy and Syncope Study—OESYS). BMC Neurol. 2017, 17, 45. [Google Scholar] [CrossRef][Green Version]
- Singh, A. Cenobamate for treatment-resistant focal seizures: Current evidence and place in therapy. J. Cent. Nerv. Syst. Dis. 2022, 14, 11795735211070209. [Google Scholar] [CrossRef]
- Janson, M.T.; Bainbridge, J.L. Continuing Burden of Refractory Epilepsy. Ann. Pharmacother. 2021, 55, 406–408. [Google Scholar] [CrossRef]
- Berg, A.T. Febrile seizures and epilepsy: The contributions of epidemiology. Paediatr. Perinat. Epidemiol. 1992, 6, 145–152. [Google Scholar] [CrossRef]
- Das, N.; Dhanawat, M.; Shrivastava, S.K. An overview on antiepileptic drugs. Drug Discov. Ther. 2012, 6, 178–193. [Google Scholar] [CrossRef] [PubMed]
- Catterall, W.A. Sodium channels, inherited epilepsy, and antiepileptic drugs. Annu. Rev. Pharmacol. Toxicol. 2014, 54, 317–338. [Google Scholar] [CrossRef] [PubMed]
- Lossin, C.; Wang, D.W.; Rhodes, T.H.; Vanoye, C.G.; George, A.L. Molecular basis of an inherited epilepsy. Neuron 2002, 34, 877–884. [Google Scholar] [CrossRef] [PubMed]
- Stafstrom, C.E. Persistent sodium current and its role in epilepsy. Epilepsy Curr. 2007, 7, 15–22. [Google Scholar] [CrossRef]
- Ramchandani, D.; López-Muñoz, F.; Alamo, C. Meprobamate-tranquilizer or anxiolytic? A historical perspective. Psychiatr. Q. 2006, 77, 43–53. [Google Scholar] [CrossRef]
- Ludwig, B.J.; Powell, L.S.; Berger, F.M. Carbamate derivatives related to meprobamate. J. Med. Chem. 1969, 12, 462–472. [Google Scholar] [CrossRef] [PubMed]
- Levy, R.; Ragueneau-Majlessi, I.; Solanki, B.; Zannikos, P.; Yao, C.; Novak, G. Pharmacokinetics, safety, and tolerability of the new antiepileptic carisbamate in the elderly. Epilepsy Res. 2008, 79, 22–30. [Google Scholar] [CrossRef]
- Sperling, M.R.; Greenspan, A.; Cramer, J.A.; Kwan, P.; Kälviäinen, R.; Halford, J.J.; Schmitt, J.; Yuen, E.; Cook, T.; Haas, M.; et al. Carisbamate as adjunctive treatment of partial onset seizures in adults in two randomized, placebo-controlled trials. Epilepsia 2010, 51, 333–343. [Google Scholar] [CrossRef]
- Zaccara, G.; Lattanzi, S.; Leo, A.; Russo, E. Critical Appraisal of Cenobamate as Adjunctive Treatment of Focal Seizures in Adults. Neuropsychiatr. Dis. Treat. 2021, 17, 3447–3457. [Google Scholar] [CrossRef]
- Bialer, M.; Johannessen, S.I.; Levy, R.H.; Perucca, E.; Tomson, T.; White, H.S. Progress report on new antiepileptic drugs: A summary of the Eleventh Eilat Conference (EILAT XI). Epilepsy Res. 2013, 103, 2–30. [Google Scholar] [CrossRef]
- Keam, S.J. Cenobamate: First Approval. Drugs 2020, 80, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Barbieri, M.A.; Perucca, E.; Spina, E.; Rota, P.; Franco, V. Cenobamate: A Review of its Pharmacological Properties, Clinical Efficacy and Tolerability Profile in the Treatment of Epilepsy. CNS Neurol. Disord. Drug Targets 2023, 22, 394–403. [Google Scholar] [CrossRef] [PubMed]
- Löscher, W.; Sills, G.J.; White, H.S. The ups and downs of alkyl-carbamates in epilepsy therapy: How does cenobamate differ? Epilepsia 2021, 62, 596–614. [Google Scholar] [CrossRef] [PubMed]
- Löscher, W.; White, H.S. Animal Models of Drug-Resistant Epilepsy as Tools for Deciphering the Cellular and Molecular Mechanisms of Pharmacoresistance and Discovering More Effective Treatments. Cells 2023, 12, 1233. [Google Scholar] [CrossRef] [PubMed]
- Guignet, M.; Campbell, A.; White, H.S. Cenobamate (XCOPRI): Can preclinical and clinical evidence provide insight into its mechanism of action? Epilepsia 2020, 61, 2329–2339. [Google Scholar] [CrossRef]
- Binnie, C.D.; Trenité, D.G.; Korte, R. Photosensitivity as a model for acute antiepileptic drug studies. Electroencephalogr. Clin. Neurophysiol. 1986, 63, 35–41. [Google Scholar] [CrossRef]
- Kasteleijn-Nolst Trenite, D.G.A.; DiVentura, B.D.; Pollard, J.R.; Krauss, G.L.; Mizne, S.; French, J.A. Suppression of the photoparoxysmal response in photosensitive epilepsy with cenobamate (YKP3089). Neurology 2019, 93, e559–e567. [Google Scholar] [CrossRef]
- Sommerfeld-Klatta, K.; Zielińska-Psuja, B.; Karaźniewcz-Łada, M.; Główka, F.K. New Methods Used in Pharmacokinetics and Therapeutic Monitoring of the First and Newer Generations of Antiepileptic Drugs (AEDs). Molecules 2020, 25, 5083. [Google Scholar] [CrossRef]
- Oh, J.H.; Jeong, J.W.; Ji, Y.G.; Shin, Y.M.; Lee, K.R.; Cho, K.H.; Koo, T.S. Development of a liquid chromatography-tandem mass spectrometry method for assaying cenobamate in rat plasma. J. Liquid. Chrom. 2019, 41, 992–997. [Google Scholar] [CrossRef]
- Vernillet, L.; Greene, S.A.; Kim, H.W.; Melnick, S.M.; Glenn, K. Mass Balance, Metabolism, and Excretion of Cenobamate, a New Antiepileptic Drug, After a Single Oral Administration in Healthy Male Subjects. Eur. J. Drug. Metab. Pharmacokinet. 2020, 45, 513–522. [Google Scholar] [CrossRef]
- Charlier, B.; Coglianese, A.; Operto, F.F.; Coppola, G.; Grazia, U.; Menna, P.; Filippelli, A.; Piaz, F.; Izzo, V. Development and Validation of a UHPLC-MS/MS-Based Method to Quantify Cenobamate in Human Plasma Samples. Molecules 2022, 27, 7325. [Google Scholar] [CrossRef]
- Arnold, S. Cenobamate: New hope for treatment-resistant epilepsy. Lancet Neurol. 2020, 19, 23–24. [Google Scholar] [CrossRef]
- Steinhoff, B.J. Cenobamate tablets as a treatment for focal-onset seizures in adults. Expert Rev. Clin. Pharmacol. 2021, 14, 161–172. [Google Scholar] [CrossRef]
- Vossler, D.G. Remarkably High Efficacy of Cenobamate in Adults With Focal-Onset Seizures: A Double-Blind, Randomized, Placebo-Controlled Trial. Epilepsy Curr. 2020, 20, 85–87. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, L.; Nisman, A.; Pegan, A.; Ursino, J. An Ex Vivo Evaluation of Cenobamate Administered via Enteral Tubes. Drugs R D 2020, 20, 125–133. [Google Scholar] [CrossRef]
- Löscher, W. Single-Target Versus Multi-Target Drugs Versus Combinations of Drugs with Multiple Targets: Preclinical and Clinical Evidence for the Treatment or Prevention of Epilepsy. Front. Pharmacol. 2021, 12, 730257. [Google Scholar] [CrossRef]
- Steinhoff, B.J. Cenobamate—A new perspective for epilepsy treatment. Nervenarzt 2021, 92, 150–160. [Google Scholar] [CrossRef]
- Nakamura, M.; Cho, J.H.; Shin, H.; Jang, I.S. Effects of cenobamate (YKP3089), a newly developed anti-epileptic drug, on voltage-gated sodium channels in rat hippocampal CA3 neurons. Eur. J. Pharmacol. 2019, 855, 175–182. [Google Scholar] [CrossRef]
- Sankar, R. Treatment of status epilepticus: Physiology, pharmacology, and future directions. Epilepsia Open 2023, 8, 141–148. [Google Scholar] [CrossRef]
- Sharma, R.; Nakamura, M.; Neupane, C.; Jeon, B.H.; Shin, H.; Melnick, S.M.; Glenn, K.J.; Jang, I.S.; Park, J.B. Positive allosteric modulation of GABAA receptors by a novel antiepileptic drug cenobamate. Eur. J. Pharmacol. 2020, 879, 173117. [Google Scholar] [CrossRef] [PubMed]
- Grasshoff, C.; Netzhammer, N.; Schweizer, J.; Antkowiak, B.; Hentschke, H. Depression of spinal network activity by thiopental: Shift from phasic to tonic GABA(A) receptor-mediated inhibition. Neuropharmacology 2008, 55, 793–802. [Google Scholar] [CrossRef] [PubMed]
- Tateiwa, H.; Chintala, S.M.; Chen, Z.; Wang, L.; Amtashar, F.; Bracamontes, J.; Germann, A.L.; Pierce, S.R.; Covey, D.F.; Akk, G.; et al. The Mechanism of Enantioselective Neurosteroid Actions on GABAA Receptors. Biomolecules 2023, 13, 341. [Google Scholar] [CrossRef]
- Roberti, R.; Caro, C.; Iannone, L.F.; Zaccara, G.; Lattanzi, S.; Russo, E. Pharmacology of Cenobamate: Mechanism of Action, Pharmacokinetics, Drug-Drug Interactions and Tolerability. CNS Drugs 2021, 35, 609–618. [Google Scholar] [CrossRef] [PubMed]
- Karaźniewicz-Łada, M.; Główka, A.K.; Mikulska, A.A.; Główka, F.K. Pharmacokinetic Drug-Drug Interactions among Antiepileptic Drugs, Including CBD, Drugs Used to Treat COVID-19 and Nutrients. Int. J. Mol. Sci. 2021, 22, 9582. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.C.; Klein, P.; Krauss, G.L.; Rashid, S.; Seiden, L.G.; Stern, J.M.; Rosenfeld, W.E. Dose Adjustment of Concomitant Antiseizure Medications During Cenobamate Treatment: Expert Opinion Consensus Recommendations. Neurol. Ther. 2022, 11, 1705–1720. [Google Scholar] [CrossRef] [PubMed]
- Villani, F.; Cianci, V.; Bonaventura, C.; Gennaro, G.; Galimberti, C.A.; Guerrini, R.; Neve, A.; Mecarelli, O.; Pietrafusa, N.; Specchio, N.; et al. Use of cenobamate for the treatment of focal epilepsy: An Italian expert opinion paper. Expert Rev. Neurother. 2022, 22, 935–940. [Google Scholar] [CrossRef]
- Greene, S.A.; Kwak, C.; Kamin, M.; Vernillet, L.; Glenn, K.J.; Gabriel, L.; Kim, H.W. Effect of cenobamate on the single-dose pharmacokinetics of multiple cytochrome P450 probes using a cocktail approach in healthy subjects. Clin. Transl. Sci. 2022, 15, 899–911. [Google Scholar] [CrossRef]
- Daina, A.; Michielin, O.; Zoete, V. SwissADME: A free web tool to evaluate pharmacokinetics, drug-likeness and medicinal chemistry friendliness of small molecules. Sci. Rep. 2017, 7, 42717. [Google Scholar] [CrossRef]
- Odi, R.; Bibi, D.; Wager, T.; Bialer, M. A perspective on the physicochemical and biopharmaceutic properties of marketed antiseizure drugs-From phenobarbital to cenobamate and beyond. Epilepsia 2020, 61, 1543–1552. [Google Scholar] [CrossRef]
- Chung, S.S.; French, J.A.; Kowalski, J.; Krauss, G.L.; Lee, S.K.; Maciejowski, M.; Rosenfeld, W.E.; Sperling, M.R.; Mizne, S.; Kamin, M. Randomized phase 2 study of adjunctive cenobamate in patients with uncontrolled focal seizures. Neurology 2020, 94, e2311–e2322. [Google Scholar] [CrossRef]
- Krauss, G.L.; Klein, P.; Brandt, C.; Lee, S.K.; Milanov, I.; Milovanovic, M.; Steinhoff, B.J.; Kamin, M. Safety and efficacy of adjunctive cenobamate (YKP3089) in patients with uncontrolled focal seizures: A multicentre, double-blind, randomised, placebo-controlled, dose-response trial. Lancet Neurol. 2020, 19, 38–48. [Google Scholar] [CrossRef] [PubMed]
- Sperling, M.R.; Klein, P.; Aboumatar, S.; Gelfand, M.; Halford, J.J.; Krauss, G.L.; Rosenfeld, W.E.; Vossler, D.G.; Wechsler, R.; Borchert, L.; et al. Cenobamate (YKP3089) as adjunctive treatment for uncontrolled focal seizures in a large, phase 3, multicenter, open-label safety study. Epilepsia 2020, 61, 1099–1108. [Google Scholar] [CrossRef] [PubMed]
- Vernillet, L.; Greene, S.A.; Kamin, M. Pharmacokinetics of Cenobamate: Results From Single and Multiple Oral Ascending-Dose Studies in Healthy Subjects. Clin. Pharmacol. Drug Dev. 2020, 9, 428–443. [Google Scholar] [CrossRef] [PubMed]
- Elizebath, R.; Zhang, E.; Coe, P.; Gutierrez, E.G.; Yang, J.; Krauss, G.L. Cenobamate treatment of focal-onset seizures: Quality of life and outcome during up to eight years of treatment. Epilepsy Behav. 2021, 116, 107796. [Google Scholar] [CrossRef]
- French, J.A.; Chung, S.S.; Krauss, G.L.; Lee, S.K.; Maciejowski, M.; Rosenfeld, W.E.; Sperling, M.R.; Kamin, M. Long-term safety of adjunctive cenobamate in patients with uncontrolled focal seizures: Open-label extension of a randomized clinical study. Epilepsia 2021, 62, 2142–2150. [Google Scholar] [CrossRef]
- Rosenfeld, W.E.; Nisman, A.; Ferrari, L. Efficacy of adjunctive cenobamate based on number of concomitant antiseizure medications, seizure frequency, and epilepsy duration at baseline: A post-hoc analysis of a randomized clinical study. Epilepsy Res. 2021, 172, 106592. [Google Scholar] [CrossRef]
- Rosenfeld, W.E.; Abou-Khalil, B.; Aboumatar, S.; Bhatia, P.; Biton, V.; Krauss, G.L.; Sperling, M.R.; Vossler, D.G.; Klein, P.; Wechsler, R. Post hoc analysis of a phase 3, multicenter, open-label study of cenobamate for treatment of uncontrolled focal seizures: Effects of dose adjustments of concomitant antiseizure medications. Epilepsia 2021, 62, 3016–3028. [Google Scholar] [CrossRef]
- Sander, J.W.; Rosenfeld, W.E.; Halford, J.J.; Steinhoff, B.J.; Biton, V.; Toledo, M. Long-term individual retention with cenobamate in adults with focal seizures: Pooled data from the clinical development program. Epilepsia 2022, 63, 139–149. [Google Scholar] [CrossRef]
- Sperling, M.R.; Abou-Khalil, B.; Aboumatar, S.; Bhatia, P.; Biton, V.; Klein, P.; Krauss, G.L.; Vossler, D.G.; Wechsler, R.; Ferrari, L.; et al. Efficacy of cenobamate for uncontrolled focal seizures: Post hoc analysis of a Phase 3, multicenter, open-label study. Epilepsia 2021, 62, 3005–3015. [Google Scholar] [CrossRef]
- Yang, E.; Sunwoo, J.; Huh, K.Y.; Kim, Y.K.; Lee, S.; Jang, I.J.; Yu, K.S. Pharmacokinetics and safety of cenobamate, a novel antiseizure medication, in healthy Japanese, and an ethnic comparison with healthy non-Japanese. Clin. Transl. Sci. 2022, 15, 490–500. [Google Scholar] [CrossRef]
- Abou-Khalil, B.; Aboumatar, S.; Klein, P.; Krauss, G.L.; Sperling, M.R.; Rosenfeld, W.E. Efficacy of cenobamate for uncontrolled focal seizures in patients with previous epilepsy-related surgery: Post hoc analysis of a phase 3, multicenter, open-label study. Epilepsy Res. 2022, 184, 106952. [Google Scholar] [CrossRef] [PubMed]
- Aboumatar, S.; Biton, V.; Wechsler, R.; Ferrari, L.; Rosenfeld, W.E. Post hoc analysis of a phase 3 study for treatment of uncontrolled focal seizures: Adjunctive cenobamate dose and seizure reduction by baseline seizure frequency. Epilepsy Res. 2022, 186, 107014. [Google Scholar] [CrossRef]
- Brandt, C.; Sánchez-Álvarez, J.C.; Steinhoff, B.J.; Milanov, I.; Serratosa, J.M. Efficacy and safety of adjunctive cenobamate: Post-hoc analysis of study C017 in patients grouped by mechanism of action of concomitant antiseizure medications. Seizure 2022, 96, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Connor, G.S.; Williamson, A. Effectiveness and safety of adjunctive cenobamate for focal seizures in adults with developmental disability treated in clinical practice. Epilepsy Behav. Rep. 2022, 18, 100533. [Google Scholar] [CrossRef] [PubMed]
- Darpo, B.; Sager, P.T.; Xue, H.; Kamin, M. A Phase 1 Clinical Study Evaluating the Effects of Cenobamate on the QT Interval. Clin. Pharmacol. Drug Dev. 2022, 11, 523–534. [Google Scholar] [CrossRef]
- Elliott, T.; Ridley-Pryor, T.; Gienapp, A.J.; Wheless, J.W. Initial Real-World Experience with Cenobamate in Adolescents and Adults: A Single Center Experience. Pediatr. Neurol. 2022, 129, 19–23. [Google Scholar] [CrossRef]
- Klein, P.; Aboumatar, S.; Brandt, C.; Dong, F.; Krauss, G.L.; Mizne, S.; Sanchez-Alvarez, J.C.; Steinhoff, B.J.; Villanueva, V. Long-Term Efficacy and Safety from an Open-Label Extension of Adjunctive Cenobamate in Patients With Uncontrolled Focal Seizures. Neurology 2022, 99, 989–998. [Google Scholar] [CrossRef]
- Makridis, K.L.; Bast, T.; Prager, C.; Kovacevic-Preradovic, T.; Bittigau, P.; Mayer, T.; Breuer, E.; Kaindl, A.M. Real-World Experience Treating Pediatric Epilepsy Patients with Cenobamate. Front. Neurol. 2022, 13, 950171. [Google Scholar] [CrossRef]
- Makridis, K.L.; Friedo, A.L.; Kellinghaus, C.; Losch, F.P.; Schmitz, B.; Boßelmann, C.; Kaindl, A.M. Successful treatment of adult Dravet syndrome patients with cenobamate. Epilepsia 2022, 63, e164–e171. [Google Scholar] [CrossRef] [PubMed]
- Rosenfeld, W.E.; Ferrari, L.; Kamin, M. Efficacy of cenobamate by focal seizure subtypes: Post-hoc analysis of a phase 3, multicenter, open-label study. Epilepsy Res. 2022, 183, 106940. [Google Scholar] [CrossRef] [PubMed]
- Schuetz, E.; Wagner, K.; Metternich, B.; Papadopoulou, G.; Kravalis, K.; Heers, M.; Martínez-Lizana, E.; Castillo-Rodriguez, M.; Altenmüller, D.M.; Schulze-Bonhage, A.; et al. Effects of cenobamate on cognitive performance of epilepsy patients. Seizure 2022, 102, 129–133. [Google Scholar] [CrossRef]
- Steinhoff, B.J.; Ben-Menachem, E.; Brandt, C.; Morales, I.G.; Rosenfeld, W.E.; Santamarina, E.; Serratosa, J.M. Onset of efficacy and adverse events during Cenobamate titration period. Acta Neurol. Scand. 2022, 146, 265–275. [Google Scholar] [CrossRef]
- Varughese, R.T.; Shah, Y.D.; Karkare, S.; Kothare, S.V. Adjunctive use of cenobamate for pediatric refractory focal-onset epilepsy: A single-center retrospective study. Epilepsy Behav. 2022, 130, 108679. [Google Scholar] [CrossRef]
- Agashe, S.; Worrell, G.; Britton, J.; Noe, K.; Ritaccio, A.; Wirrell, E.C.; Nickels, K.C.; Cascino, G.D.; Burkholder, D. Cenobamate in Generalized Epilepsy and Combined Generalized and Focal Epilepsy. Neurol. Clin. Pract. 2023, 13, e200133. [Google Scholar] [CrossRef]
- Carlson, J.M.; Molyneaux, B.J.; Lee, J.W. Safe Use of Cenobamate in Super Refractory Status Epilepticus: A Case Series. Neurohospitalist 2023, 13, 169–172. [Google Scholar] [CrossRef]
- Elakkary, S.; Hagemann, A.; Klimpel, D.; Bien, C.G.; Brandt, C. A retrospective non-interventional study evaluating the pharmacokinetic interactions between cenobamate and clobazam. Epilepsia 2023, 64, 36–42. [Google Scholar] [CrossRef]
- Falcicchio, G.; Lattanzi, S.; Negri, F.; Tommaso, M.; Neve, A.; Specchio, N. Treatment with Cenobamate in Adult Patients with Lennox-Gastaut Syndrome: A Case Series. J. Clin. Med. 2022, 12, 129. [Google Scholar] [CrossRef]
- Falcicchio, G.; Riva, A.; Neve, A.; Iacomino, M.; Lastella, P.; Suppressa, P.; Sciruicchio, V.; Trojano, M.; Striano, P. Case report: LAMC3-associated cortical malformations: Case report of a novel stop-gain variant and literature review. Front. Genet. 2023, 13, 990350. [Google Scholar] [CrossRef] [PubMed]
- Osborn, M.; Abou-Khalil, B. The cenobamate-clobazam interaction- evidence of synergy in addition to pharmacokinetic interaction. Epilepsy Behav. 2023, 142, 109156. [Google Scholar] [CrossRef]
- Peña-Ceballos, J.; Moloney, P.B.; Munteanu, T.; Doyle, M.; Colleran, N.; Liggan, B.; Breen, A.; Murphy, S.; El-Naggar, H.; Widdess-Walsh, P.; et al. Adjunctive cenobamate in highly active and ultra-refractory focal epilepsy: A “real-world” retrospective study. Epilepsia 2023, 64, 1225–1235. [Google Scholar] [CrossRef]
- Villanueva, V.; Santos-Carrasco, D.; Cabezudo-García, P.; Gómez-Ibáñez, A.; Garcés, M.; Serrano-Castro, P.; Castro-Vilanova, M.D.; Sayas, D.; Lopez-Gonzalez, F.J.; Rodríguez-Osorio, X.; et al. Real-world safety and effectiveness of cenobamate in patients with focal onset seizures: Outcomes from an Expanded Access Program. Epilepsia Open 2023. online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Rosenfeld, W.E.; Ferrari, L.; Kerr, W.T.; Sperling, M.R. Sudden unexpected death in epilepsy during cenobamate clinical development. Epilepsia 2023. online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Lattanzi, S.; Trinka, E.; Zaccara, G.; Striano, P.; Giovane, C.; Silvestrini, M.; Brigo, F. Adjunctive Cenobamate for Focal-Onset Seizures in Adults: A Systematic Review and Meta-Analysis. CNS Drugs 2020, 34, 1105–1120. [Google Scholar] [CrossRef]
- Zhang, L.; Wang, J.; Wang, C. Efficacy and safety of cenobamate in patients with uncontrolled focal seizures: A meta-analysis. Acta Neurol. Scand. 2021, 144, 58–66. [Google Scholar] [CrossRef] [PubMed]
- Cutillo, G.; Tolba, H.; Hirsch, L.J. Anti-seizure medications and efficacy against focal to bilateral tonic-clonic seizures: A systematic review with relevance for SUDEP prevention. Epilepsy Behav. 2021, 117, 107815. [Google Scholar] [CrossRef]
- Lattanzi, S. New evidence in adjunctive treatment of focal-onset seizures in adults: A critical appraisal. Glob. Reg. Health Technol. Assess. 2022, 9, 14–19. [Google Scholar] [CrossRef]
- Lattanzi, S.; Trinka, E.; Zaccara, G.; Striano, P.; Russo, E.; Giovane, C.; Silvestrini, M.; Brigo, F. Third-Generation Antiseizure Medications for Adjunctive Treatment of Focal-Onset Seizures in Adults: A Systematic Review and Network Meta-analysis. Drugs 2022, 82, 199–218. [Google Scholar] [CrossRef]
- Privitera, M.; Richy, F.F.; Schabert, V.F. Indirect treatment comparison of cenobamate to other ASMs for the treatment of uncontrolled focal seizures. Epilepsy Behav. 2022, 126, 108429. [Google Scholar] [CrossRef]
- Klein, P.; Krauss, G.L.; Steinhoff, B.J.; Devinsky, O.; Sperling, M.R. Failure to use new breakthrough treatments for epilepsy. Epilepsia 2023. online ahead of print. [Google Scholar] [CrossRef]
- Flint, I.; Medjedovic, J.; O’Flaherty, E.D.; Alvarez-Baron, E.; Thangavelu, K.; Savic, N.; Meunier, A.; Longworth, L. Mapping analysis to predict SF-6D utilities from health outcomes in people with focal epilepsy. Eur. J. Health Econ. 2022. online ahead of print. [Google Scholar] [CrossRef]
- Mulhern, B.; Mukuria, C.; Barkham, M.; Knapp, M.; Byford, S.; Soeteman, D.; Brazier, J. Using generic preference-based measures in mental health: Psychometric validity of the EQ-5D and SF-6D. Br. J. Psychiatry 2014, 205, 236–243. [Google Scholar] [CrossRef] [PubMed]
- Calleja, M.A.; Navarro, A.; Serratosa, J.M.; Toledo, M.; Villanueva, V.; Labazuy, S.S.; Gil, A. Determination of the economically justifiable price of cenobamate in the treatment of focal-onset seizures in adult patients with drug-resistant epilepsy in Spain. Expert Rev. Pharmacoecon. Outcomes Res. 2022, 22, 1127–1136. [Google Scholar] [CrossRef]
- Laskier, V.; Agyei-Kyeremateng, K.K.; Eddy, A.E.; Patel, D.; Mulheron, S.; James, S.; Thomas, R.H.; Sander, J.W. Cost-effectiveness of cenobamate for focal seizures in people with drug-resistant epilepsy. Epilepsia 2023, 64, 843–856. [Google Scholar] [CrossRef]
- Villanueva, V.; Serratosa, J.M.; Toledo, M.; Calleja, M.A.; Navarro, A.; Sabaniego, J.; Pérez-Domper, P.; Álvarez-Barón, E.; Subías, S.; Gil, A. Number needed to treat and associated cost analysis of cenobamate versus third-generation anti-seizure medications for the treatment of focal-onset seizures in patients with drug-resistant epilepsy in Spain. Epilepsy Behav. 2023, 139, 109054. [Google Scholar] [CrossRef]
- Bialer, M.; Johannessen, S.I.; Levy, R.H.; Perucca, E.; Tomson, T.; White, H.S. Progress report on new antiepileptic drugs: A summary of the Tenth Eilat Conference (EILAT X). Epilepsy Res. 2010, 92, 89–124. [Google Scholar] [CrossRef]
- Wiciński, M.; Puk, O.; Malinowski, B. Cenobamate: Neuroprotective Potential of a New Antiepileptic Drug. Neurochem. Res. 2021, 46, 439–446. [Google Scholar] [CrossRef] [PubMed]
- Buckley, C.T.; Waters, O.R.; DeMaagd, G. Cenobamate: A New Adjunctive Agent for Drug-Resistant Focal Onset Epilepsy. Ann. Pharmacother. 2021, 55, 318–329. [Google Scholar] [CrossRef]
- Bialer, M.; Johannessen, S.I.; Koepp, M.J.; Levy, R.H.; Perucca, E.; Perucca, P.; Tomson, T.; White, H.S. Progress report on new antiepileptic drugs: A summary of the Fifteenth Eilat Conference on New Antiepileptic Drugs and Devices (EILAT XV). II. Drugs in more advanced clinical development. Epilepsia 2020, 61, 2365–2385. [Google Scholar] [CrossRef]
- Shen, M.; Wang, S.; Wen, X.; Han, X.R.; Wang, Y.J.; Zhou, X.M.; Zhang, M.H.; Wu, D.M.; Lu, J.; Zheng, Y.L. Dexmedetomidine exerts neuroprotective effect via the activation of the PI3K/Akt/mTOR signaling pathway in rats with traumatic brain injury. Biomed. Pharmacother. 2017, 95, 885–893. [Google Scholar] [CrossRef]
- Jang, I.S.; Nakamura, M.; Ito, Y.; Akaike, N. Presynaptic GABAA receptors facilitate spontaneous glutamate release from presynaptic terminals on mechanically dissociated rat CA3 pyramidal neurons. Neuroscience 2006, 138, 25–35. [Google Scholar] [CrossRef]
- Kim, Y.; Hsu, C.L.; Cembrowski, M.S.; Mensh, B.D.; Spruston, N. Dendritic sodium spikes are required for long-term potentiation at distal synapses on hippocampal pyramidal neurons. eLife 2015, 4, 06414. [Google Scholar] [CrossRef] [PubMed]
- Schmidt-Wilcke, T.; Fuchs, E.; Funke, K.; Vlachos, A.; Müller-Dahlhaus, F.; Puts, N.A.J.; Harris, R.E.; Edden, R.A.E. GABA-from Inhibition to Cognition: Emerging Concepts. Neuroscientist 2018, 24, 501–515. [Google Scholar] [CrossRef] [PubMed]
- Song, W.S.; Cho, Y.S.; Oh, S.P.; Yoon, S.H.; Kim, Y.S.; Kim, M.H. Cognitive and behavioral effects of the anti-epileptic drug cenobamate (YKP3089) and underlying synaptic and cellular mechanisms. Neuropharmacology 2022, 221, 109292. [Google Scholar] [CrossRef]
- Specchio, N.; Pietrafusa, N.; Vigevano, F. Is Cenobamate the Breakthrough We Have Been Wishing for? Int. J. Mol. Sci. 2021, 22, 9339. [Google Scholar] [CrossRef] [PubMed]
- Strzelczyk, A.; Mann, C.; Willems, L.M.; Rosenow, F.; Bauer, S. Cenobamate for the treatment of focal epilepsies. Expert Opin. Pharmacother. 2020, 21, 2215–2223. [Google Scholar] [CrossRef]
- Sperling, M.; Klein, P.; Kamin, M. Safety of Cenobamate (YKP3089) as Adjunctive Treatment for Uncontrolled Focal Seizures in a Large, Multicenter, Open-Label Study (P1.5-019). Neurology 2019, 92, 19. [Google Scholar]
- Shah, Y.D.; Singh, K.; Friedman, D.; Devinsky, O.; Kothare, S.V. Evaluating the safety and efficacy of felbamate in the context of a black box warning: A single center experience. Epilepsy Behav. 2016, 56, 50–53. [Google Scholar] [CrossRef]
- Mudigoudar, B.; Wheless, J. Safety of adjunctive treatment with cenobamate in patients with uncontrolled focal seizures. Lancet Neurol. 2020, 19, 288. [Google Scholar] [CrossRef]
- Sáenz-Farret, M.; Tijssen, M.A.J.; Eliashiv, D.; Fisher, R.S.; Sethi, K.; Fasano, A. Antiseizure Drugs and Movement Disorders. CNS Drugs 2022, 36, 859–876. [Google Scholar] [CrossRef]
- Kerrick, J.M.; Kelley, B.J.; Maister, B.H.; Graves, N.M.; Leppik, I.E. Involuntary movement disorders associated with felbamate. Neurology 1995, 45, 185–187. [Google Scholar] [CrossRef]
- Rissardo, J.P.; Caprara, A.L.F. Pregabalin-associated movement disorders: A literature review. Brain Circ. 2020, 6, 96–106. [Google Scholar] [CrossRef]
- Rissardo, J.P.; Caprara, A.L.F.; Durante, Í. Valproate-associated Movement Disorder: A Literature Review. Prague Med. Rep. 2021, 122, 140–180. [Google Scholar] [CrossRef] [PubMed]
- Latimer, D.R.; Edinoff, A.N.; Ruff, R.D.; Rooney, K.C.; Penny, K.M.; Patel, S.B.; Sabbenahalli, S.; Kaye, A.M.; Cornett, E.M.; Viswanath, O.; et al. Cenobamate, a Sodium Channel Inhibitor and Positive Allosteric Modulator of GABAA Ion Channels, for Partial Onset Seizures in Adults: A Comprehensive Review and Clinical Implications. Neurol. Int. 2021, 13, 252–265. [Google Scholar] [CrossRef]
- Wheless, J.W. Adjunctive cenobamate for the treatment of focal onset seizures in adults with epilepsy: A critical review. Expert Rev. Neurother. 2020, 20, 1085–1098. [Google Scholar] [CrossRef]
- Tomson, T.; Battino, D.; Bromley, R.; Kochen, S.; Meador, K.J.; Pennell, P.B.; Thomas, S.V. Breastfeeding while on treatment with antiseizure medications: A systematic review from the ILAE Women Task Force. Epileptic Disord. 2022, 24, 1020–1032. [Google Scholar]
- Pong, A.W.; Tyrlikova, I.; Giermek, A.J.; Klein, P. Impact of regulatory safety warnings and restrictions on drug treatment of epilepsy. Expert Opin. Drug Saf. 2023, 22, 111–114. [Google Scholar] [CrossRef]
- Pong, A.W.; Xu, K.J.; Klein, P. Recent advances in pharmacotherapy for epilepsy. Curr. Opin. Neurol. 2023, 36, 77–85. [Google Scholar] [CrossRef]
- Klein, P.; Devinsky, O.; French, J.; Harden, C.; Krauss, G.L.; McCarter, R.; Sperling, M.R. Suicidality Risk of Newer Antiseizure Medications: A Meta-analysis. JAMA Neurol. 2021, 78, 1118–1127. [Google Scholar] [CrossRef]
- Jang, Y.; Moon, J.; Kim, N.; Kim, T.J.; Jun, J.S.; Shin, Y.W.; Chang, H.; Kang, H.R.; Lee, S.T.; Jung, K.H.; et al. A new rapid titration protocol for lamotrigine that reduces the risk of skin rash. Epilepsia Open 2021, 6, 394–401. [Google Scholar] [CrossRef]
- Hussar, D.A. New Drugs 2021, Part 2. Nursing 2021, 51, 18–29. [Google Scholar] [CrossRef]
- Steinhoff, B.J.; Rosenfeld, W.E.; Serratosa, J.M.; Brandt, C.; Klein, P.; Toledo, M.; Krauss, G.L. Practical guidance for the management of adults receiving adjunctive cenobamate for the treatment of focal epilepsy-expert opinion. Epilepsy Behav. 2021, 123, 108270. [Google Scholar] [CrossRef] [PubMed]



| Alkyl-Carbamate | Carisbamate | Cenobamate | Felbamate | Retigabine | |
|---|---|---|---|---|---|
| Mechanism of Action | AMPA, NMDA, Transient Sodium Currents, VGCC | GABAA Receptors and Persistent Sodium Currents | GABAA and NMDA Receptors, Transient Sodium Currents, VGCC | Voltage-Gated Potassium Channels, GABAA Receptors | |
| MES | Mice | 7.9 | 9.8 | 35.5 | 9.3 |
| Rats | 4.4 | 2.9 | 35 | 5.1 | |
| PTZ | Mice | 20.4 | 28.5 | 126 | 149 |
| Rats | NA | NA | >250 | 195 | |
| 6 Hz (mice) | 22 mA | 20.7 | 11 | 13.1 | NA |
| 32 mA | 21.4 | 17.9 | 69.5 | 26 | |
| 44 mA | 27.6 | 16.5 | 241 | 33 | |
| Rotarod test | Mice | 46 | 58 | 220 | 20.5 |
| Rats | 39.5 | 38.9 | >500 | 10 | |
| Kindled seizures c | NA | 16.4 | 296 | 3.2 | |
| Dosage forms and strengths (mg) | 12.5, 25, 50, 100, 150, 200 | |
| Bioavailability | 88%, not influenced by high-fat meal | |
| Peak plasma time: | 1–4 h | |
| Volume distribution | 40–50 L | |
| Plasma-protein binding | 60%, primarily to albumin | |
| Metabolism | Glucuronidation (UGT2B7 > UGT2B4) Oxidation (CYP2E1, CYP2A6, CYP2B6 > CYP2C19, CYP3A4/5) | |
| Elimination half-life (hours) | Human | 50–60 |
| Rat | 2.9 | |
| Mice | NA | |
| Oral clearance | 0.45–9.63 L/hr | |
| Excretion | Renal 87.8% (6% unmetabolized) and feces 5.2% (<1% unmetabolized) | |
| Physicochemical properties extracted from SwissADME b | ||
| Formula | C10H10ClN5O2 | |
| Molecular weight (150–500 g/mol) | 267.67 g/mol | |
| Fraction Csp3 (0.25–1.0) | 0.20 | |
| Num. rotatable bonds (0–9) | 5 | |
| Num. H-bond acceptors (≤10) | 5 | |
| Num. H-bond donors (≤5) | 1 | |
| Topological polar surface area (20–130 Å2) | 95.92 Å2 | |
| Lipophilicity | ||
| Consensus Log Po/w (0.7–5.0) | 0.95 | |
| Water solubility | ||
| Log S (ESOL) (−6–0) | −2.59 | |
| Class | Soluble | |
| Pharmacokinetics | ||
| Gastrointestinal absorption | High | |
| Blood–brain barrier permeant | No | |
| Druglikeness | ||
| Bioavailability score | 0.55 | |
| Medicinal chemistry | ||
| Synthetic accessibility [1(very easy)–10 (very difficult)] | 3.05 | |
| Medication | Effect of CNB on Drug/Substrate | Mechanism | Recommendation |
|---|---|---|---|
| CBZ | Decrease of 24% in plasma CBZ levels | CYP3A4 induction | Monitor plasma CBZ level and increase CBZ dose as needed |
| CLB | Increase in plasma N-desmethylclobazam (active metabolite of CLB) levels | CYP2C19 inhibition | Monitor plasma N-desmethylclobazam levels and decrease CLB dose as needed |
| LTG | Decreases of 21% (CNB 100 mg/day), 35% (CNB 200 mg/day), and 52% (CNB 400 mg/day) in plasma LTG levels | Induction of UDPGT | Monitor plasma LTG levels and increase LTG dose as needed |
| PB | Increase in PB AUC by 37% | CYP2C19 inhibition | Monitor plasma PB levels and decrease PB as needed |
| PHT | Increase in PHT AUC by 84% | CYP2C19 inhibition | Monitor plasma PHT levels. Gradually decrease PHT dose by up to 50% during CNB titration |
| OCP | Decrease in plasma concentrations of OCPs | CYP3A4 induction | Use additional or alternative non-hormonal birth control methods |
| CYP2B6 substrates | Decrease in plasma concentrations of CYP2B6 substrates, e.g., decrease in plasma bupropion levels by 39% | CYP2B6 induction | Increase the dosage of CYP2B6 substrates as needed |
| CYP2C19 substrates | Increase in plasma concentrations of CYP2C19 substrates, e.g., increase in plasma omeprazole levels by 107% | CYP2C19 inhibition | Monitor plasma concentration or response to CYP2C19 substrates and decrease the dose of CYP2C19 substrates as needed |
| CYP3A4 substrates | Decrease in plasma concentrations of CYP3A4 substrates, e.g., decrease in plasma midazolam levels by 27% (CNB 100 mg/day) to 72% (CNB 200 mg/day) | CYP3A4 induction | Increase the dosage of CYP3A4 substrates as needed |
| Drug-induced QT interval shortening | Additive effect on QT interval shortening | Variable | Drugs associated with QT-interval shortening should be cautiously prescribed when in combination with CNB |
| Drug-induced CNS side effects | Additive effect of CNS depressants | Variable | CNS depressants should be cautiously prescribed when in combination with CNB |
| Identifier | Study Start to Completion | Condition | Intervention | N Enrolled | Comment |
|---|---|---|---|---|---|
| NCT04513860 | NA | Focal epilepsy | CNB | NA | The objective of this expanded access program is to continue providing treatment with CNB to patients with focal epilepsy that were enrolled in the SK Life Science Inc clinical trials |
| NCT00616148 | Aug 2007–Jan 2010 | Focal epilepsy | CNB, placebo | 11 | PPR study |
| NCT01397968 | Jul 2011–Jan 2021 | Focal epilepsy | CNB, placebo | 222 | Efficacy of CNB in DRE |
| NCT01866111 | Jul 2013–Oct 2021 | Focal epilepsy | CNB, placebo | 437 | Effective dose range of CNB as adjunctive therapy |
| NCT02535091 | Aug 2016–Feb 2022 | Focal epilepsy | CNB | 1345 | Effective dose range of CNB as adjunctive therapy |
| NCT03234699 | Feb 2017–Jul 2017 | Healthy | CNB, midazolam, warfarin, omeprazole, bupropion | 24 | Investigate the influence of CNB on the activity of CYP3A4/5, CYP2B6, CYP2C19, and CYP2C9 |
| NCT03509285 | Mar 2017–Dec 2017 | Healthy | CNB, alprazolam | 53 | Evaluate the abuse liability potential of CNB in recreational drug users with sedative drug use experience |
| NCT03678753 | Sep 2018–Jul 2024 | Primary generalized epilepsy | CNB, placebo | 170 | Safety and effectiveness of CNB on primary generalized tonic-clonic seizures |
| NCT03961568 | Aug 2019–May 2023 | Primary generalized epilepsy | CNB | 130 | Long-term safety of CNB adjunctive therapy in subjects with primary generalized tonic-clonic seizures |
| NCT04879433 | Jun 2020–Nov 2023 | Focal epilepsy | CNB | 100 | Efficacy, safety, and tolerability of CNB as adjunctive treatment of DRE |
| NCT04690751 | Dec 2020–May 2021 | Healthy | CNB | 28 | Pharmacokinetics of CNB |
| NCT04557085 | Mar 2021–Oct 2024 | Focal epilepsy | CNB, placebo | 540 | Efficacy and safety of 100, 200, and 400 mg/day of CNB as adjunctive therapy in focal epilepsy |
| NCT04903314 | May 2021–Oct 2024 | Focal epilepsy | CNB | 24 | Pharmacokinetics of CNB in pediatric subjects |
| NCT04791553 | Jun 2021–Nov 2022 | NA | CNB | 16 | Effect of severe hepatic impairment on the pharmacokinetics of CNB |
| NCT05067634 | Jan 2022–Jul 2026 | Focal epilepsy | CNB | 140 | Safety and tolerability of CNB in pediatric subjects with focal epilepsy |
| NCT05572255 | Sep 2022–Jan 2023 | Healthy | CNB | 24 | Pharmacokinetics of CNB |
| NCT05859854 | Jan 2023–Sep 2024 | Focal epilepsy | CNB | 200 | Efficacy of CNB in DRE |
| NCT05747001 | Jan 2023–Apr 2023 | Focal epilepsy | CNB | 500 | Effectiveness and tolerability of CNB from real-world data collected in patients who participated in the early access program |
| Reference | Study CO13, NCT01397968, Chung et al. [60] | Study CO17, NCT01866111, Krauss et al. [61] | Study CO21, NCT02535091, Sperling et al. [62] | |
|---|---|---|---|---|
| Type of study | Phase II, R, DB, followed by OLE | Phase II, R, DB, DR, followed by OLE | Phase III, open-label | |
| Seizure type | Focal, uncontrolled a | Focal, uncontrolled b | Focal, uncontrolled b | |
| CNB starting dose mg/day | 50 | 50 c | 12.5 | |
| Titration schedule | Increase by 50 mg every two weeks | Increase by 50 mg every week up to 200 mg, then 100 mg/week thereafter c | Increase to 25 mg for weeks 3 and 4, 50 mg for weeks 5 and 6, and then by 50 mg every 2 weeks thereafter | |
| Titration phase, weeks | 6 | 6 | 12 | |
| CNB target dose for maintenance phase mg/day (N of participants) | 200 (n = 113) | 100 (n = 108); 200 (n = 110); 400 (n = 111) | 200, could be increased to a maximum dose of 400 (n = 1339) | |
| Maintenance phase, weeks | 6 | 12 | ≥40 | |
| Compared group | Placebo (n = 109) | Placebo (n = 108) | NA | |
| Inclusion criteria | Common | 1. Taking 1–3 concomitant ASMs at stable doses; 2. EEG confirming the diagnosis of focal epilepsy; 3. prior neuroimaging | ||
| Specific | 4. Adults 18–65 years old 5. ≥3 focal seizures per month (baseline period 8 weeks) 6. No consecutive 21-day seizure-free interval | 4. Adults 18–70 years old 5. ≥3 focal seizures per month (baseline period 8 weeks), with ≥8 focal seizures during baseline 6. No consecutive 25-day seizure-free interval | 4. Adults 18–70 years old | |
| Exclusion criteria | Common | 1. Taking FBM for <18 continuous months; 2. history of status epilepticus, alcoholism, drug abuse, or psychiatric illness; 3. taking VGB within the past year | ||
| Specific | 4. Taking intermittent rescue benzodiazepines more than once per month within the past month 5. Taking PHT or PB 6. History of >2 allergic reactions to prior ASMs 7. History of 1 serious hypersensitivity reaction | 4. Taking intermittent rescue benzodiazepines more than once per month within the past month 5. Taking diazepam, PHT, or PB 6. History of a serious drug-induced hypersensitivity reaction or drug-related rash requiring treatment in a hospital, ASM drug-associated rash involving conjunctiva or mucosa, or >1 maculopapular rash requiring discontinuation | 4.Taking retigabine (ezogabine) within the past year 5. History of any drug-induced rash or hypersensitivity reaction 6. First-degree relatives with a serious cutaneous, drug-induced adverse reaction | |
| Median % seizure reduction from baseline d | ITT population (primary endpoint) CNB 200 mg (↓55%) * vs. placebo (↓21%) | mITT population (FDA primary endpoint) CNB 400 mg (↓55%) * vs. CNB 200 mg (↓55%) * vs. CNB 100 mg (↓35%) * vs. placebo (↓24%) | NA | |
| Responder rate, % of patients e | • ITT population (secondary endpoint) CNB 200 mg (50%) * vs. placebo (22%) • Post hoc analysis (maintenance phase) CNB 200 mg (62%) * vs. placebo (32%) | mITT-M population (EMA primary endpoint) CNB 400 mg (64%) * vs. CNB 200 mg (56%) * vs. CNB 100 mg (40%) * vs. placebo (25%) | NA | |
| 100% seizure reduction during maintenance phase, % of patients | Post hoc analysis CNB 200 mg (28%) * vs. placebo (8%) | Secondary endpoint CNB 400 mg (21%) * vs. CNB 200 mg (11%) * vs. CNB 100 mg (3%) vs. placebo (1%) | NA | |
| Median % seizure reduction by seizure subtype from baseline | ITT population (secondary endpoint) • Focal aware motor seizures CNB 200 mg (↓76%) * vs. placebo (↓27%) • Focal impaired awareness seizures CNB 200 mg (↓55%) * vs. placebo (↓21%) • Focal to bilateral tonic-clonic seizures CNB 200 mg (↓77%) * vs. placebo (↓33%) | mITT-M population (post-hoc analysis) • Focal aware motor seizures CNB 400 mg (69%) * vs. CNB 200 mg (62%) * vs. CNB 100 mg (49%) * vs. placebo (↑11%) • Focal impaired awareness seizures CNB 400 mg (61%) * vs. CNB 200 mg (55%%) * vs. CNB 100 mg (32%) vs. placebo (29%) • Focal to bilateral tonic-clonic seizures CNB 400 mg (83%) * vs. CNB 200 mg (92%) * vs. CNB 100 mg (51%) vs. placebo (33%) | NA | |
| Most common TEAEs, % of CNB patients (occurring in ≥10% of patients with any dose) | • 22% somnolence • 22% dizziness • 12% headache • 11% nausea • 10% fatigue | • 18% (100 mg), 20% (200 mg), 36% (400 mg) somnolence • 17%, 20%, 33% dizziness • 10%, 10%, 10% headache • 12%, 17%, 24% fatigue • 7%, 10%, 15% diplopia | • 28% somnolence • 23% dizziness • 16% fatigue • 11% headache | |
| Serious TEAEs, % of patients | CNB (1.8%) vs. placebo (3.7%) | CNB 400 mg (7.2%), 200 mg (3.6%), 100 mg (9.3%) vs. placebo (5.6%) | 8.1% | |
| Hypersensitivity reactions in CNB-treated patients, n of patients | 1 (reddening of palms and soles and itching of ears) | 3 (1 non-serious pruritic rash with fever, 1 non-serious rash and facial swelling, 1 DRESS) | 1 | |
| DRESS, n of patients | 0 | 1 (randomized to 200 mg cenobamate with weekly titration) | 0 | |
| Deaths, n of patients (relationship to study drug) | 1 (unrelated, occurred prior to randomization) | 0 | 4 (3 unrelated; 1 remotely related) | |
| Reference | Population | Intervention/Outcome | Comparison | Results/Conclusion | Study Design | Comment |
|---|---|---|---|---|---|---|
| Krauss et al., (2019) [61] | Adult patients with uncontrolled FOS | Safety, efficacy, and tolerability of adjunctive CNB | CNB at dose groups of 100, 200, or 400 mg, or placebo | CNB reduced focal-onset seizure frequency, in a dose-related fashion | MC, DB, R, PC, dose–response | NCT01866111; CO17; N = 437 |
| Trenite et al., (2019) [37] | Adults with photosensitive epilepsy, with/without concomitant ASM therapy | Effect of CNB in patients with PPR to IPS | CNB at dose groups of 100, 250, or 400 mg, or placebo | CNB is a potentially effective product for epilepsy | MC, single-blind | NCT00616148 N = 6 |
| Chung et al., (2020) [60] | Adult patients with uncontrolled FOS | Safety, efficacy, and tolerability of adjunctive CNB | CNB 200 mg or placebo | CNB significantly improved seizure control | MC, DB, PC | NCT01397968; CO13 N = 222 |
| Sperling et al., (2020) [62] | Adult patients with uncontrolled FOS | Safety and tolerability of adjunctive CNB | CNB 12.5 mg/d was initiated and increased at 2-week intervals to 25, 50, 100, 150, and 200 mg/day | CNB was generally well tolerated in the long term, with no new safety issues found | MC, OL | NCT02535091; CO21 N = 1347 |
| Vernillet et al., (2020) [63] | Healthy subjects | Pharmacokinetic characteristics | CNB single (5 to 750 mg) and multiple (50 to 600 mg/day) oral doses or placebo | CNB pharmacokinetic characteristics | R, PC, DB | N = 210 |
| Elizebath et al., (2021) [64] | Adult patients with uncontrolled FOS | Quality of life in epilepsy-31 | CNB 100–200 mg/day | Stable treatment responses during CNB treatment. High responders had high scores in quality of life | Two OL extensions of R and PC studies. One OL safety study | Treated at one center for up to eight years. N = 49 |
| French et al., (2021) [65] | Adult patients with uncontrolled FOS | Safety and tolerability of adjunctive CNB | CNB 50–200 mg or placebo | Safety and tolerability of adjunctive CNB treatment | MC, DB, R, PC, multinational | NCT01397968; CO13; N = 149 |
| Rosenfeld, W.E.; Nisman, A.; et al., (2021) [66] | Adult patients with uncontrolled FOS | Efficacy of adjunctive CNB | CNB at dose groups of 100, 200, or 400 mg, or placebo | Reductions in seizure frequency, which was mainly with the 200 and 400 mg/day groups. | DB, PC, PHA | NCT01866111; N = 397 |
| Rosenfeld, W.E.; Abou-Khalil, B.; et al., (2021) [67] | Adult patients with uncontrolled FOS | Efficacy of adjunctive CNB | CNB 12.5 mg/d was initiated and increased at 2-week intervals to 25, 50, 100, 150, and 200 mg/day | Concomitant ASM dose reductions were associated with more patients remaining on CNB | MC, OL, phase 3, PHA | CO21; N = 240 |
| Sander et al., (2021) [68] | Adult patients with FOS | Retention rates | NA | High retention rates | Two R, PC, CNB studies and one OL safety and pharmacokinetic | N = 1844 |
| Sperling et al., (2021) [69] | Adult patients with uncontrolled FOS | Efficacy of adjunctive CNB | CNB 12.5 mg/d was initiated and increased at 2-week intervals to 25, 50, 100, 150, and 200 mg/day | High rates of sustained seizure reduction, with many achieving response early during titration | MC, OL, phase 3, PHA | CO21; N = 240 |
| Yang et al., (2021) [70] | Healthy Japanese subjects | Pharmacokinetics and safety of CNB | CNB at dose groups of 50 mg, 100 mg, 200 mg, or 400 mg | Similar results to the pattern in non-Japanese subjects | R, DB, PC | KCT0002880 N = 32 |
| Abou-Khalil et al., (2022) [71] | Adult patients with uncontrolled FOS | Efficacy of adjunctive CNB | CNB 12.5 mg/d was initiated and increased at 2-week intervals to 25, 50, 100, 150, and 200 mg/day | Efficacy of CNB in patients with DRE despite prior surgery | MC, OL, phase 3, PHA | CO21; N = 240 |
| Aboumatar et al., (2022) [72] | Adult patients with uncontrolled FOS | Efficacy of adjunctive CNB | CNB 12.5 mg/d was initiated and increased at 2-week intervals to 25, 50, 100, 150, and 200 mg/day | A higher percentage of patients with less vs. more frequent seizures at baseline reached zero seizures | MC, OL, phase 3, PHA | CO21; N = 240 |
| Brandt et al., (2022) [73] | Adult patients with uncontrolled FOS | Efficacy of CNB with co-administration of an ASM that is or is not a sodium channel blocker | CNB at dose groups of 100, 200, or 400 mg, or placebo | CNB is effective with or without sodium channel blocker ASMs | MC, DB, R, PC, dose–response | NCT01866111; CO17; N = 437 |
| Connor et al., (2022) [74] | Adult patients with uncontrolled FOS living with a developmental disability | Efficacy and tolerability of CNB | CNB 50–300 mg/day | CNB is effective and was well tolerated | RE medical chart review | N = 28 |
| Darpo et al., (2022) [75] | Healthy adults | Effects of CNB on the QT interval | Therapeutic and supratherapeutic CNB doses | CNB had no relevant effects on electrocardiographic parameters | Single-center, R, DB, PC, parallel-design | N = 108 |
| Elliott et al., (2022) [76] | Adolescents and adults patients with uncontrolled FOS | Real-world application, a history of drug-related rash | CNB 50–300 mg/day | Patients with a history of rash may benefit from CNB | RE medical chart review | N = 45 |
| Klein et al., (2022) [77] | Adult patients with uncontrolled FOS | Long-term efficacy of adjunctive CNB | CNB (target dose, 300 mg/d; min/max, 50/400 mg/d) | Long-term efficacy was sustained during 48 months of CNB treatment. No new safety issues were identified | MC, DB, R, PC | NCT01866111; N = 355 |
| Makridis, K.L.; Bast, T.; et al., (2022) [78] | Pediatric patients with uncontrolled FOS | Efficacy of adjunctive CNB | CNB 50–400 mg/day | CNB is effective and well-tolerated | RE, MC | N = 16 |
| Makridis, K.L.; Friedo, A.; et al., (2022) [79] | Adult patients with Dravet syndrome | Efficacy of adjunctive CNB | CNB 150–250 mg/day | Long-lasting and significant seizure reduction | RE, MC | N = 4 |
| Rosenfeld et al., (2022) [80] | Adult patients with uncontrolled FOS | Efficacy of adjunctive CNB | CNB 12.5 mg/d was initiated and increased at 2-week intervals to 25, 50, 100, 150, and 200 mg/day | Seizure reductions occurred in all focal seizure subtypes with CNB, with the earliest onset in the focal to bilateral tonic-clonic group | MC, OL, phase 3, PHA | CO21; N = 240 |
| Schuetz et al., (2022) [81] | Adult patients with uncontrolled FOS | Adjunctive treatment with CNB is associated with changes in cognitive performance | CNB 50–250 mg/day | Most of the patients showed stable or improved cognitive performance | Prospective observational | N = 59 |
| Steinhoff et al., (2022) [82] | Adult patients with uncontrolled FOS | Efficacy onset and characteristics of time to onset, duration, and severity of the most common treatment-emergent adverse events | CNB 50–200 mg or placebo | Reductions in seizure frequency occurred during titration with initial efficacy observed prior to reaching the target dose | MC, DB, R, PC, PHA, multinational | NCT01397968; CO13; N = 149 |
| Varughese et al., (2022) [83] | Pediatric patients with uncontrolled FOS | Efficacy of adjunctive CNB | CNB 50–400 mg/day | CNB is effective and well-tolerated | RE, MC | N = 21 |
| Agashe et al., (2023) [84] | Pediatric patients with generalized-onset seizures due to generalized or combined generalized and FOS | Efficacy of CNB | CNB 50–200 mg/day | CNB is effective and well-tolerated | RE medical chart review | N = 13 |
| Carlson et al., (2023) [85] | Adult patients with super-refractory status epilepticus | Efficacy of CNB | CNB 200 mg/day | Both patients achieved seizure control | Case report | N = 2 |
| Elakkary et al., (2023) [86] | Adult patients with uncontrolled FOS | Pharmacokinetic interactions between CNB and CLB | CNB 150–200 mg/day | Concomitant administration of CNB and CLB can lead to a substantial increase in serum concentrations of NCLB | RE medical chart review | N = 5 Increased levels of NCLB were associated with positive therapeutic effect, but with increased levels of fatigue |
| Falcicchio, G.; Lattanzi, S.; et al., (2023) [87] | Adult patients with Lennox–Gastaut syndrome | Efficacy of CNB | CNB 200–300 mg/day | CNB reduced baseline seizure frequency ranged from 25 to 74%, with two patients achieving 50% seizure reduction | RE medical chart review | N = 4 |
| Falcicchio, G.; Riva, A.; et al., (2023) [88] | LAMC3-associated cortical malformations | NA | CNB 300 mg/day | CNB was administered and a partial reduction in seizure frequency | Case report | N = 1 |
| Osborn et al., (2023) [89] | Adult patients with uncontrolled FOS | Pharmacokinetic interactions between CNB and CLB | CNB 25–100 mg/day | Low-dose CLB could be considered in patients with incomplete response to CNB | RE medical chart review | N = 11 |
| Peña-Ceballos et al., (2023) [90] | Adult patients with uncontrolled FOS | CNB’s efficacy and tolerability in a “real-world” severe DRE cohort | CNB 75–350 mg/day | Patients with highly active and ultra-refractory focal epilepsy experienced meaningful seizure outcomes on CNB | RE medical chart review | N = 57 Emergence of adverse events at CNB doses above 250 mg/day |
| Villanueva et al., (2023) [91] | Adult patients with uncontrolled FOS | CNB’s efficacy and tolerability in a “real-world” Spanish expanded access program | CNB 25–300 mg/day | CNB showed a high response regardless of prior and concomitant ASMs. Adverse effects were frequent but mostly mild-to-moderate, and few led to discontinuation | MC, RE, observational | N = 170 |
| Rosenfeld et al., (2023) [92] | Adult patients with uncontrolled FOS | Mortality and standardized mortality ratio during CNB therapy | CNB 100–400 mg/day | CNB may reduce excess mortality associated with epilepsy | RE medical chart review | N = 2132 |
| Timing | Amount | |
|---|---|---|
| Initial dosage | Weeks 1 and 2 | 12.5 mg once daily |
| Titration regimen | Weeks 3 and 4 | 25 mg once daily |
| Weeks 5 and 6 | 50 mg once daily | |
| Weeks 7 and 8 | 100 mg once daily | |
| Weeks 9 and 10 | 150 mg once daily | |
| Maintenance regimen | Week 11 and later | 200 mg once daily |
| Incremental doses after 200 mg/day | Every two weeks | Increase 50 mg once daily until 400 mg once daily |
 | ||
| Who is a candidate for CNB treatment? | Any adults with uncontrolled focal onset seizures. | |
| Specific populations | Elderly | Individuals should be monitored for central nervous system and cognitive adverse events and monitored carefully for potential drug–drug interactions. |
| Woman of child-bearing age | Women who are actively seeking to become pregnant or who are pregnant should consider a different ASM. | |
| Who is not a candidate for CNB therapy? | Patients who require an immediate effect from an ASM. Also, individuals with a history of DRESS or severe hypersensitivity reactions to other drugs. | |
| What is the target CNB dose? | CNB 200 mg/day should be the initial target dose. But, initial signs of efficacy have been reported early in the titration period. | |
| When should the pill be taken? | Dose at bedtime to alleviate adverse events. | |
| Counseling patients about common adverse effects | Advise the patients to inform their provider if adverse effects occur. Adverse effects include somnolence (dose-dependent), dizziness (dose-dependent), fatigue (dose-dependent), diplopia (dose-dependent), headache, and nausea. | |
| Adjusting concomitant ASM | This will depend on the dose/concentration of the ASM and the dose of CNB. | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rissardo, J.P.; Fornari Caprara, A.L. Cenobamate (YKP3089) and Drug-Resistant Epilepsy: A Review of the Literature. Medicina 2023, 59, 1389. https://doi.org/10.3390/medicina59081389
Rissardo JP, Fornari Caprara AL. Cenobamate (YKP3089) and Drug-Resistant Epilepsy: A Review of the Literature. Medicina. 2023; 59(8):1389. https://doi.org/10.3390/medicina59081389
Chicago/Turabian StyleRissardo, Jamir Pitton, and Ana Letícia Fornari Caprara. 2023. "Cenobamate (YKP3089) and Drug-Resistant Epilepsy: A Review of the Literature" Medicina 59, no. 8: 1389. https://doi.org/10.3390/medicina59081389
APA StyleRissardo, J. P., & Fornari Caprara, A. L. (2023). Cenobamate (YKP3089) and Drug-Resistant Epilepsy: A Review of the Literature. Medicina, 59(8), 1389. https://doi.org/10.3390/medicina59081389






