Circumflex Coronary Artery Injury during Modern Mitral Valve Surgery—A Review of Current Concepts and Perspectives
Abstract
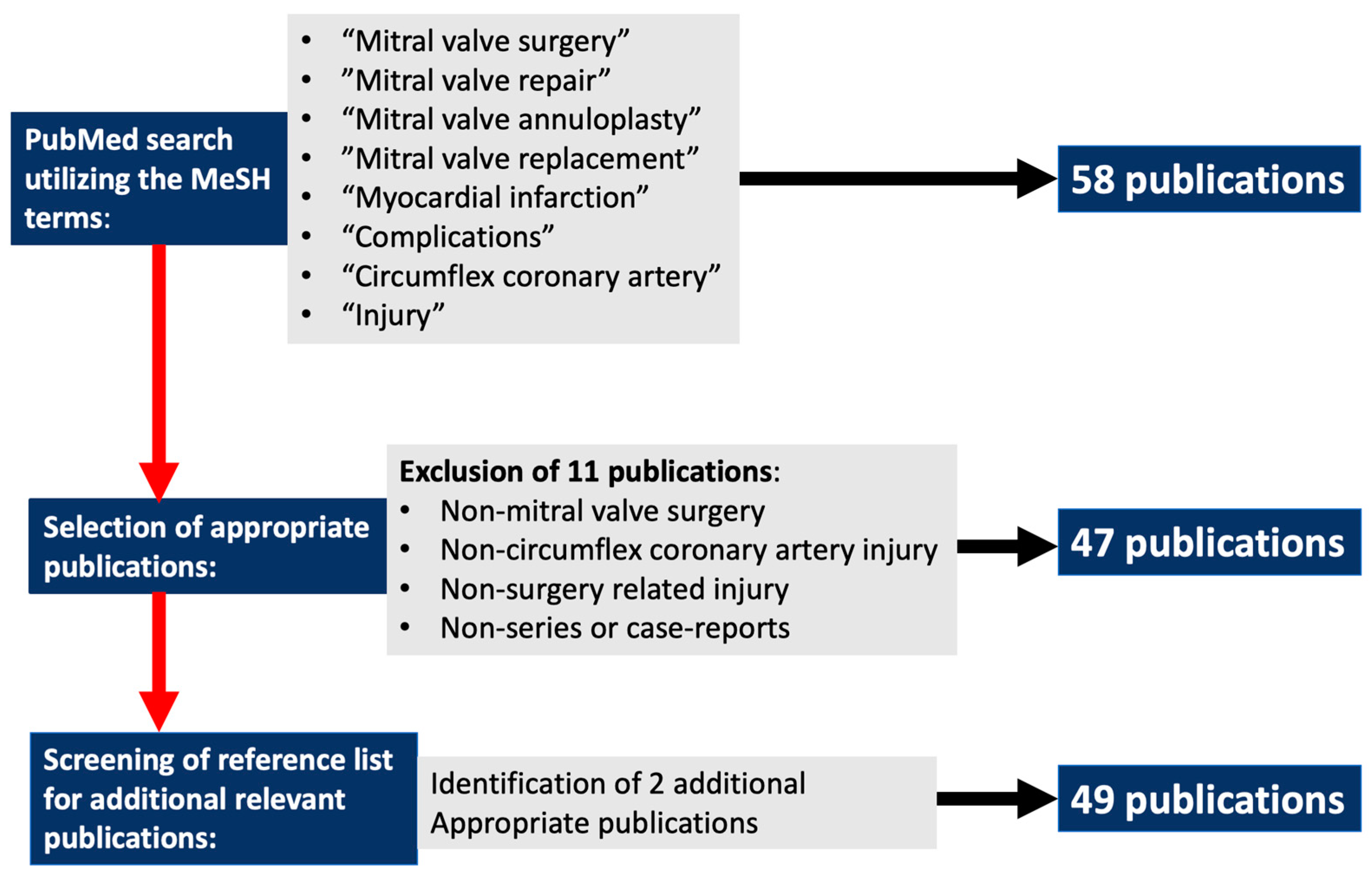
:1. Introduction
2. Current Circumflex Coronary Artery Injury Prevention, Diagnosis and Treatment Strategies
- A.
- Current strategies to identify circumflex coronary arteries at risk during mitral valve surgery
- Coronary angiography;
- Computerized tomography coronary angiography;
- Transthoracic and transesophageal echocardiography;
- B.
- Modern mitral valve surgical techniques and technology to minimize circumflex coronary artery injury risk
- C.
- Intraoperative circumflex coronary artery injury diagnosis and treatment pathways
- D.
- Postoperative and delayed circumflex coronary artery injury diagnosis and treatment strategies
- E.
- The impact of CX injury on contemporary in-hospital outcomes
- F.
- Proposal of a comprehensive algorithm to prevent, diagnose and treat circumflex artery injury during mitral valve surgery
3. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Danielson, G.K.; Cooper, E.; Tweedore, D.N. Circumflex coronary artery injury during mitral valve replacement. Ann. Thorac. Surg. 1967, 4, 53–59. [Google Scholar] [CrossRef]
- Roberts, W.C.; Morrow, A.G. Compression of anomalous left circumflex coronary arteries by prosthetic valve fixation rings. J. Thorac. Cardiovasc. Surg. 1969, 57, 834–838. [Google Scholar] [CrossRef] [PubMed]
- Morin, D.; Fischer, A.P.; Sohl, B.E.; Sadeghi, H. Iatrogenic myocardial infarction. A possible complication of mitral valve surgery related to anatomical variation of the circumflex coronary artery. Thorac. Cardiovasc. Surg. 1982, 30, 176–179. [Google Scholar] [CrossRef] [PubMed]
- Virmani, R.; Chun, P.K.; Parker, J.; McAlister, H.A. Suture obliteration of the circumflex coronary artery in three patients undergoing mitral valve operation. Role of left dominant or codominant coronary artery. J. Thorac. Cardiovasc. Surg. 1982, 84, 773–778. [Google Scholar] [CrossRef]
- Speziale, G.; Fattouch, K.; Ruvolo, G.; Fiorenza, G.; Papalia, U.; Marino, B. Myocardial infarction caused by compression of anomalous circumflex coronary artery after mitral valve replacement. Minerva Cardioangiol. 1998, 46, 455–456. [Google Scholar]
- Tavilla, G.; Pacini, D. Damage to the circumflex artery during MVR with sliding leaflet technique. Ann. Thorac. Surg. 1998, 66, 2091–2093. [Google Scholar] [CrossRef]
- Mulpur, A.K.; Kotidis, K.N.; Nair, U.R. Partial circumflex artery injury during mitral valve replacement: Late presentation. J. Cardiovasc. Surg. 2000, 41, 333–334. [Google Scholar]
- Mantilla, R.; Legarra, J.J.; Pradas, G.; Bravo, M.; Sanmartin, M.; Goicolea, J. Percutaneous coronary intervention for iatrogenic occlusion of the circumflex artery after mitral anuloplasty. Rev. Esp. Cardiol. 2004, 57, 702–704. (In Spanish) [Google Scholar] [CrossRef]
- Sangha, R.; Hui, P. Intravascular ultrasound imaging and percutaneous intervention in a patient with post-mitral valve replacement circumflex coronary artery occlusion. J. Invasive Cardiol. 2004, 16, 351–352. [Google Scholar]
- Nakajima, H.; Ikari, Y.; Kigawa, I.; Kitamura, T.; Hatori, M.; Tooda, E.; Tanabe, K.; Miyairi, T.; Hara, K. Rapid diagnosis and management of intraoperative myocardial infarction during valvular surgery: Using intraoperative transesophageal echocardiography followed by emergency coronary artery bypass grafting without coronary angiography. Echocardiography 2005, 22, 834–838. [Google Scholar] [CrossRef]
- Meursing, D.F.; Boonswang, N.A.; Dobrilovic, N.; Wait, M.A. Perioperative myocardial infarction secondary to dynamic circumflex coronary artery occlusion after mitral valve repair. Tex. Heart Inst. J. 2006, 33, 85–87. [Google Scholar] [PubMed]
- Wykrzykowska, J.; Cohen, D.; Zimetabum, P. Mitral annuloplasty causing left circumflex injury and infarction: Novel use of intravascular ultrasound to diagnose suture injury. J. Invasive Cardiol. 2006, 18, 505–508. [Google Scholar] [PubMed]
- Raza, J.A.; Rodriguez, E.; Miller, M.J. Successful percutaneous revascularization of circumflex artery injury after minimally invasive mitral valve repair and left atrial cryo-MAZE. J. Invasive Cardiol. 2006, 18, E285–E287. [Google Scholar] [PubMed]
- Acar, C. Re: Injury to the circumflex coronary artery following mitral valve repair. Eur. J. Cardiothorac. Surg. 2007, 32, 818. [Google Scholar] [CrossRef]
- Zegdi, R.; Jouan, J.; Fabiani, J.N.; Deloche, A. Injury to the circumflex coronary artery following mitral valve repair. Eur. J. Cardiothorac. Surg. 2007, 31, 740. [Google Scholar] [CrossRef]
- Aubert, S.; Barthelemy, O.; Landi, M.; Acar, C. Circumflex coronary artery injury following mitral annuloplasty treated by emergency angioplasty. Eur. J. Cardiothorac. Surg. 2008, 34, 922–924. [Google Scholar] [CrossRef]
- Gomes, W.J. Injury to the circumflex coronary artery following mitral valve repair: A rather opposite strategy. Eur. J. Cardiothorac. Surg. 2008, 33, 948–949. [Google Scholar] [CrossRef]
- Grande, A.M.; Fiore, A.; Massetti, M.; Vigano, M. Iatrogenic circumflex coronary lesion in mitral valve surgery: Case report and review of the literature. Tex. Heart Inst. J. 2008, 35, 179–183. [Google Scholar]
- Calafiore, A.M.; Iaco, A.L.; Varone, E.; Bosco, P.; Di Mauro, M. Distortion of the proximal circumflex artery during mitral valve repair. J. Card. Surg. 2010, 25, 163–165. [Google Scholar] [CrossRef]
- Ender, J.; Gummert, J.; Fassl, J.; Krohmer, E.; Bossert, T.; Mohr, F.W. Ligation or distortion of the right circumflex artery during minimal invasive mitral valve repair detected by transesophageal echocardiography. J. Am. Soc. Echocardiogr. 2008, 21, 408.e4–408.e5. [Google Scholar] [CrossRef]
- Varela, N.L.; Pulido, J.N.; Lynch, J.J.; Mauermann, W.J.; Rehfeldt, K.H. Acute coronary syndrome after mitral valve surgery: A rare complication secondary to mechanical occlusion of the circumflex artery. Int. Anesthesiol. Clin. 2011, 49, 32–41. [Google Scholar] [CrossRef]
- Murugesan, C.; Raghu, B.; Rao, P.V. Transesophageal Echocardiographic Diagnosis and Management of Circumflex Artery Injury Following Mitral Valve Repair. Cardiol. Res. 2011, 2, 90–92. [Google Scholar] [CrossRef] [PubMed]
- Postorino, S.; Buja, P.; Grassi, G.; Millosevich, P.; Barbierato, M.; Venturini, A.; Zanchettin, C.; Polesel, E.; Di Pede, F.; Raviele, A. Mitral valve repair complicated by iatrogenic coronary artery lesion treated with percutaneous coronary intervention. J. Cardiovasc. Med. 2011, 12, 180–181. [Google Scholar] [CrossRef] [PubMed]
- Sheth, H.; Swamy, R.S.; Shah, A.P. Acute myocardial infarction and cardiac arrest due to coronary artery perforation after mitral valve surgery: Successful treatment with a covered stent. Cardiovasc. Revasc. Med. 2012, 13, 62–65. [Google Scholar] [CrossRef] [PubMed]
- Schyma, C.; Kernbach-Wighton, G.; Madea, B. Kinking of a coronary artery as a rare complication in mitral valve replacement. Forensic Sci. Int. 2012, 221, e30–e33. [Google Scholar] [CrossRef]
- Somekh, N.N.; Haider, A.; Makaryus, A.N.; Katz, S.; Bello, S.; Hartman, A. Left circumflex coronary artery occlusion after mitral valve annuloplasty: “A stitch in time”. Tex. Heart Inst. J. 2012, 39, 104–107. [Google Scholar]
- Ziadi, J.; Mleyhi, S.; Denguir, R.; Khayati, A. Iatrogenic occlusion of the circumflex artery and left ventricle pseudoaneurysm after mitral annuloplasty. J. Cardiol. Cases 2013, 9, 104–105. [Google Scholar] [CrossRef]
- Folkmann, S.; Mohr, F.W.; Garbade, J. Emergency PCI after occlusion of the circumflex artery due to minimally invasive mitral valve replacement in redo operation. Acta Cardiol. 2014, 64, 451–453. [Google Scholar] [CrossRef]
- Pettinari, M.; Gutermann, H.; Van Kerrebroeck, C.; Dion, R. Anomalous Origin of the Circumflex Artery: An Underestimated Threat During Mitral Valve Operation. Ann. Thorac. Surg. 2015, 100, 1437–1439. [Google Scholar] [CrossRef]
- Monteiro, J.P.; Rijo, D.; Simões Costa, S.; Martins, D.; Pereira, R.; Ribeiro, J.; Melica, B.; Vouga, L.; Guerra, M. Circumflex Coronary Artery Lesion and Consequent Papillary Muscle Rupture after Chordal Sparing Mitral Valve Replacement. Rev. Port. Cir. Cardiotorac. Vasc. 2016, 23, 165–168. [Google Scholar]
- Hiltrop, N.; Bennett, J.; Desmet, W. Circumflex coronary artery injury after mitral valve surgery: A report of four cases and comprehensive review of the literature. Catheter. Cardiovasc. Interv. 2017, 89, 78–92. [Google Scholar] [CrossRef] [PubMed]
- Coutinho, G.F.; Leite, F.; Antunes, M.J. Circumflex artery injury during mitral valve repair: Not well known, perhaps not so infrequent-lessons learned from a 6-case experience. J. Thorac. Cardiovasc. Surg. 2017, 154, 1613–1620. [Google Scholar] [CrossRef] [PubMed]
- Busu, T.; Alqahtani, F.; Kawsara, A.; Hijazi, M.; Alkhouli, M. Iatrogenic Circumflex Artery Stenosis Following Mitral Valve Repair. Cureus 2017, 9, e1680. [Google Scholar] [CrossRef]
- Sunagawa, O.; Nakamura, M.; Hokama, R.; Miyara, T.; Taba, Y.; Touma, T. A case of percutaneous coronary intervention for treatment of iatrogenic chronic total occlusion of the left circumflex artery after mitral valve repair. Cardiovasc. Interv. Ther. 2017, 32, 146–150. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, T.A.; Nudy, M.; Pabst, D.; Kozak, M. Mitral valve repair complicated by left circumflex coronary artery occlusion: An under-recognized but potentially deadly complication. Cardiovasc. Revasc. Med. 2018, 19, 77–81. [Google Scholar] [CrossRef]
- Gentry, J.L., 3rd; Summers, M.R.; Harb, S.; Jaber, W.; Pettersson, G.; Griffin, B. Iatrogenic Left Circumflex Coronary Artery Fistula after Mitral Valve Replacement. CASE 2018, 2, 218–221. [Google Scholar] [CrossRef]
- Husain, A.; Alsanei, A.; Tahir, M.; Dahdouh, Z.; AlHalees, Z.; AlMasood, A. Left circumflex artery injury postmitral valve surgery, single center experience. J. Saudi Heart Assoc. 2019, 31, 94–99. [Google Scholar] [CrossRef]
- Fortunato, G.A.; Misfeld, M.; Battellini, R.; Domenech, A.; Garbade, J.; Borger, M.A.; Kotowicz, V. Situation Awareness for Circumflex Artery Injury During Mitral Valve Surgery. Ann. Thorac. Surg. 2019, 108, e329–e332. [Google Scholar] [CrossRef]
- Scarsini, R.; De Maria, G.L.; Ciofani, J.; Jin, X.Y.; Sayeed, R.; Petrou, M.; Banning, A. Coronary Injury in Mitral and Aortic Valve Surgery: A Case Series Using Optical Coherence Tomography. Ann. Thorac. Surg. 2020, 109, e171–e174. [Google Scholar] [CrossRef]
- Dello, S.A.; Leus, S.J.; Tan, M.E.S.; Otterspoor, L.C.; Botman, C.J. Percutaneous coronary intervention of an iatrogenic occlusion of the circumflex coronary artery after mitral valve replacement. Eur. Heart J. Acute Cardiovasc. Care 2020, 9, NP1–NP2. [Google Scholar] [CrossRef]
- Felekos, I.; Theodoropoulos, K.C.; Mullen, L. Acute Circumflex Occlusion After a Successful Mitral Valve Repair. Cardiovasc. Revasc. Med. 2020, 21, 60–62. [Google Scholar] [CrossRef] [PubMed]
- Caruso, V.; Sabry, H.; Birdi, I. Dramatic resolution of an immediate postoperative distortion of the circumflex artery during mitral valve surgery. J. Card. Surg. 2020, 35, 1135–1137. [Google Scholar] [CrossRef] [PubMed]
- Yavari, N.; Ghorbanpour Landy, M.; Motevali, Y.; Tavousi Tabatabaei, E.; Mansourian, S.; Mohseni Badalabadi, R.; Javad Mehrabanian, M.; Hossein Ahmadi Tafti, S. Iatrogenic left circumflex coronary occlusion following mitral valve replacement surgery: A case report. Clin. Case Rep. 2021, 9, 1534–1538. [Google Scholar] [CrossRef]
- Arevalos, V.; Ortega-Paz, L.; Pereda, D.; Sandoval, E.; Brugaletta, S. Percutaneous treatment of a circumflex artery occlusion after minimally invasive barlow disease mitral valve repair. JACC Case Rep. 2021, 3, 173–176. [Google Scholar] [CrossRef] [PubMed]
- Gaba, P.; Kaneko, T.; Kochar, A.; Sung, J.; O’Gara, P.T.; Bhatt, D.L. Left circumflex artery injury following surgical mitral valve replacement: A case report. Eur. Heart J. Case Rep. 2021, 5, ytab464. [Google Scholar] [CrossRef]
- Landa, A.B.; Hoyos, J.; D’Mello, J. Mitral valve repair complicated by left circumflex coronary artery occlusion: The vital role of the anesthesiologist. Ann. Card. Anaesth. 2021, 24, 405–407. [Google Scholar] [CrossRef]
- Bulak, L.; Brzozowski, P.; Reczuch, K.W.; Kuliczkowski, W. Iatrogenic circumflex coronary artery injury after mitral valve replacement. Postepy Kardiol. Interwencyjnej 2021, 17, 315–316. [Google Scholar] [CrossRef]
- Bargagna, M.; Trumello, C.; Sala, A.; Blasio, A.; Castiglioni, A.; Alfieri, O.; De Bonis, M. Left circumflex artery injury after mitral valve surgery: An algorithm management proposal. Ann. Thorac. Surg. 2020, 111, 899–904. [Google Scholar] [CrossRef]
- Nassereddine, Z.; Kazem, H.; Moussa, M.; Saab, M. Left circumflex coronary artery injury following mitral valve replacement with late presentation: A case report and literature review. J. Cardiovasc. Thorac. Res. 2022, 14, 268–271. [Google Scholar] [CrossRef]
- Pessa, C.J.N.; Gomes, W.J.; Catani, R.; Prates, J.C.; Buffolo, E. Anatomical relashionship [sic] between the posterior mitral valve annulus and the coronary arteries. Implication to operative treatment. Braz. J. Cardiovasc. Surg. 2004, 19, 372–377. [Google Scholar] [CrossRef]
- Bevilacqua, C.; Eibel, S.; Foldyna, B.; Knoefler, T.; Lehmkuhl, L.; Gutberlet, M.; Mukherjee, C.; Seeburger, J.; Davierwala, P.; Ender, J. Analysis of circumflex artery anatomy by real time 3D transesophageal echocardiography compared to cardiac computed tomography. Int. J. Cardiovasc. Imaging 2017, 33, 1703–1710. [Google Scholar] [CrossRef] [PubMed]
- Kishimoto, N.; Takahashi, Y.; Fujii, H.; Sakon, Y.; Izuta, S.; Kitada, R.; Morisaki, A.; Yoshida, H.; Ehara, S.; Shibata, T. Computed tomography to identify risk factors for left circumflex artery injury during mitral surgery. Eur. J. Cardiothorac. Surg. 2022, 61, 675–683. [Google Scholar] [CrossRef] [PubMed]
- Mak, G.J.; Blanke, P.; Ong, K.; Naoum, C.; Thompson, C.R.; Webb, J.G.; Moss, R.; Boone, R.; Ye, J.; Cheung, A.; et al. Three-Dimensional Echocardiography Compared With Computed Tomography to Determine Mitral Annulus Size Before Transcatheter Mitral Valve Implantation. Circ. Cardiovasc. Imaging 2016, 9, e004176. [Google Scholar] [CrossRef] [PubMed]
- Man, J.P.; Bouma, B.J.; Schuuring, M.J. Fusion imaging in preoperative planning of mitral valve surgery to prevent injury of the left circumflex artery. Eur. Heart J. 2022, 43, 4762. [Google Scholar] [CrossRef]
- Nakanishi, R.; Osawa, K.; Kurata, A.; Miyoshi, T. Role of coronary computed tomography angiography (CTA) post the ISCHEMIA trial: Precision prevention based on coronary CTA-derived coronary atherosclerosis. J. Cardiol. 2022, 79, 572–580. [Google Scholar] [CrossRef]
- Krzanowski, M.; Bodzoń, W.; Dimitrow, P.P. Imaging of all three coronary arteries by transthoracic echocardiography. An illustrated guide. Cardiovasc. Ultrasound 2003, 1, 16. [Google Scholar] [CrossRef]
- Ender, J.; Selbach, M.; Borger, M.A.; Krohmer, E.; Falk, V.; Kaisers, U.X.; Mohr, F.W.; Mukherjee, C. Echocardiographic identification of iatrogenic injury of the circumflex artery during minimally invasive mitral valve repair. Ann. Thorac. Surg. 2010, 89, 1866–1872. [Google Scholar] [CrossRef]
- Młynarski, R.; Młynarska, A.; Sosnowski, M. Anatomical variants of left circumflex artery, coronary sinus and mitral valve can determine safety of percutaneous mitral annuloplasty. Cardiol. J. 2013, 20, 235–240. [Google Scholar] [CrossRef]
- Caruso, V.; Shah, U.; Sabry, H.; Gedela, S.; Birdi, I. Mitral valve annulus and circumflex artery: In vivo study of anatomical zones. J. Thorac. Cardiovasc. Surg. Tech. 2020, 4, 122–129. [Google Scholar] [CrossRef]
- Bennani, F.; Sebestyen, A.; Grimont, P.; Ghaffar, N.; Cavallo, D.; Nocenti, M.; Tardy, N.; Chessel, E.; Chaffanjon, P.; Chavanon, O. Relationships between coronary arteries and atrioventricular annuli: Surgical and percutaneous implications. Gen. Thorac. Cardiovasc. Surg. 2022, 70, 132–138. [Google Scholar] [CrossRef]
- Van der Merwe, J.; Casselman, F. Mitral Valve Replacement-Current and Future Perspectives. Open J. Cardiovasc. Surg. 2017, 9, 1179065217719023. [Google Scholar] [CrossRef] [PubMed]
- Carpentier, A.F.; Lessana, A.; Relland, J.Y.; Belli, E.; Mihaileanu, S.; Berrebi, A.J.; Palsky, E.; Loulmet, D.F. The “Physio-Ring”: An advanced concept in mitral valve annuloplasty. Ann. Thorac. Surg. 1995, 60, 1177–1185. [Google Scholar] [PubMed]
- Carpentier, A.; Adams, D.H.; Filsoufi, F. Carpentier’s Reconstructive Valve Surgery: From Valve Analysis to Valve Reconstruction; Saunders-Elsevier: Philadelphia, PA, USA, 2010. [Google Scholar]
- Filsoufi, F.; Carpentier, A. Principles of reconstructive surgery in degenerative mitral valve disease. Semin. Thorac. Cardiovasc. Surg. 2007, 19, 103–110. [Google Scholar] [CrossRef]
- Van der Merwe, J.; Casselman, F.; Van Praet, F. The principles of minimally invasive atrioventricular valve repair surgery utilizing endoaortic balloon occlusion technology: How to start and sustain a safe and effective program. J. Vis. Surg. 2019, 5, 72. [Google Scholar] [CrossRef]
- Van der Merwe, J.; Casselman, F.; Van Praet, F. Minimally invasive atrioventricular surgery—Current status and future perspectives. SA Heart 2019, 16, 310–316. [Google Scholar] [CrossRef]
- Van der Merwe, J.; Van Praet, F.; Stockman, B.; Degrieck, I.; Vermeulen, Y.; Casselman, F. Reasons for conversion and adverse intraoperative events in Endoscopic Port Access™ atrioventricular valve surgery and minimally invasive aortic valve surgery. Eur. J. Cardiothorac. Surg. 2018, 54, 288–293. [Google Scholar]
- Van der Merwe, J.; Van Praet, F.; Vermeulen, Y.; Casselman, F. Complications and pitfalls in minimally invasive atrioventricular valve surgery utilizing endo-aortic balloon occlusion technology. J. Vis. Surg. 2018, 4, 248. [Google Scholar] [CrossRef]
- Czesla, M.; Götte, J.; Weimar, T.; Ruttkay, T.; Doll, N. Safeguards and pitfalls in minimally invasive mitral valve surgery. Ann. Cardiothorac. Surg. 2013, 2, 849–852. [Google Scholar]
- De Backer, O.; Wong, I.; Taramasso, M.; Maisano, F.; Franzen, O.; Søndergaard, L. Transcatheter mitral valve repair: An overview of current and future devices. Open Heart 2021, 8, e001564. [Google Scholar] [CrossRef]
- Noack, T.; Kiefer, P.; Besler, C.; Lurz, P.; Leontyev, S.; Abdel-Wahab, M.; Holzhey, D.M.; Seeburger, J. Transcatheter mitral valve repair: Review of current techniques. Indian. J. Thorac. Cardiovasc. Surg. 2020, 36 (Suppl. S1), 53–63. [Google Scholar] [CrossRef]
- Kargoli, F.; Pagnesi, M.; Rahgozar, K.; Goldberg, Y.; Ho, E.; Chau, M.; Colombo, A.; Latib, A. Current Devices and Complications Related to Transcatheter Mitral Valve Replacement: The Bumpy Road to the Top. Front. Cardiovasc. Med. 2021, 8, 639058. [Google Scholar] [CrossRef] [PubMed]
- Fiorilli, P.N.; Herrmann, H.C.; Szeto, W.Y. Transcatheter mitral valve replacement: Latest advances and future directions. Ann. Cardiothorac. Surg. 2021, 10, 85–95. [Google Scholar] [CrossRef] [PubMed]
- Otto, C.M.; Nishimura, R.A.; Bonow, R.O.; Carabello, B.A.; Erwin, J.P., 3rd; Gentile, F.; Jneid, H.; Krieger, E.V.; Mack, M.; McLeod, C.; et al. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2021, 143, e35–e71. [Google Scholar] [CrossRef] [PubMed]
- Vahanian, A.; Beyersdorf, F.; Praz, F.; Milojevic, M.; Baldus, S.; Bauersachs, J.; Capodanno, D.; Conradi, L.; De Bonis, M.; De Paulis, R.; et al. ESC/EACTS Scientific Document Group. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur. Heart J. 2022, 43, 561–632. [Google Scholar] [CrossRef]
- Cornu, E.; Lacroix, P.H.; Christides, C.; Laskar, M. Coronary artery damage during mitral valve replacement. J. Cardiovasc. Surg. 1995, 36, 261–264. [Google Scholar]
- Kaklikkaya, I.; Yeginoglu, G. Damage to coronary arteries during mitral valve surgery. Heart Surg. Forum 2003, 6, E138–E142. [Google Scholar]
- Iung, B.; Baron, G.; Tornos, P.; Gohlke-Bärwolf, C.; Butchart, E.G.; Vahanian, A. Valvular heart disease in the community: A European experience. Curr. Probl. Cardiol. 2007, 32, 609–661. [Google Scholar] [CrossRef]
- Hu, X.; Zhao, Q. Systematic evaluation of the flexible and rigid annuloplasty ring after mitral valve repair for mitral regurgitation. Eur. J. Cardiothorac. Surg. 2011, 40, 480–487. [Google Scholar] [CrossRef]
- Cetinkaya, A.; Waheed, M.; Bramlage, K.; Liakopoulos, O.J.; Zeriouh, M.; Hein, S.; Bramlage, P.; Schönburg, M.; Choi, Y.H.; Richter, M. Comparison of flexible, open with semi-rigid, closed annuloplasty-rings for mitral valve repair. J. Cardiothorac. Surg. 2021, 16, 35. [Google Scholar] [CrossRef]
- Chang, B.C.; Youn, Y.N.; Ha, J.W.; Lim, S.H.; Hong, Y.S.; Chung, N. Long-term clinical results of mitral valvuloplasty using flexible and rigid rings: A prospective and randomized study. J. Thorac. Cardiovasc. Surg. 2007, 133, 995–1003. [Google Scholar] [CrossRef]
- Silberman, S.; Klutstein, M.W.; Sabag, T.; Oren, A.; Fink, D.; Merin, O.; Bitran, D. Repair of ischemic mitral regurgitation: Comparison between flexible and rigid annuloplasty rings. Ann. Thorac. Surg. 2009, 87, 1721–1726. [Google Scholar] [CrossRef] [PubMed]
- Chauvette, V.; Bouchard, D.; Pellerin, M.; Perrault, L.P. Commentary: Mitral valve annuloplasty and circumflex artery injury: Are fewer stitches better? JTCVS Tech. 2020, 5, 31–33. [Google Scholar] [CrossRef] [PubMed]
- Obarski, T.P.; Loop, F.D.; Cosgrove, D.M.; Lytle, B.W.; Stewart, W.J. Frequency of acute myocardial infarction in valve repairs versus valve replacement for pure mitral regurgitation. Am. J. Cardiol. 1990, 65, 887–890. [Google Scholar] [CrossRef] [PubMed]
- Sardari Nia, P.; Daemen, J.H.T.; Maessen, J.G. Development of a high-fidelity minimally invasive mitral valve surgery simulator. J. Thorac. Cardiovasc. Surg. 2019, 157, 1567–1574. [Google Scholar] [CrossRef]
- Ascione, G.; Denti, P. Mitral annular calcification in patients with significant mitral valve disease: An old problem with new solutions. Front. Cardiovasc. Med. 2022, 9, 1033565. [Google Scholar] [CrossRef] [PubMed]
- van der Merwe, J.; Casselman, F.; Stockman, B.; Roubelakis, A.; Vermeulen, Y.; Degrieck, I.; Van Praet, F. Endoscopic port access surgery for isolated atrioventricular valve endocarditis. Interact. Cardiovasc. Thorac. Surg. 2018, 27, 487–493. [Google Scholar] [CrossRef]
- Tibaut, M.; Mekis, D.; Petrovic, D. Pathophysiology of Myocardial Infarction and Acute Management Strategies. Cardiovasc. Hematol. Agents Med. Chem. 2017, 14, 150–159. [Google Scholar] [CrossRef]





| Author | Year | Procedure | Access | Mechanism | Time of Diagnosis | 30-Day Mortality | Treatment Strategy |
|---|---|---|---|---|---|---|---|
| Danielson [1] | 1967 | MVR (n = 3) | Sterno | Total | PO | Yes | None |
| Roberts [2] | 1969 | MVR | Sterno | Total | PO | Yes | None |
| Morin [3] | 1982 | MVR | Sterno | Total | PO | Yes | None |
| Virmani [4] | 1982 | MVR (n = 2) MVr (n = 1) | Sterno | Total | PO | Yes | None |
| Speziale [5] | 1998 | MVR | Sterno | Total | PO | None | none |
| Tavilla [6] | 1998 | MVr | Sterno | Total | IntraO | None | Revision and CABG |
| Mulpur [7] | 2000 | MVR | Sterno | Partial | Del | None | MVR |
| Mantilla [8] | 2004 | MVr | Sterno | Partial | PO | None | PCI |
| Sangha [9] | 2004 | MVr | Sterno | Partial | PO | None | PCI |
| Nakajima [10] | 2005 | MVr | Sterno | Total | IntraO | None | CABG |
| Meursing [11] | 2006 | MVr | Sterno | Partial | IntraO | None | PCI |
| Wykrzykowska [12] | 2006 | MVr | Sterno | Partial | PO | None | PCI |
| Raza [13] | 2006 | MVr | MI-MVS | Partial | IntraO | None | PCI |
| Acar [14] | 2007 | MVr (n = 3) | Sterno | Total (n = 3) | IntraO (n = 3) | None | CABG (n = 3) |
| Zegdi [15] | 2007 | MVr | Sterno | Partial | PO | None | CABG |
| Aubert [16] | 2008 | MVr | Sterno | Partial | IntraO | None | PCI |
| Gomes [17] | 2008 | MVr (n = 2) | Sterno | Partial | IntraO | None | Revision |
| Grande [18] | 2008 | MVr | MI-MVS | Partial | IntraO | None | PCI |
| Calafiore [19] | 2010 | MVr | Sterno | Total | IntraO | None | CABG |
| Ender [20] | 2010 | MVr (n = 3) | MI-MVS | Partial (n = 3) | IntraO (n = 3) | None | Revision (n = 2) PCI (n = 1) |
| Varela [21] | 2011 | MVr (n = 2) | Sterno | Partial | PO | None | PCI (n = 2) |
| Murugesan [22] | 2011 | MVr | Sterno | Partial | IntraO | None | Revision |
| Postorino [23] | 2011 | MVr | Sterno | Partial | PO | None | PCI |
| Sheth [24] | 2012 | MVR | Sterno | Laceration | PO | None | PCI |
| Schyma [25] | 2012 | MVR | Sterno | Partial | PO | yes | None |
| Somekh [26] | 2012 | MVr | MI-MVS | Total | PO | None | PCI |
| Ziadi [27] | 2014 | MVr | Sterno | Partial | Del(5 months) | None | CABG and aneurysmectomy |
| Folkmann [28] | 2014 | MVR | MI-MVS | Partial | IntraO | None | PCI |
| Pettinari [29] | 2015 | MVr | Sterno | Partial | PO | None | PCI |
| Monteiro [30] | 2016 | MVr | Sterno | Partial | Del | None | Revision |
| Hiltrop [31] | 2016 | MVr (n = 2) MVR (n = 2) | MI-MVS (n = 2) Sterno (n = 2) | Total (n = 1) Partial (n = 2) | IntraO (n = 1) PO (n = 2) Del (n = 1) | Yes (n = 1) | PCI (n = 2) CABG (n = 2) |
| Coutinho [32] | 2017 | MVr (n = 6) | Sterno | Partial (n = 3) Total (n = 3) | PO (n = 6) | None | None (n = 1) Transplant (n = 1) Revision (n = 3) PCI (n = 1) |
| Busu [33] | 2017 | MVr | Sterno | Partial | Del (2 years) | None | PCI |
| Sunagawa [34] | 2017 | MVr | Sterno | Total | Del (3 years) | None | PCI |
| Ahmad [35] | 2018 | MVr | Sterno | Total | IntraO | Yes | PCI |
| Gentry [36] | 2018 | MVR | Sterno | Fistula | Del (1 year) | None | Redo-MVR |
| Husain [37] | 2018 | MVR (n = 9) | Sterno | Partial (n = 3) Total (n = 6) | N/A | Yes (n = 3) | PCI (n = 3) CABG (n = 6) |
| Fortunato [38] | 2019 | MVr (n = 4) MVR (n = 1) | Sterno | Total (n = 4) Partial (n = 1) | PO (n = 2) IntraO (n =3) | Yes (n = 2) | None (n = 1) PCI (n = 2) CABG (n = 1) Revision (n = 1) |
| Scarsini [39] | 2020 | MVr (n = 2) | Sterno | Partial (n = 2) | IntraO (n = 2) | None | PCI (n = 2) |
| Dello [40] | 2020 | MVR | Sterno | Partial | IntraO | None | PCI |
| Felekos [41] | 2020 | MVr | MI-MVS | Partial | IntraO | None | PCI |
| Caruso [42] | 2020 | MVr | MI-MVS | Partial | IntraO | None | Revision |
| Yavari [43] | 2020 | MVR | Sterno | Partial | PO | None | PCI (unsuccessful) |
| Arevalos [44] | 2021 | MVr | MI-MVS | Total | PO | None | PCI |
| Gaba [45] | 2021 | Redo-MVR | Sterno | Total | IntraO | None | PCI |
| Landa [46] | 2021 | MVr | MI-MVS | Partial | IntraO | None | PCI |
| Bulak [47] | 2021 | MVR | Sterno | Total | PO | None | PCI |
| Bargagna [48] | 2021 | MVr (n = 5) MVR (n = 5) | Sterno | Total (n = 4) Partial (n = 6) | PO (n = 5) IntraO = 5 | Yes (n = 2) | PCI (n = 4) CABG (n = 5) Revision (n = 1) |
| Nassereddine [49] | 2022 | MVr | Sterno | Total | Del (4 weeks) | None | PCI (unsuccessful) |
| Echocardiographic/clinical criteria Repeat mitral valve surgery Severe posterior mitral annular calcification Destructive posterior leaflet infection Anomalous circumflex coronary artery course Circumflex artery distance to mitral valve annulus less than 3 mm Coronary angiographic criteria Anomalous circumflex coronary artery course Left dominant coronary system Codominant coronary system Computerised tomographic coronary angiographic criteria Circumflex artery distance to mitral valve annulus less than 3 mm |
| External compression Oversized prosthesis Hematoma Suture injury Vessel laceration with bleeding Vessel distortion with partial occlusion Vessel occlusion Thermal injury of endothelium Cryoablation injury Radiofrequency ablation injury Embolism Air Bone marrow Fat fragments Suture material Prosthetic material |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
van der Merwe, J.; Casselman, F. Circumflex Coronary Artery Injury during Modern Mitral Valve Surgery—A Review of Current Concepts and Perspectives. Medicina 2023, 59, 1470. https://doi.org/10.3390/medicina59081470
van der Merwe J, Casselman F. Circumflex Coronary Artery Injury during Modern Mitral Valve Surgery—A Review of Current Concepts and Perspectives. Medicina. 2023; 59(8):1470. https://doi.org/10.3390/medicina59081470
Chicago/Turabian Stylevan der Merwe, Johan, and Filip Casselman. 2023. "Circumflex Coronary Artery Injury during Modern Mitral Valve Surgery—A Review of Current Concepts and Perspectives" Medicina 59, no. 8: 1470. https://doi.org/10.3390/medicina59081470




