Type I Dentin Dysplasia: The Literature Review and Case Report of a Family Affected by Misrecognition and Late Diagnosis
Abstract
1. Introduction
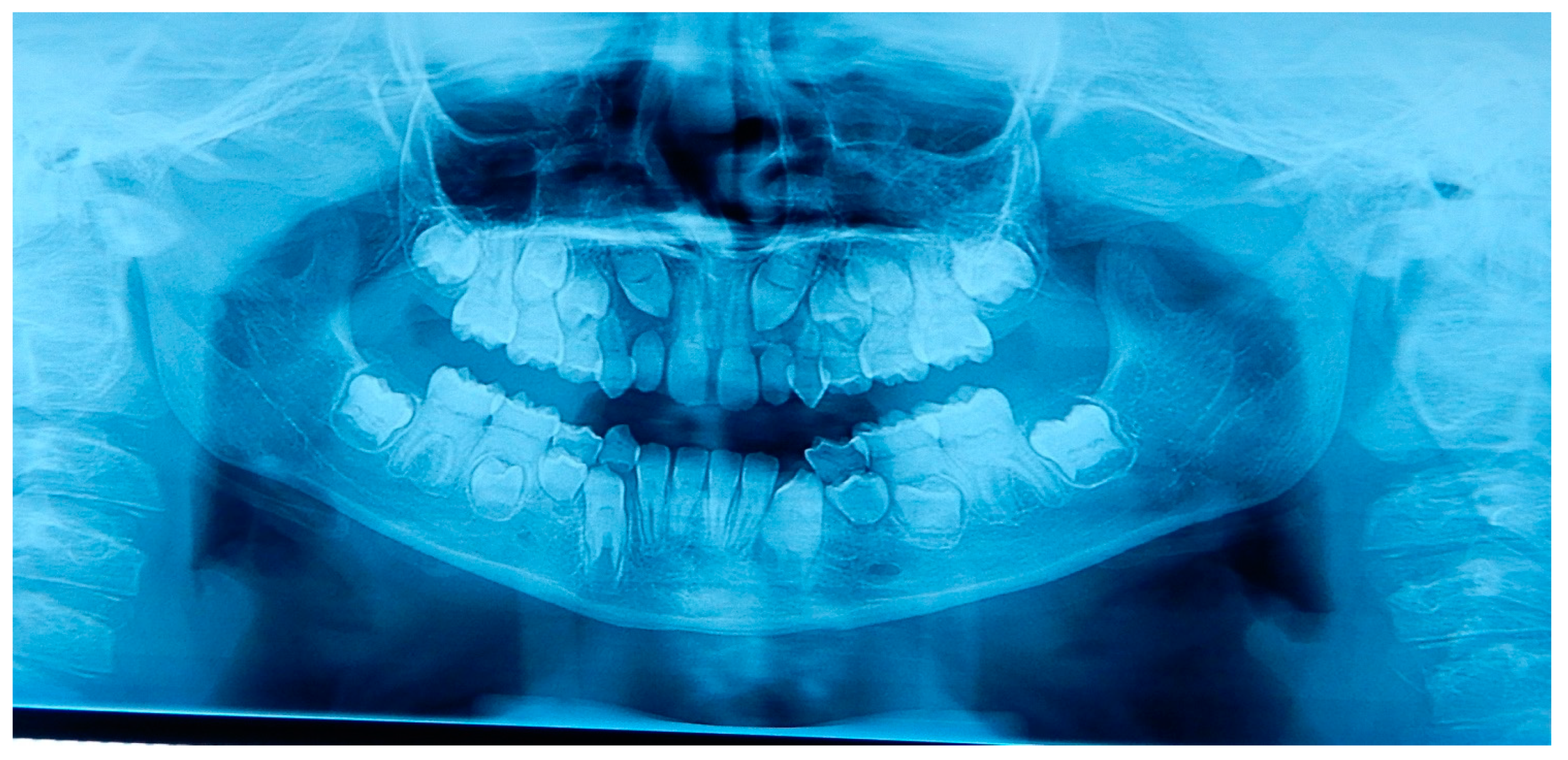
2. Case Presentation
2.1. Patient A
2.2. Patient B
2.3. Father
2.4. Other Family Members
2.5. Differential Diagnosis and Genetic Tests
2.6. Dental Management of the Affected Children and Father
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shields, E.D.; Bixler, D.; El-Kafrawy, A.M. A proposed classification of heritable human dentine defects with a description of a new entity. Arch. Oral Biol. 1973, 18, 543–553. [Google Scholar] [CrossRef] [PubMed]
- Shankly, P.E.; Mackie, I.C.; Sloan, P. Dentinal dysplasia type I: Report of a case. Int. J. Pediatr. Dent. 1999, 9, 37–42. [Google Scholar] [CrossRef] [PubMed]
- Orphanet. Available online: https://www.orpha.net/consor/cgi-bin/OC_Exp.php?lng=EN&Expert=99789 (accessed on 20 January 2023).
- Coila, B.; Bahn, S.L.; Goviea, G.L. Radiographic manifestations of an unusual combination Type I and Type II dentine dysplasia. Oral Surg. 1978, 45, 317–322. [Google Scholar]
- Carroll, M.K.O.; Duncan, W.K.; Perkins, T.M. Dentin dysplasia: Review of the literature and a proposed subclassification based on radiographic findings. Oral Surg. Oral Med. Oral Pathol. 1991, 72, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Carroll, M.K.O.; Duncan, W.K. Dentin dysplasia type I. Radiologic and genetic perspectives in a six-generation family. Oral Surg. Oral Med. Oral Pathol. 1994, 78, 375–381. [Google Scholar] [CrossRef]
- Omami, G. Rootless teeth and Condylar osteolysis. Gen. Dent. 2021, 69, 76–78. [Google Scholar]
- Xu, C.; Xie, X.; Zhao, L.; Wu, Y.; Wang, J. The critical role of nuclear factor I-C in tooth development. Oral Dis. 2022, 28, 2093–2099. [Google Scholar] [CrossRef]
- Ranjitkar, S.; Yong, R.; Wu, I.C.; Gully, G.; Farmer, D.; Watson, I.; Heithersay, G.S. Dentinal dysplasia type 1: A 3D micro-computed tomographic study of enamel, dentine and root canal morphology. Aust. Endod. J. 2019, 45, 298–304. [Google Scholar] [CrossRef]
- Simmer, J.P.; Zhang, H.; Moon, S.J.H.; Donnelly, L.A.; Lee, Y.L.; Seymen, F.; Koruyucu, M.; Chan, H.C.; Lee, K.Y.; Wu, S.; et al. The Modified Shields Classification and 12 Families with Defined DSPP Mutations. Genes 2022, 13, 858. [Google Scholar] [CrossRef]
- Charisi, C.; Kodonas, K.; Keklikoglou, K.; Arhakis, A.; Arapostathis, K.A.; Kotsanos, N. Morphological, histological, and chemical analysis of first permanent molars with molar incisor malformation. Eur. Arch. Paediatr. Dent. 2022, 23, 601–608. [Google Scholar] [CrossRef]
- Massé, L.; Etienne, O.; Noirrit-Esclassan, E.; Bailleul-Forestier, I.; Garot, E. Dentine disorders and adhesive treatments: A systematic review. J. Dent. 2021, 109, 103654. [Google Scholar] [CrossRef]
- Ruan, W.; Duan, X. A new SMOC2 mutation within selective tooth agenesis, malformed teeth and dentin dysplasia. Clin. Genet. 2022, 102, 352–354. [Google Scholar] [CrossRef]
- Kim, Y.J.; Lee, Y.; Zhang, H.; Seymen, F.; Koruyucu, M.; Bayrak, S.; Tuloglu, N.; Simmer, J.P.; Hu, J.C.C.; Kim, J.W. Translated Mutant DSPP mRNA Expression Level Impacts the Severity of Dentin Defects. J. Pers. Med. 2022, 12, 1002. [Google Scholar] [CrossRef]
- Su, T.; Zhu, Y.; Wang, X.; Zhu, Q.; Duan, X. Hereditary dentin defects with systemic diseases. Oral Dis. 2023. [Google Scholar] [CrossRef]
- Okawa, R.; Hamada, M.; Takagi, M.; Matayoshi, S.; Nakano, K. A Case of X-Linked Hypophosphatemic Rickets with Dentin Dysplasia in Mandibular Third Molars. Children 2022, 9, 1304. [Google Scholar] [CrossRef] [PubMed]
- Ni, X.; Gong, Y.; Jiang, Y.; Li, X.; Pang, Q.; Liu, W.; Chi, Y.; Jiajue, R.; Wang, O.; Li, M.; et al. The First Compound Heterozygous Mutations of DMP1 Causing Rare Autosomal Recessive Hypophosphatemic Rickets Type 1. J. Clin. Endocrinol. Metab. 2023, 108, 791–801. [Google Scholar] [CrossRef] [PubMed]
- Depprich, R.A.; Ommerborn, M.A.; Handschel, J.G.; Naujoks, C.D.; Meyer, U.; Kübler, N.R. Dentin dysplasia type I: A challenge for treatment with dental implants. Head Face Med. 2007, 3, 31. [Google Scholar] [CrossRef] [PubMed]
- Malik, S.; Gupta, S.; Wadhwan, V.; Suhasini, G.P. Dentin dysplasia type I—A rare entity. J. Oral Maxillofac. Pathol. 2015, 19, 110. [Google Scholar] [CrossRef]
- Lee, J.W.; Hong, J.; Seymen, F.; Kim, Y.J.; Kang, J.; Koruyucu, M.; Tuloglu, N.; Bayrak, S.; Song, J.S.; Shin, T.J.; et al. Novel frameshift mutations in DSPP cause dentin dysplasia type II. Oral Dis. 2019, 25, 2044–2046. [Google Scholar] [CrossRef]
- Xiong, F.; Ji, Z.; Liu, Y.; Zhang, Y.; Hu, L.; Yang, Q.; Qiu, Q.; Zhao, L.; Chen, D.; Tian, Z.; et al. Mutation in SSUH2 Causes Autosomal-Dominant Dentin Dysplasia Type I. Hum. Mutat. 2017, 38, 95–104. [Google Scholar] [CrossRef]
- Zhu, Q.L.; Duan, X.H.; Yu, Q. Mutation of dentin sialophosphoprotein and hereditary malformations of dentin. Zhonghua Kou Qiang Yi Xue Za Zhi 2023, 58, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Kim, Y.J.; Hyun, H.K.; Lee, J.C.; Lee, Z.H.; Kim, J.W. Non-Syndromic Dentinogenesis Imperfecta Caused by Mild Mutations in COL1A2. J. Pers. Med. 2021, 11, 526. [Google Scholar] [CrossRef] [PubMed]
- Gopalakrishnan, S.; Balasubramaniam, N.; Ramamoorthi, R.; Vedachalam, R. A case of multiple rootless teeth: A case report and review. J. Oral Maxillofac. Pathol. 2021, 25, 559. [Google Scholar] [CrossRef]
- Buchanan, G.D.; Tredoux, S.; Nel, C.; Gamieldien, M.Y. Endodontic treatment of dentin dysplasia type I D. Aust. Endod. J. 2021, 47, 343–349. [Google Scholar] [CrossRef]
- Council on Clinical affairs of the American Association of Pediatric Dentistry. Guideline on Dental Management of Heritable Dental Developmental Anomalies. Ref. Man. Clin. Pract. Guidel. 2013, 38, 302–307. [Google Scholar]
- Korshunov, A.S.; Vagner, V.D.; Kuryatnikov, K.N.; Serov, D.O.; Torohov, A.L.; Shykhalieva, D.D.; Sarf, E.A.; Bel’skaya, L.V. Infrared Spectroscopy to Analyze Sexual Dimorphism of Hard Dental Tissue Maturation at Eruption in Patients with Connective Tissue Dysplasia. Appl. Spectrosc. 2023, 77, 457–469. [Google Scholar] [CrossRef]
- Kumar, N.; Ansari, S.; Shrivastava, H.; Patsa, S.; Ray, J.G. Dentin Dysplasia Type I: Case series and review of the literature. Int. J. Dent. Health Sci. 2015, 2, 198–202. [Google Scholar]
- Toomarian, L.; Mashhadiabbas, F.; Mirkarimi, M.; Mehrdad, L. Dentin dysplasia type I: A case report and review of the literature. J. Med. Case Rep. 2010, 4, 1. [Google Scholar] [CrossRef]
- Ansari, G.; Reid, J.S. Dentinal dysplasia type I: Review of the literature and report of a family. ASDC J. Dent. Child. 1997, 64, 429–434. [Google Scholar]
- Krug, R.; Volland, J.; Reich, S.; Soliman, S.; Connert, T.; Krastl, G. Guided endodontic treatment of multiple teeth with dentin dysplasia: A case report. Head Face Med. 2020, 16, 27. [Google Scholar] [CrossRef]
- Fulari, S.G.; Tambake, D.P. Rootless teeth: Dentin dysplasia type I. Contemp. Clin. Dent. 2013, 4, 520–522. [Google Scholar] [CrossRef] [PubMed]
- Papagiannis, A.; Fanourakis, G.; Mitsea, A.; Karayianni, K.; Vastardis, H.; Sifakakis, I. Orthodontic Treatment of a Patient with Dentin Dysplasia Type I and Bilateral Maxillary Canine Impaction: Case Presentation and a Family-Based Genetic Analysis. Children 2021, 8, 519. [Google Scholar] [CrossRef] [PubMed]
- Leonardi, R.; Ronsivalle, V.; Barbato, E.; Lagravère, M.; Flores-Mir, C.; Lo Giudice, A. External root resorption (ERR) and rapid maxillary expansion (RME) at post-retention stage: A comparison between tooth-borne and bone-borne RME. Prog. Orthod. 2022, 23, 45. [Google Scholar] [CrossRef]
- Shahrure, B.; Acar, A. Evaluation of Risk Factors for Severe Apical Root Resorption in the Maxillary Incisors Following Fixed Orthodontic Treatment. Turk. J. Orthod. 2022, 35, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Lo Giudice, A.; Leonardi, R.; Ronsivalle, V.; Allegrini, S.; Lagravère, M.; Marzo, G.; Isola, G. Evaluation of pulp cavity/chamber changes after tooth-borne and bone-borne rapid maxillary expansions: A CBCT study using surface-based superimposition and deviation analysis. Clin. Oral Investig. 2021, 25, 2237–2247. [Google Scholar] [CrossRef]
- de Andrade Vieira, W.; Oliveira, M.B.; Machado, L.S.; Cericato, G.O.; Lima, I.F.P.; Paranhos, L.R. Pulp changes from rapid maxillary expansion: A systematic review. Orthod. Craniofac. Res. 2022, 25, 320–335. [Google Scholar] [CrossRef]
- Putrino, A.; Caputo, M.; Giovannoni, D.; Barbato, E.; Galluccio, G. Impact of the SARS-CoV-2 pandemic on orthodontic therapies: An italian experience of teleorthodontics. Pesqui. Bras. Odontopediatria Clínica Integr. 2020, 20, e0100. [Google Scholar] [CrossRef]
- Patel, N.; Viswanathan, A.; Lee, J.; Barrow, S.; Cant, A.; Sanghvi, R.; Deseta, M.; Layton, J.; Bhujel, N.; Sheehy, E.C. Paediatric dental A&E service during the COVID-19 pandemic in the Greater London area. Eur. Arch. Paediatr. Dent. 2021, 22, 507–513. [Google Scholar] [CrossRef]
- Damoiselet, C.; Veynachter, T.; Jager, S.; Baudet, A.; Hernandez, M.; Clément, C. Teledentistry and management protocol in a pediatric dental department during the first COVID-19 lockdown. Arch. Pediatr. Infect. Dis. 2023, 30, 20–24. [Google Scholar] [CrossRef]
- Sangalli, L.; Savoldi, F.; Dalessandri, D.; Bonetti, S.; Gu, M.; Signoroni, A.; Paganelli, C. Effects of remote digital monitoring on oral hygiene of orthodontic patients: A prospective study. BMC Oral Health 2021, 21, 435. [Google Scholar] [CrossRef]
- Putrino, A.; Federica, A.; Denise, G.; Roberto, D.G.; Ersilia, B.; Gabriella, G.; Michele, C. Williams syndrome: Oral findings and orthodontic management of a rare disease. Int. J. Dent. Oral Sci. 2021, 8, 3690–3694. [Google Scholar] [CrossRef]
- Akhil Jose, E.J.; Palathingal, P.; Baby, D.; Thachil, J.M. Dentin dysplasia Type I: A rare case report. J. Oral Maxillofac. Pathol. 2019, 23, 309. [Google Scholar] [CrossRef] [PubMed]
- Alhilou, A.; Beddis, H.P.; Mighell, A.J.; Durey, K. Dentin dysplasia: Diagnostic challenges. BMJ Case Rep. 2018, 2018, bcr-2017-223942. [Google Scholar] [CrossRef] [PubMed]
- Picanço, G.V.; de Freitas, K.M.; Cançado, R.H.; Valarelli, F.P.; Picanço, P.R.; Feijão, C.P. Predisposing factors to severe external root resorption associated to orthodontic treatment. Dent. Press J. Orthod. 2013, 18, 110–120. [Google Scholar] [CrossRef]
- Pinzon, M.L.; Gong, S.G. Arrested root formation of 4 second premolars: Report of a patient. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 652–656. [Google Scholar] [CrossRef]
- Edwards, P.C. Considering that this is such a rare condition, should we really be expected to recognize it? Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2011, 112, 143–145. [Google Scholar] [CrossRef][Green Version]
- Precious, D.S. In exhortation of advocacy: We can do better. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013, 115, 565. [Google Scholar] [CrossRef]
- Montanari Vergallo, G.; Zaami, S. Guidelines and best practices: Remarks on the Gelli-Bianco law. Clin. Ter. 2018, 169, e82–e85. [Google Scholar] [CrossRef]








Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Putrino, A.; Caputo, M.; Galeotti, A.; Marinelli, E.; Zaami, S. Type I Dentin Dysplasia: The Literature Review and Case Report of a Family Affected by Misrecognition and Late Diagnosis. Medicina 2023, 59, 1477. https://doi.org/10.3390/medicina59081477
Putrino A, Caputo M, Galeotti A, Marinelli E, Zaami S. Type I Dentin Dysplasia: The Literature Review and Case Report of a Family Affected by Misrecognition and Late Diagnosis. Medicina. 2023; 59(8):1477. https://doi.org/10.3390/medicina59081477
Chicago/Turabian StylePutrino, Alessandra, Martina Caputo, Angela Galeotti, Enrico Marinelli, and Simona Zaami. 2023. "Type I Dentin Dysplasia: The Literature Review and Case Report of a Family Affected by Misrecognition and Late Diagnosis" Medicina 59, no. 8: 1477. https://doi.org/10.3390/medicina59081477
APA StylePutrino, A., Caputo, M., Galeotti, A., Marinelli, E., & Zaami, S. (2023). Type I Dentin Dysplasia: The Literature Review and Case Report of a Family Affected by Misrecognition and Late Diagnosis. Medicina, 59(8), 1477. https://doi.org/10.3390/medicina59081477








