Traumatic Brain Injury in Cameroon: A Prospective Observational Study in a Level I Trauma Centre
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population
2.3. Data Collection
2.4. Outcome Measures
2.5. Data Management and Analysis
2.6. Ethical Clearance and Administrative Authorizations
3. Results
3.1. Presentation of Sociodemographic and Clinical Features
3.2. Clinical Details of Participants
3.3. Injury Details of Participants
3.4. Pre-Hospital Details of TBI Patients
3.5. Injury Characteristics and Management
3.6. Discharge Status of Participants
3.7. Six Months Outcome after Hospital Discharge
3.8. Comparison of Six-Month TBI Outcomes and Time Difference between Injury and Arrival, Type of Referral, and TBI Severity
4. Discussion
4.1. Demographic and Injury Characteristics
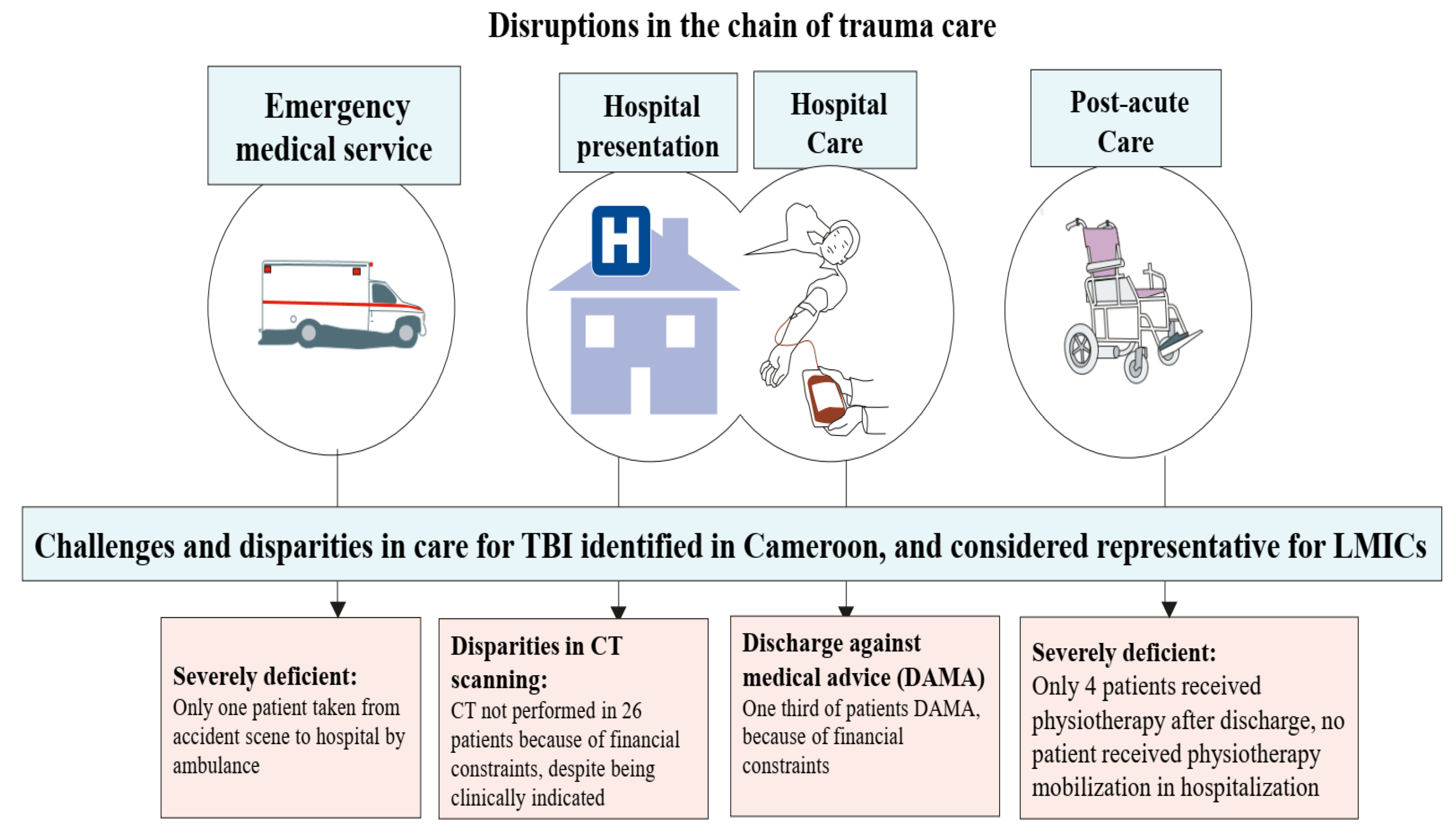
4.2. Pre-Hospital Care and Post-Acute Care
4.3. Disparities in Care due to Financial Constraints
4.4. Outcome
4.5. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dewan, M.C.; Rattani, A.; Gupta, S.; Baticulon, R.E.; Hung, Y.-C.; Punchak, M.; Agrawal, A.; Adeleye, A.O.; Shrime, M.G.; Rubiano, A.M.; et al. Estimating the global incidence of traumatic brain injury. J. Neurosurg. 2019, 130, 1080–1097. [Google Scholar] [CrossRef]
- Wongchareon, K.; Thompson, H.J.; Mitchell, P.H.; Barber, J.; Temkin, N. IMPACT and CRASH prognostic models for traumatic brain injury: External validation in a South-American cohort. INJ Prev. 2020, 26, 546–554. [Google Scholar] [CrossRef]
- GBD 2016 Traumatic Brain Injury and Spinal Cord Injury Collaborators. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 56–87. [Google Scholar] [CrossRef] [PubMed]
- Sun, D.; Jiang, B.; Ru, X.; Sun, H.; Fu, J.; Wu, S.; Wang, L.; Wang, L.; Zhang, M.; Liu, B.; et al. For the NESS-China investigators. Prevalence and Altered Causes of Traumatic Brain Injury in China: A Nationwide Survey in 2013. Neuroepidemiology 2020, 54, 106–113. [Google Scholar] [CrossRef]
- Brazinova, A.; Rehorcikova, V.; Taylor, M.S.; Buckova, V.; Majdan, M.; Psota, M.; Peeters, W.; Feigin, V.; Theadom, A.; Holkovic, L.; et al. Epidemiology of Traumatic Brain Injury in Europe: A Living Systematic Review. J. Neurotrauma 2021, 38, 1411–1440. [Google Scholar] [CrossRef]
- Boniface, R.; Lugazia, E.R.; Musa, A.; Kiloloma, O. Management and outcome of traumatic brain injury patients at Muhimbili Orthopaedic Institute Dar es Salaam, Tanzania. Pan Afr. Med. J. 2017, 26, 140. [Google Scholar] [CrossRef]
- Adegboyega, G.; Zolo, Y.; Sebopelo, L.A.; Dalle, D.U.; Dada, O.E.; Mbangtang, C.B.; Tetinou, F.; Kanmounye, U.S.; Alalade, A.F. The Burden of Traumatic Brain Injury in Sub-Saharan Africa: A Scoping Review. World Neurosurg. 2021, 156, e192–e205. [Google Scholar] [CrossRef]
- Toth, A. Advanced Imaging in Traumatic Brain Injury 2017. Ph.D. Thesis, Universitas Quinqueecclesiennsis, Pecs, Hungary, 2017; p. 119. [Google Scholar]
- Djientcheu, V.; Fongang, E.N.; Etoundi, P.O.; Esiene, A.; Motah, M.; Tchaleu, C.; Emakam, E.; Tonye, R.; Nonga, B.N.; Essiben, X.; et al. Mortality of head injuries in Sub-Saharan African countries: The case of the university teaching hospitals of Cameroon. J. Neurol. Sci. 2016, 371, 100–104. [Google Scholar] [CrossRef] [PubMed]
- Najem, D.; Rennie, K.; Ribecco-Lutkiewicz, M.; Ly, D.; Haukenfrers, J.; Liu, Q.; Nzau, M.; Fraser, D.D.; Bani-Yaghoub, M. Traumatic brain injury: Classification, models, and markers. Biochem. Cell Biol. 2018, 96, 391–406. [Google Scholar] [CrossRef]
- National Institute of Neurological Disorders. Traumatic Brain Injury: Hope through Research. 2019. Available online: https://catalog.ninds.nih.gov/sites/default/files/publications/traumatic-brain-injury-hope-through-research_1.pdf (accessed on 2 August 2023).
- Dadas, A.; Washington, J.; Diaz-Arrastia, R.; Janigro, D. Biomarkers in traumatic brain injury (TBI): A review. Neuropsychiatr. Dis. Treat. 2018, 14, 2989–3000. [Google Scholar] [CrossRef] [PubMed]
- Ashley, M.J. Assessment of mild traumatic brain injury. In Traumatic Brain Injury Rehabilitation, Treatment, and Case Management, 4th ed.; Ashley, M.J., Hovda, M.J., Eds.; CRC Press/Taylor & Francis: Boca Raton, FL, USA, 2018; pp. 321–3340. [Google Scholar]
- Ndoumbe, A.; Edu, P.B.N.; Simeu, C.; Takongmo, S. Epidemiological Analysis of 135 Cases of Severe Traumatic Brain Injury Managed at a Surgical Intensive Care Unit. Open J. Mod. Neurosurg. 2018, 8, 119–131. [Google Scholar] [CrossRef]
- Motah, M.; Ndoumbe, A.; Massi, D.G.; Bekolo, F.F.; Inemb, G.B.; Moumi, M.; Esene, I.; Chunteng, N.T.; Boukar, Y.E.; Eyenga, V.-C. Traumatic intracranial haemorrhage in Cameroon: Clinical features, treatment options and outcome. Interdiscip. Neurosurg. 2021, 26, 101346. [Google Scholar] [CrossRef]
- Eaton, J.; Hanif, A.B.; Grudziak, J.; Charles, A. Epidemiology, Management, and Functional Outcomes of Traumatic Brain Injury in Sub-Saharan Africa. World Neurosurg. 2017, 108, 650–655. [Google Scholar] [CrossRef] [PubMed]
- World Population Review. Douala Population 2023. Available online: https://worldpopulationreview.com/world-cities/doualapopulation (accessed on 20 June 2023).
- National Heart, Lung and Blood Institute. Low Blood Pressure. Consulted 26 March 2022; 2022. Available online: https://www.nih.gov/about-nih/what-we-do/nih-almanac/national-heart-lung-blood-institute-nhlbi (accessed on 2 August 2023).
- Rappaport, M.; Hall, K.M.; Hopkins, K.; Belleza, T.; Cope, D.N. Disability rating scale for severe head trauma: Coma to community. Arch. Phys. Med. Rehabil. 1982, 63, 118–123. [Google Scholar]
- Mehmood, A.; Zia, N.; Kobusingye, O.; Namaganda, R.H.; Ssenyonjo, H.; Kiryabwire, J.; Hyder, A.A. Determinants of emergency department disposition of patients with traumatic brain injury in Uganda: Results from a registry. Trauma Surg. Acute Care Open 2018, 3, e000253. [Google Scholar] [CrossRef]
- El-Menyar, A.; Mekkodathil, A.; Al-Thani, H.; Consunji, R.; Latifi, R. Incidence, Demographics, and Outcome of Traumatic Brain Injury in The Middle East: A Systematic Review. World Neurosurg. 2017, 107, 6–21. [Google Scholar] [CrossRef] [PubMed]
- Sami, A.; Moafian, G.; Najafi, A.; Aghabeigi, M.-R.; Yamini, N.; Heydari, S.T.; Lankarani, K.-B. Educational level and age as contributing factors to road traffic accidents. Chin. J. Traumatol. 2013, 16, 281–285. [Google Scholar]
- Amram, O.; Schuurman, N.; Pike, I.; Yanchar, N.L.; Friger, M.; McBeth, P.B.; Griesdale, D. Socio Economic Status and Traumatic Brain Injury amongst Pediatric Populations: A Spatial Analysis in Greater Vancouver. Int. J. Environ. Res. Public Health 2015, 12, 15594–15604. [Google Scholar] [CrossRef]
- Buh, F.C.; Taiwe, G.S.; Maas, A.I.R.; Motah, M.; Youm, E.; Wanyu, B.Y.; Wang, K.W.; Hutchinson, P.J.A.; Sumbele, I.U.N. Demographics, Causes, and Outcome of Traumatic Brain Injury among Trauma Cases in Cameroon: A Multi-Center Five Year’s Retrospective Study. Neurotrauma Rep. 2022, 3, 569–583. [Google Scholar] [CrossRef]
- Kouagheu, J. Au Cameroun, dans la jungle des motos-taxisA Douala, sept accidents de la circulation sur dix sont causés par les bend-skinneurs, ces jeunes chauffeurs sans le sou et, souvent, sans permis de conduire. Monde Afr 2020. Available online: https://www.lemonde.fr/afrique/article/2020/02/03/au-cameroun-dans-la-jungle-des-motos-taxis_6028276_3212.html (accessed on 2 August 2023).
- Fu, T.S.; Jing, R.; McFaull, S.R.; Cusimano, M.D. Health & Economic Burden of Traumatic Brain Injury in the Emergency Department. Can. J. Neurol. Sci. 2016, 43, 238–247. [Google Scholar]
- Steyerberg, E.W.; Wiegers, E.; Sewalt, C.; Buki, A.; Citerio, G.; De Keyser, V.; Ercole, A.; Kunzmann, K.; Lanyon, L.; Lecky, F.; et al. CENTER-TBI Participants and Investigators. Case-mix, care pathways, and outcomes in patients with traumatic brain injury in CENTER-TBI: A European prospective, multicentre, longitudinal, cohort study. Lancet Neurol. 2019, 18, 923–934. [Google Scholar] [CrossRef] [PubMed]
- Isah, M. Multisectorial Approach in Reducing Road Traffic Accidents in Cameroon. Nfafu Policy Institute. 2020. Available online: https://nkafu.org/multi-sectorial-approach-in-reducing-road-traffic-accidents-in-cameroon/ (accessed on 2 August 2023).
- Bezabeh, G.B.; Souare, M.; Oumarou, A. Road Safety in Africa Assessment of Progresses and Challenges in Road Safety Management System 2013; African Development Bank Group: Tunis, Tunisia, 2013. [Google Scholar]
- Kongnyuy, E.J.; Wiysonge, C.S. Alcohol use and extramarital sex among men in Cameroon. BMC Int. Health Hum. Rights 2007, 7, 6. [Google Scholar] [CrossRef]
- Wakabayashi, M.; McKetin, R.; Banwell, C.; Yiengprugsawan, V.; Kelly, M.; Seubsman, S.-A.; Iso, H.; Sleigh, A.; Thai Cohort Study Team. Alcohol consumption patterns in Thailand and their relationship with non-communicable disease. BMC Public Health 2015, 15, 1297. [Google Scholar] [CrossRef] [PubMed]
- Pawłowski, W.; Lasota, D.; Goniewicz, M.; Rzońca, P.; Goniewicz, K.; Krajewski, P. The Effect of Ethyl Alcohol upon Pedestrian Trauma Sustained in Traffic Crashes. Int. J. Environ. Res. Public Health 2019, 16, 1471. [Google Scholar] [CrossRef] [PubMed]
- Landes, M.; Venugopal, R.; Berman, S.; Heffernan, S.; Maskalyk, J.; Azazh, A. Epidemiology, clinical characteristics and outcomes of head injured patients in an Ethiopian emergency centre. Afr. J. Emerg. Med. 2017, 7, 130–134. [Google Scholar] [CrossRef]
- Tesfay, M. Clinical Profile and Outcome of Traumatic Brain Injury Patients at the Emergency Department of AaBET Hospital. Master’s Thesis, College of Health Science, Addis Ababa University, Addis Ababa, Ethiopia, 2020. [Google Scholar]
- Foster, M.; Tilse, C. Referral to rehabilitation following traumatic brain injury: A model for understanding inequities in access. Soc. Sci. Med. 2003, 56, 2201–2210. [Google Scholar] [CrossRef]
- Hellweg, S.; Johannes, S. Physiotherapy after traumatic brain injury: A systematic review of the literature. Brain Inj. 2008, 22, 365–373. [Google Scholar] [CrossRef]
- Lendraitienė, E.; Petruševičienė, D.; Savickas, R.; Žemaitienė, I.; Mingaila, S. The impact of physical therapy in patients with severe traumatic brain injury during acute and post-acute rehabilitation according to coma duration. J. Phys. Ther. Sci. 2016, 28, 2048–2054. [Google Scholar] [CrossRef]
- John Hopkins Medicine. Rehabilitation after Traumatic Brain Injury. 2023. Available online: https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/rehabilitation-after-traumatic-brain-injury (accessed on 2 August 2023).
- Kim, Y.J. The Impact of Time from ED Arrival to Surgery on Mortality and Hospital Length of Stay in Patients with Traumatic Brain Injury. J. Emerg. Nurs. 2011, 37, 328–333. [Google Scholar] [CrossRef]
- de Guise, E.; LeBlanc, J.; Dagher, J.; Tinawi, S.; Lamoureux, J.; Marcoux, J.; Maleki, M.; Feyz, M. Characteristics of patients with acute traumatic brain injury discharged against medical advice in a Level 1 urban trauma centre. Brain Inj. 2014, 28, 1288–1294. [Google Scholar] [CrossRef]
- Marcoux, J.; Alkutbi, M.; Lamoureux, J.; Feyz, M.; Saluja, R.S.; de Guise, E. Discharge against Medical Advice in Traumatic Brain Injury: Follow-Up and Readmission Rate. Can. J. Neurol. Sci. 2017, 44, 311–317. [Google Scholar] [CrossRef]
- Kalogriopoulos, N.A.; Baran, J.; Nimunkar, A.J.; Webstar, J.G. Electronic Medical Record Systems for Developing Countries: Review. In Proceedings of the 2009 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Minneapolis, MN, USA, 3–6 September 2009; pp. 1730–1733. Available online: https://ewh.slc.engr.wisc.edu/publications/conferences/2009/IEEEEMBC/KalogriopoulosNWMedRSIEEEMBC2009.pdf (accessed on 26 August 2023).
- Ramakrishnan, N.; Ranganathan, L.; Abraham, B.K.; Rajagopalan, S.; Venkataraman, R. What Happens to Patients Discharged Against Medical Advice? Indian J. Crit. Care Med. 2018, 22, 580–584. [Google Scholar]
- Albayati, A.; Douedi, S.; Alshami, A.; Hossain, M.A.; Sen, S.; Buccellato, V.; Cutroneo, A.; Beelitz, J.; Asif, A. Why Do Patients Leave against Medical Advice? Reasons, Consequences, Prevention, and Interventions. Healthcare 2021, 9, 111. [Google Scholar] [CrossRef] [PubMed]
- Pélieu, I.; Kull, C.; Walder, B. Prehospital and Emergency Care in Adult Patients with Acute Traumatic Brain Injury. Med. Sci. 2019, 7, 12. [Google Scholar] [CrossRef]
- Gao, G.; Wu, X.; Feng, J.; Hui, J.; Mao, Q.; Lecky, F.; Lingsma, H.; Maas, A.I.R.; Jiang, J. Clinical characteristics and outcomes in patients with traumatic brain injury in China: A prospective, multicentre, longitudinal, observational study. Lancet Neurol. 2020, 19, 670–677. [Google Scholar] [CrossRef] [PubMed]
- Lu, J.; Marmarou, A.; Choi, S.; Maas, A.; Murray, G.; Steyerberg, E.W. Impact and Abic Study Group. Mortality from traumatic brain injury. Acta Neurochir. 2005, 95, 281–285. [Google Scholar]
- Buh, F.C.; Hutchinson, P.J.A.; Anwar, F. Early neuro-rehabilitation in traumatic brain injury: The need for an African perspective. BMC Med. 2023, 21, 290. [Google Scholar] [CrossRef]
- Ruet, A.; Bayen, E.; Jourdan, C.; Ghout, I.; Meaude, L.; Lalanne, A.; Pradat-Diehl, P.; Nelson, G.; Charanton, J.; Aegerter, P.; et al. A Detailed Overview of Long-Term Outcomes in Severe Traumatic Brain Injury Eight Years Post-injury. Front. Neurol. 2019, 10, 120. [Google Scholar] [CrossRef]
- Born, K.; Amsler, F.; Gross, T. Prospective evaluation of the Quality of Life after Brain Injury (QOLIBRI) score: Minor differences in patients with major versus no or mild traumatic brain injury at one-year follow up. Heal. Qual. Life Outcomes 2018, 16, 136. [Google Scholar] [CrossRef]
| Characteristic | N = 160 |
|---|---|
| Age, Median (IQR) | 32 (IQR26, 39) |
| [<15] | 6 (3.8%) |
| [15–45] | 125 (78%) |
| [46–65] | 22 (14%) |
| [>65] | 7 (4.4%) |
| Gender | |
| Female | 16 (10%) |
| Male | 144 (90%) |
| Education | |
| Graduated | 19 (12%) |
| Illiterate | 9 (5.6%) |
| Matriculated | 7 (4.4%) |
| Post-graduate | 1 (0.6%) |
| Primary | 40 (25%) |
| Secondary | 82 (51%) |
| Not Known | 2 (1.2%) |
| Profession | |
| Employee in service | 30 (19%) |
| Manual workers | 24 (15%) |
| Bike riders | 43 (27%) |
| Student | 16 (10%) |
| Unemployed | 21 (13%) |
| Others | 26 (16%) |
| Marital status | |
| Married | 67 (42%) |
| Not applicable | 6 (3.8%) |
| Single | 87 (54.4%) |
| Religion | |
| Christian | 122 (80.3%) |
| Muslim | 28 (18%) |
| Other | 2 (1.3%) |
| Missing | 8 |
| Driving license? | |
| Yes | 11 (12.2%) |
| No license | 73 (81%) |
| Not applicable | 70 (44%) |
| Unknown | 6 (6.7%) |
| Income rate per month in Central African FCFA (USD) | N = 130 |
| <50,000 (<$78) | 26 (20%) |
| 50,001–150,000 ($78–$234) | 84 (65%) |
| 150,001–200,000 ($235–$312) | 14 (11%) |
| 200,001–300,000 ($313–$468) | 2 (2%) |
| >300,000 (>$468) | 4 (3%) |
| Not applicable | 30 (19%) |
| Medico-social history | |
| Diabetes | 2 (1.2%) |
| Hypertension | 14 (8.8%) |
| Smoking | 22 (14%) |
| Alcohol | 97 (61%) |
| Characteristic | N = 160 |
|---|---|
| Clinical details | |
| Loss of consciousness | 152 (95%) |
| Vomiting | 55 (34%) |
| Nausea | 21 (13%) |
| Ear bleed | 20 (12%) |
| Nasal bleed | 43 (27%) |
| Headache | 103 (64%) |
| Seizure | 7 (4.4%) |
| Agitation | 43 (27%) |
| Median heart rate | 88 (78, 99) |
| Blood pressure | N = 160 |
| Elevated | 15 (9.4%) |
| Hypertension | 62 (39%) |
| Hypotension | 19 (12%) |
| Normal | 64 (40%) |
| temperature | N = 144 |
| Hypothermia | 3 (2.1%) |
| Normal | 131 (91%) |
| Elevated | 10 (6.9%) |
| Missing | 16 |
| Pupil reactivity | |
| Both pupils reactive | 145 (91%) |
| No pupil reactive | 5 (3.1%) |
| One pupil reactive | 10 (6.2%) |
| Median Glasgow Coma Scale | 12.0 (8.0, 14.0) |
| Eye opening | |
| 1 | 29 (18%) |
| 2 | 23 (14%) |
| 3 | 49 (31%) |
| 4 | 59 (37%) |
| Verbal response | |
| 1 | 34 (21%) |
| 2 | 18 (11%) |
| 3 | 25 (16%) |
| 4 | 46 (29%) |
| 5 | 37 (23%) |
| Motor response | |
| 1 | 4 (2.5%) |
| 2 | 4 (2.5%) |
| 3 | 8 (5.0%) |
| 4 | 22 (14%) |
| 5 | 45 (28%) |
| 6 | 77 (48%) |
| Influence of alcohol | |
| None | 108 (68%) |
| Suspected | 33 (21%) |
| Unknown | 19 (12%) |
| Characteristic | N = 160 |
|---|---|
| Cause of injury | 160 |
| Assault/violence | 12 (7.5%) |
| Fall | 8 (5.0%) |
| Road traffic incident | 136 (85%) |
| Other Causes | 4 (2.5%) |
| Road traffic collision type | 136 |
| Pedestrian | 31 (23%) |
| RTC car (passenger) | 7 (5.2%) |
| RTC cyclist | 1 (0.7%) |
| RTC driver | 2 (1.5%) |
| RTC Motorcyclist | 81 (60%) |
| RTC Motorcyclist (passenger) | 11 (8.1%) |
| RTC other type of vehicle (driver) | 1 (0.7%) |
| Other | 1 (0.1%) |
| Fall type | N = 8 |
| Fall from height | 6 (75%) |
| Fall standing height | 2 (25%) |
| Assault type | N = 12 |
| Assault (without a weapon) | 3 (25%) |
| Assault blunt instrument | 5 (42%) |
| Assault knife/Machete | 4 (33%) |
| Domestic violence | N = 3 |
| Assault (without a weapon) | 2 (67%) |
| Assault blunt instrument | 1 (33%) |
| Other causes | N = 3 |
| Hit by falling object | 1 (33%) |
| Industrial accident | 2 (67%) |
| Mechanism of injury | 160 |
| Bicycle accident | 1 (0.6%) |
| Fall from a higher lever | 6 (3.4%) |
| Fall from the same level | 5 (3.1%) |
| Hit by a blunt object | 6 (3.4%) |
| Knife/machete | 4 (2.5%) |
| Motor vehicle accident | 23 (14.4%) |
| Motorcycle accident | 111 (69.4%) |
| Other | 4 (2.5%) |
| If other, specify | |
| Blow | 1 (25%) |
| hit by falling object | 2 (50%) |
| occupational accident | 1 (25%) |
| Characteristic | N = 160 |
|---|---|
| Referral details | |
| Direct referral | 65 (41%) |
| Indirect referral | 95 (59%) |
| If direct referral, Means of transport | |
| Ambulance | 1 (1.6%) |
| Moto taxi | 7 (11%) |
| Private vehicle | 10 (16%) |
| Taxi | 45 (67%) |
| Other | 2 (3.3%) |
| Transport from other health centre to trauma centre | 95 |
| Ambulance | 14 (15%) |
| Moto taxi | 5 (5%) |
| Private vehicle | 15 (16%) |
| Taxi | 60 (63%) |
| Other | 1 (1.0%) |
| General means of transport | N = 160 |
| Medical means | 15 (9%) |
| Non-medical means | 145 (91%) |
| If Ambulance, | 14 |
| Physician present? | N = 14 |
| No | 12 (85.7%) |
| Yes | 2 (14.3%) |
| Vital monitoring | 12 (85.7%) |
| Fluid administration | 0 (0%) |
| Airway protection | 7 (50%) |
| Drug administration | 0 (00%) |
| Transport position | 160 |
| Side lying | 28 (18%) |
| Sitting | 44 (28%) |
| Supine | 88 (55%) |
| Time difference between injury and arrival at the referral hospital | |
| <1 h | 39 (24%) |
| 1–4 h | 71 (44%) |
| 4.1–11 h | 30 (19%) |
| 11–24 | 20 (12%) |
| Characteristic | N = 160 |
|---|---|
| Poly-trauma | 19 (12%) |
| Isolated TBI | 141 (88%) |
| Classification of TBI | N = 160 |
| Mild | 66 (41%) |
| Moderate | 55 (34%) |
| Severe | 39 (24%) |
| CT not done | 35 (22%) |
| CT Scan asked, not done | 28 (80%) |
| No CT scan recommended | 7 (20%) |
| Reason why CT Scan not done | 28 |
| No finance | 26 (93%) |
| Other | 10 (36%) |
| If other, specify | 10 |
| moved to other hospital | 3 (22%) |
| not asked | 7 (78%) |
| Complementary exams done to characterize injury | N = 160 |
| CT Scan | 125 (78%) |
| If scan or MRI, traumatic abnormalities present | 77 (64%) |
| Fracture | N = 125 |
| Yes | 36 (30%) |
| Linear skull fracture | 20 (56%) |
| Depressed fracture | 22 (61%) |
| Basilar skull fracture | 19 (53%) |
| Type of TBI | N = 77 |
| Extradural hematoma | 22 (29%) |
| Acute subdural haemorrhage | 18 (23%) |
| Cerebral contusion | 25 (32%) |
| Cerebral oedema | 10 (13%) |
| Meningeal haemorrhage | 8 (10%) |
| Mass effect pressure | 3 (3.9%) |
| Intracerebral haemorrhage | 12 (16%) |
| Other type of TBI | 4 (5.2%) |
| Neurosurgery | N = 77 |
| Yes | 17 (22.1%) |
| No | 60 (77.9%) |
| Characteristic | N = 160 |
|---|---|
| Total hospital stay (days) | 4.0 (2.0, 6.8) |
| Post Op Stay (days) | 7 (4, 11) |
| Discharge destination | 138 |
| Discharge to home | 126 (91%) |
| Discharge to rehabilitation | 4 (3.0%) |
| Other hospital facility | 8 (5%) |
| Discharge against medical advice (DAMA) | 46 (33%) |
| Reason for DAMA | |
| Financial constraint | 46 (100%) |
| Traditional treatment | 8 (17.4%) |
| Readmission | 00 |
| Outcome at discharge | N = 160 |
| Disability rating scale | N = 138, 4 (1, 10) |
| Recovery status | N = 138 |
| Extreme vegetative state | 6 (4.3%) |
| vegetative state | 3 (2.2) |
| Extremely severe disability | 7 (5.0%) |
| Severe disability | 8 (5.8%) |
| Moderately severe | 26 (18.7%) |
| Moderate | 28 (20.1%) |
| Partial disability | 27 (19.4%) |
| Mild disability | 9 (6.5%) |
| Recovering | 25 (18%) |
| Mortality | 21 (13%) |
| Mortality according to TBI severity | |
| Mortality in mild TBI | 1 (4.8%) |
| Mortality in moderate TBI | 3 (14.3%) |
| Mortality in severe TBI | 17 (80.9%) |
| Time difference between injury and death (days) | 1.00 (1.00, 2.00) |
| (a) | |||
| Characteristic | N = 160 | ||
| 6-months outcome with GOSE | N = 152 | ||
| Death | 22 (14.5%) | ||
| GR− | 15 (9.9%) | ||
| GR+ | 44 (28.9%) | ||
| MD− | 23 (15.1%) | ||
| MD+ | 32 (21.1%) | ||
| SD− | 4 (2.6%) | ||
| SD+ | 12 (7.9%) | ||
| Overall | |||
| Death | 22 (14%) | ||
| Good recovery | 59 (39%) | ||
| Moderate disability | 55 (36%) | ||
| Severe disability | 16 (11%) | ||
| Missing | 8 | ||
| 6-months outcome with QoLIBRI | N = 130 | ||
| Impaired | 36 (28%) | ||
| Borderline | 14 (11%) | ||
| Normal | 34 (26%) | ||
| Above average | 46 (35%) | ||
| Mean final score | 71.8 (19) | ||
| Missing and death (08 and 22, respectively) | 30 | ||
| (b) | |||
| Characteristic | No N = 114 | Yes N = 46 | p-Value |
| GOSE | N = 90 | N = 40 | 0.6 |
| Favourable outcome | 79 (88%) | 34 (85%) | |
| Unfavourable outcome | 11 (12%) | 6 (15%) | |
| (Missing and death), respectively | 24 (3 and 21) | 6 (5 and 1) | |
| QoLIBRI | N = 89 | N = 41 | 0.019 * |
| Impaired | 20 (22%) | 16 (39%) | |
| Not impaired (borderline, normal, above average) | 69 (78%) | 25 (61%) | |
| Missing | 25 | 05 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buh, F.C.; Sumbele, I.U.N.; Maas, A.I.R.; Motah, M.; Pattisapu, J.V.; Youm, E.; Meh, B.K.; Kobeissy, F.H.; Wang, K.W.; Hutchinson, P.J.A.; et al. Traumatic Brain Injury in Cameroon: A Prospective Observational Study in a Level I Trauma Centre. Medicina 2023, 59, 1558. https://doi.org/10.3390/medicina59091558
Buh FC, Sumbele IUN, Maas AIR, Motah M, Pattisapu JV, Youm E, Meh BK, Kobeissy FH, Wang KW, Hutchinson PJA, et al. Traumatic Brain Injury in Cameroon: A Prospective Observational Study in a Level I Trauma Centre. Medicina. 2023; 59(9):1558. https://doi.org/10.3390/medicina59091558
Chicago/Turabian StyleBuh, Franklin Chu, Irene Ule Ngole Sumbele, Andrew I. R. Maas, Mathieu Motah, Jogi V. Pattisapu, Eric Youm, Basil Kum Meh, Firas H. Kobeissy, Kevin W. Wang, Peter J. A. Hutchinson, and et al. 2023. "Traumatic Brain Injury in Cameroon: A Prospective Observational Study in a Level I Trauma Centre" Medicina 59, no. 9: 1558. https://doi.org/10.3390/medicina59091558
APA StyleBuh, F. C., Sumbele, I. U. N., Maas, A. I. R., Motah, M., Pattisapu, J. V., Youm, E., Meh, B. K., Kobeissy, F. H., Wang, K. W., Hutchinson, P. J. A., & Taiwe, G. S. (2023). Traumatic Brain Injury in Cameroon: A Prospective Observational Study in a Level I Trauma Centre. Medicina, 59(9), 1558. https://doi.org/10.3390/medicina59091558








